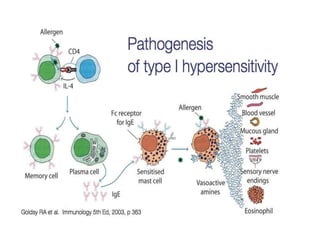
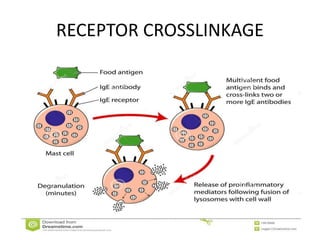
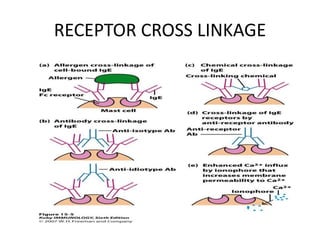
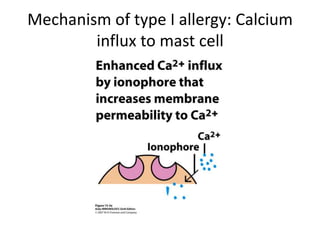
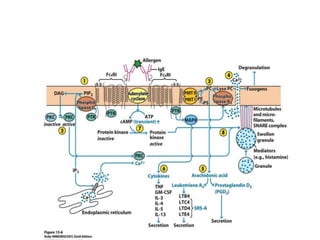
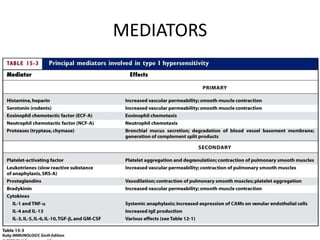
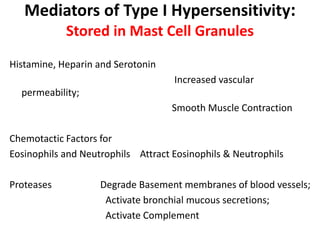
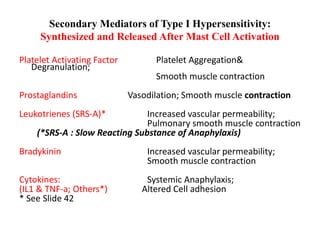
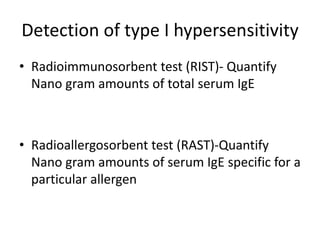
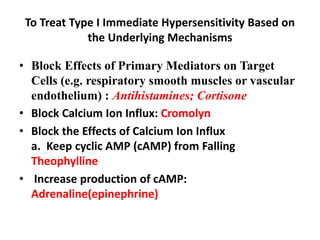
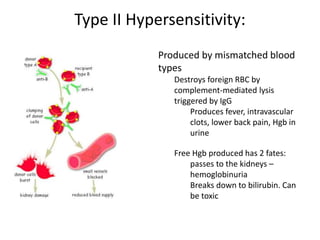
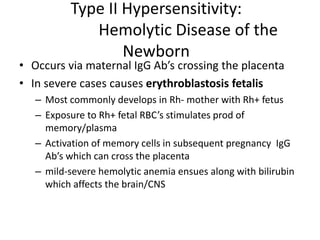
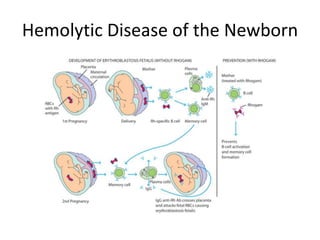
This document discusses hypersensitivity reactions of types I and II. It defines hypersensitivity as undesirable immune responses that can cause tissue damage or death. Type I reactions are immediate and IgE-mediated, involving mast cell degranulation. Common allergens are listed. Type II reactions are antibody-mediated and cytotoxic, destroying cells through complement activation or antibody-dependent cellular cytotoxicity. Examples given include blood transfusion reactions and hemolytic disease of the newborn. The mechanisms, mediators, treatments, and tests related to types I and II hypersensitivity reactions are described in detail.