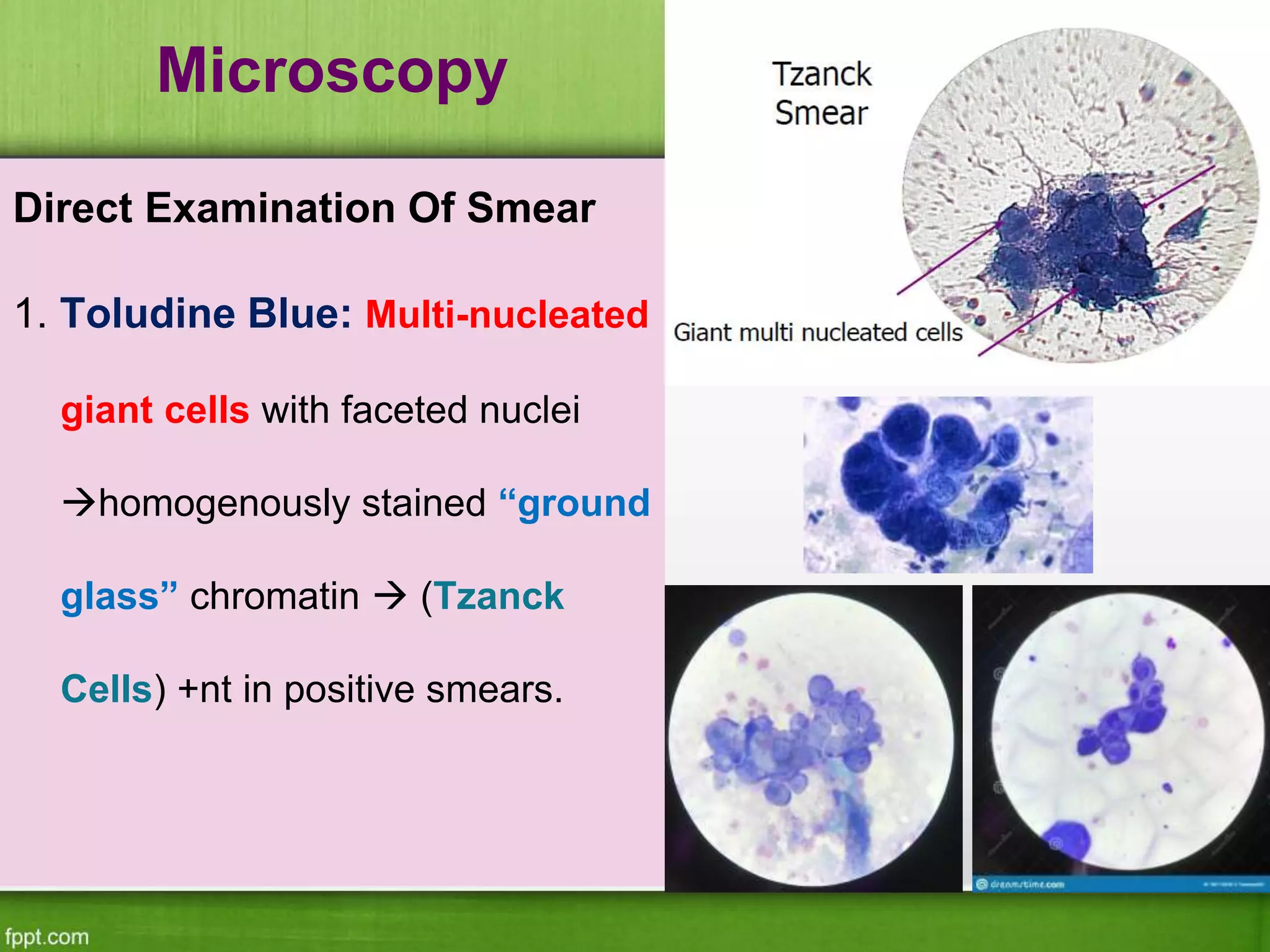
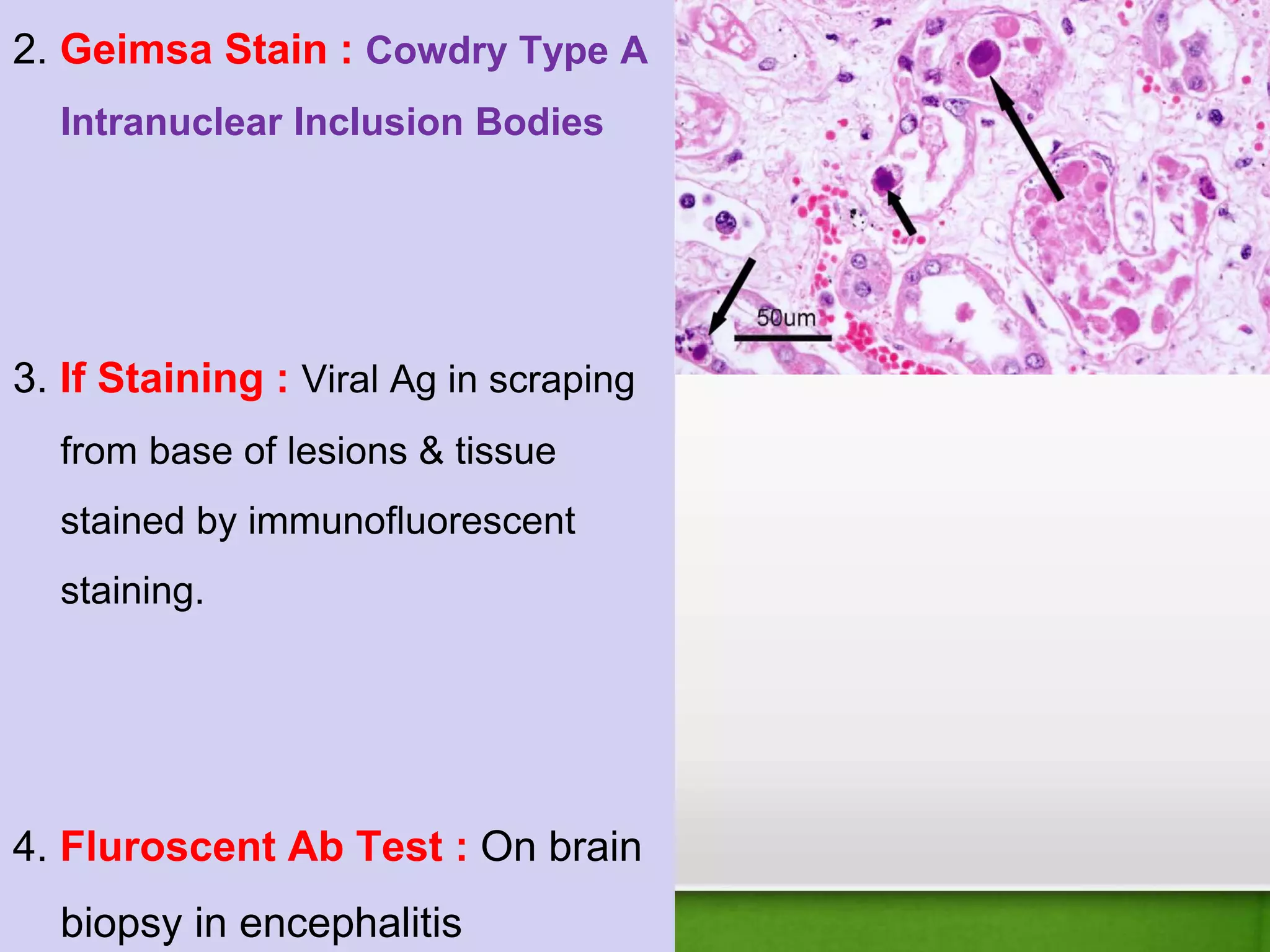
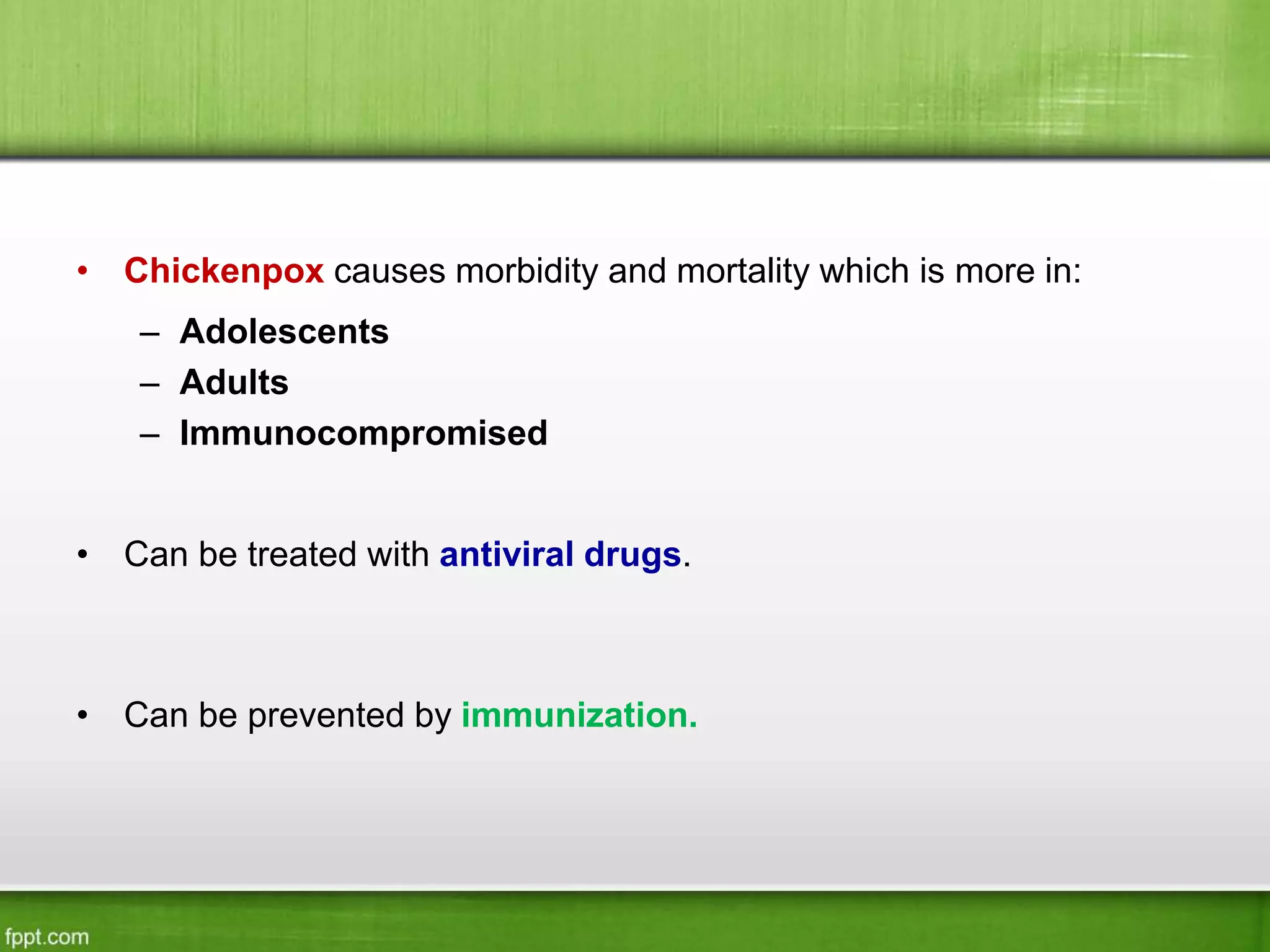
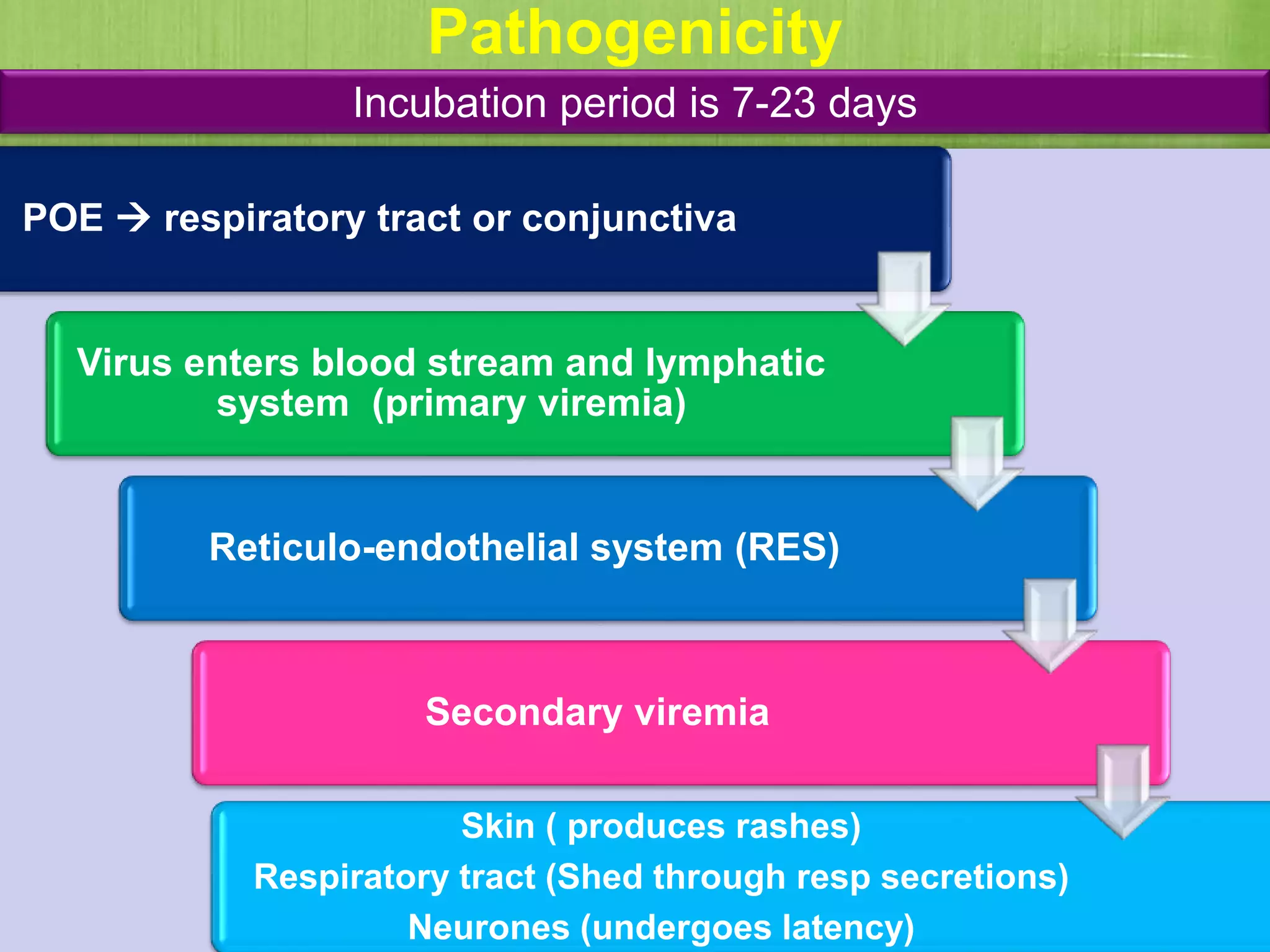
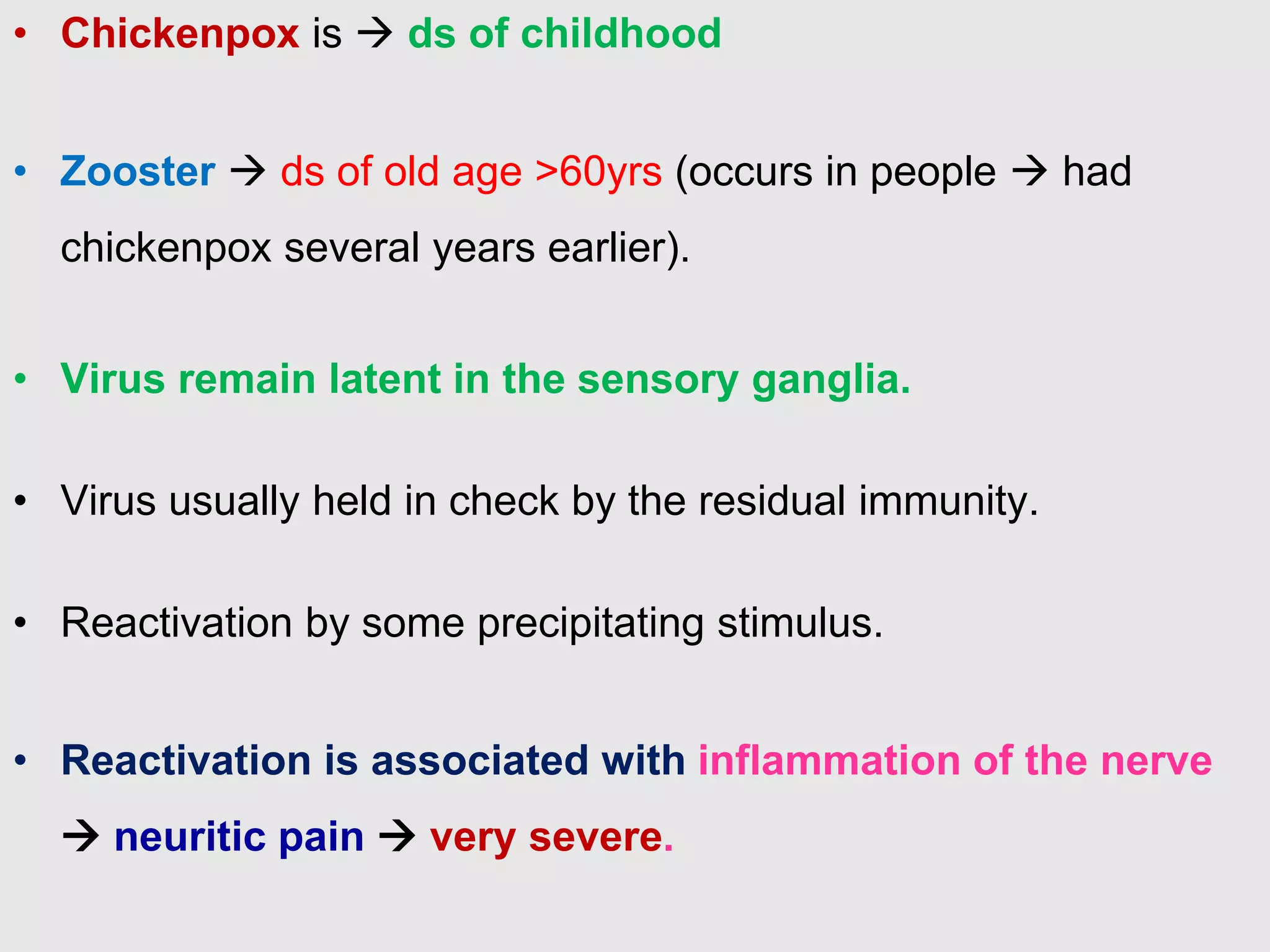
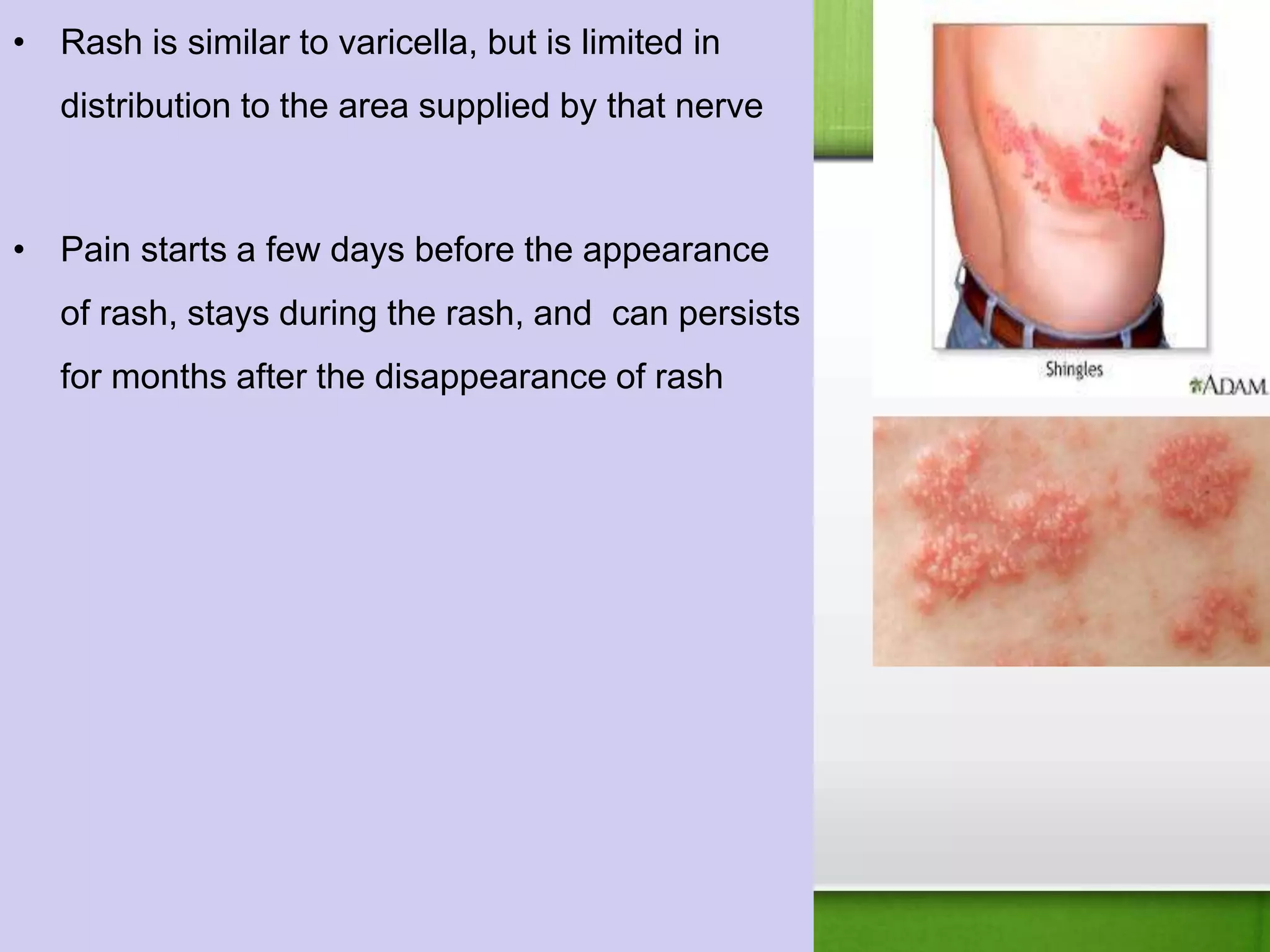
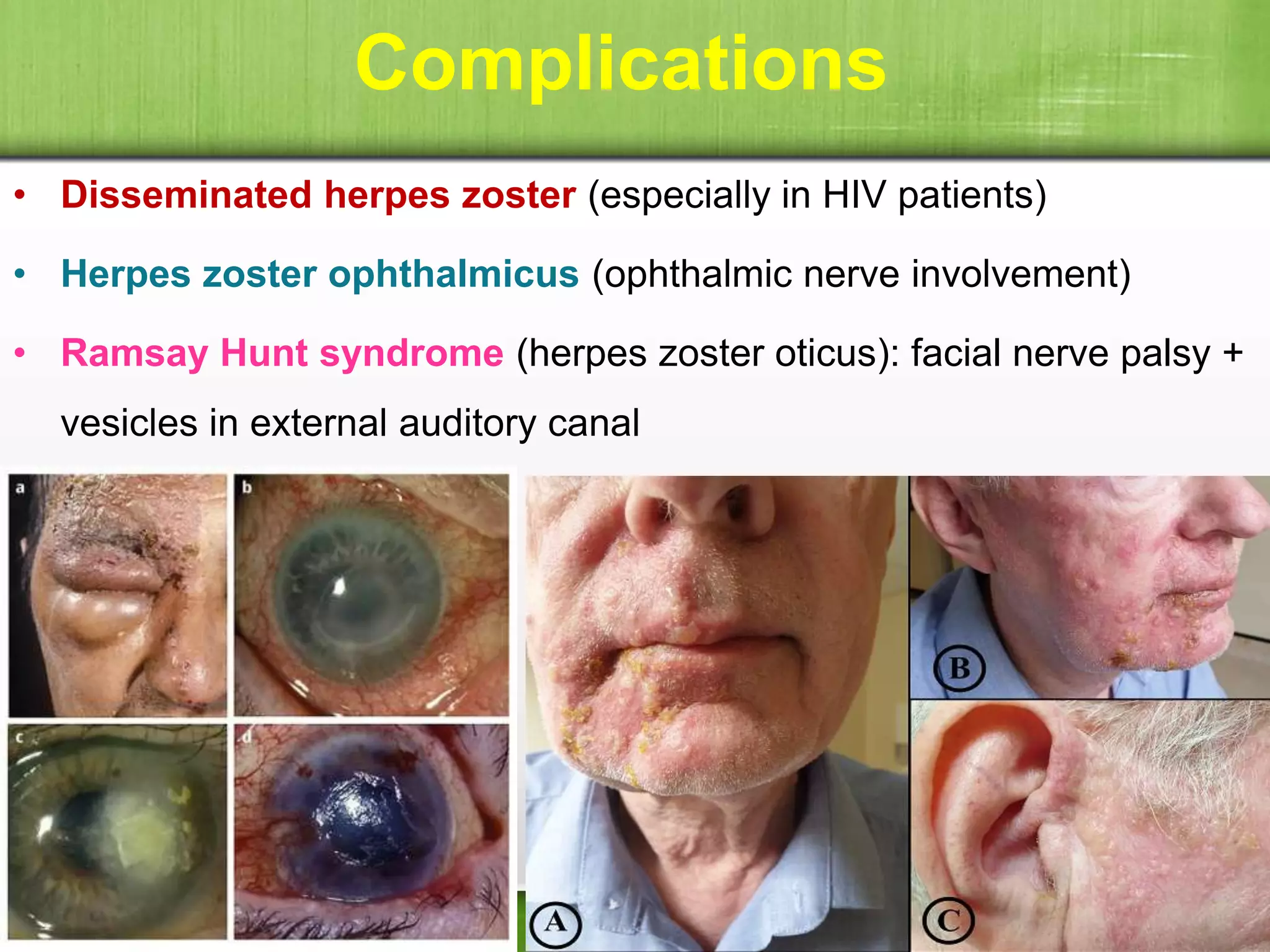
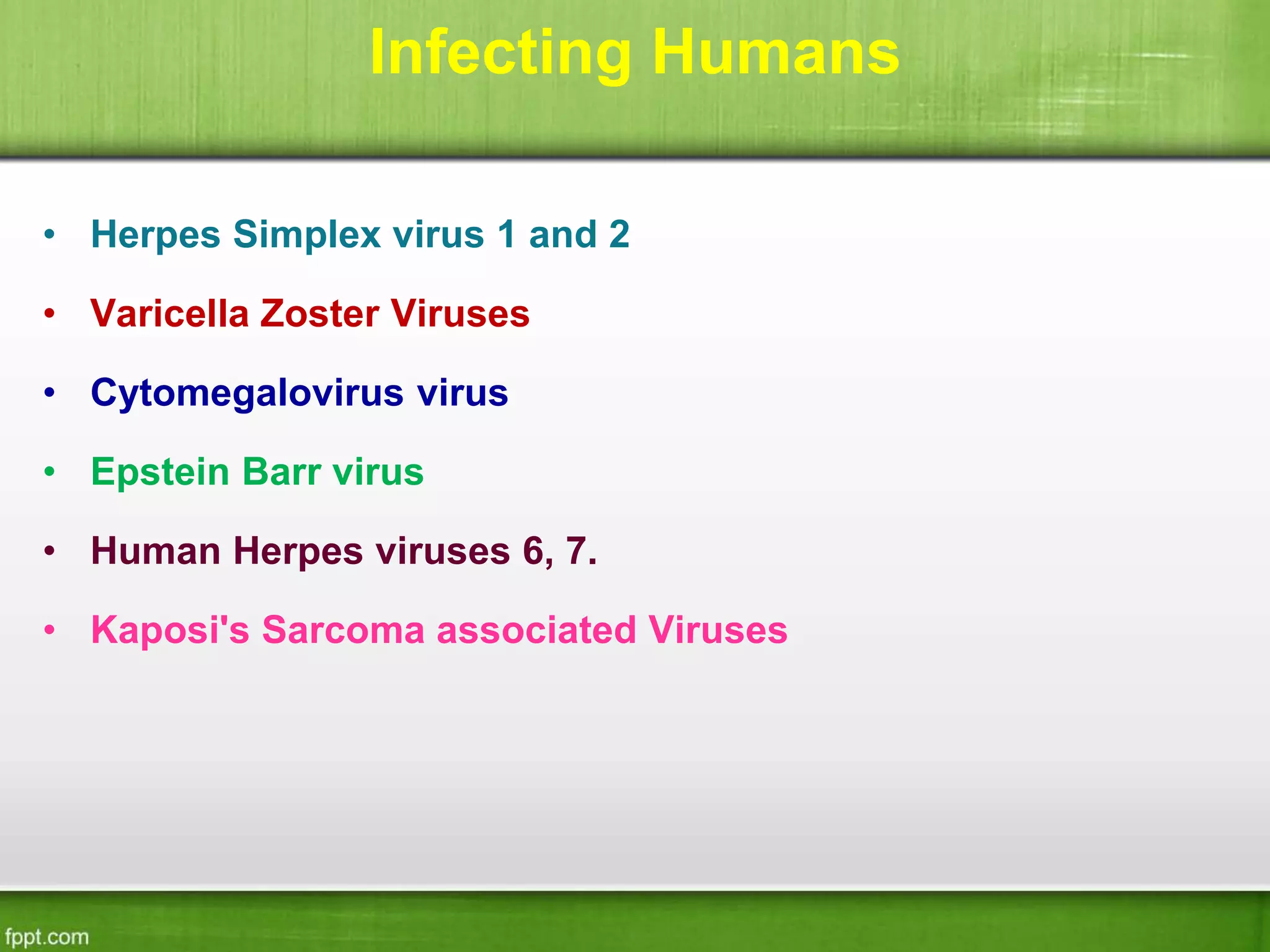
HSV are DNA viruses that establish latent infections in hosts. There are 8 human herpesviruses including HSV-1, HSV-2, VZV, CMV, EBV, and HHV-6/7/8. HSV-1 typically causes oral lesions while HSV-2 typically causes genital lesions. VZV causes chickenpox during primary infection and shingles during reactivation from latency in nerve ganglia. These viruses are diagnosed via microscopy, antigen/DNA detection, virus isolation, and serology. Antivirals like acyclovir are used to treat infections while vaccination can prevent chickenpox and shingles.



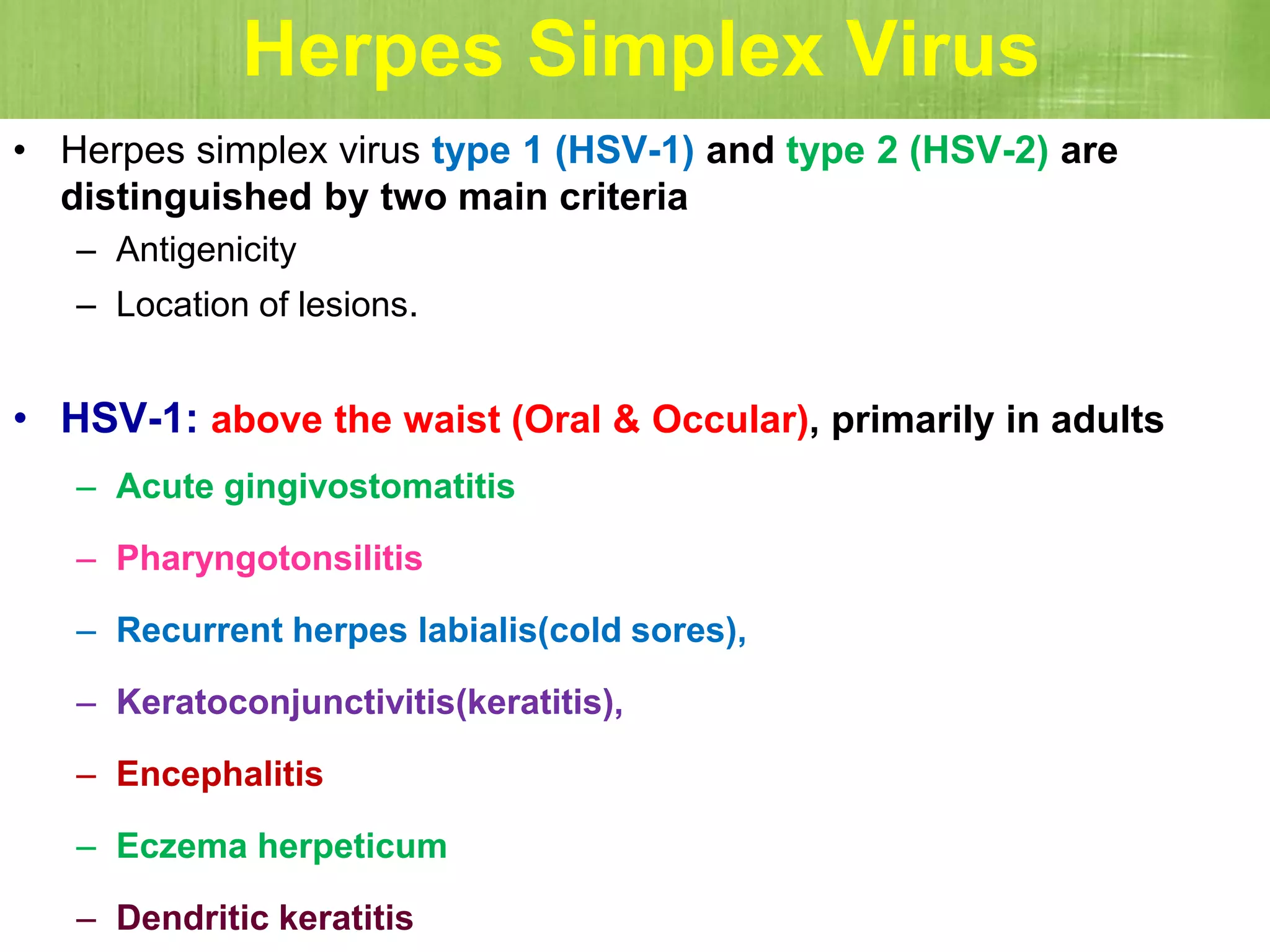








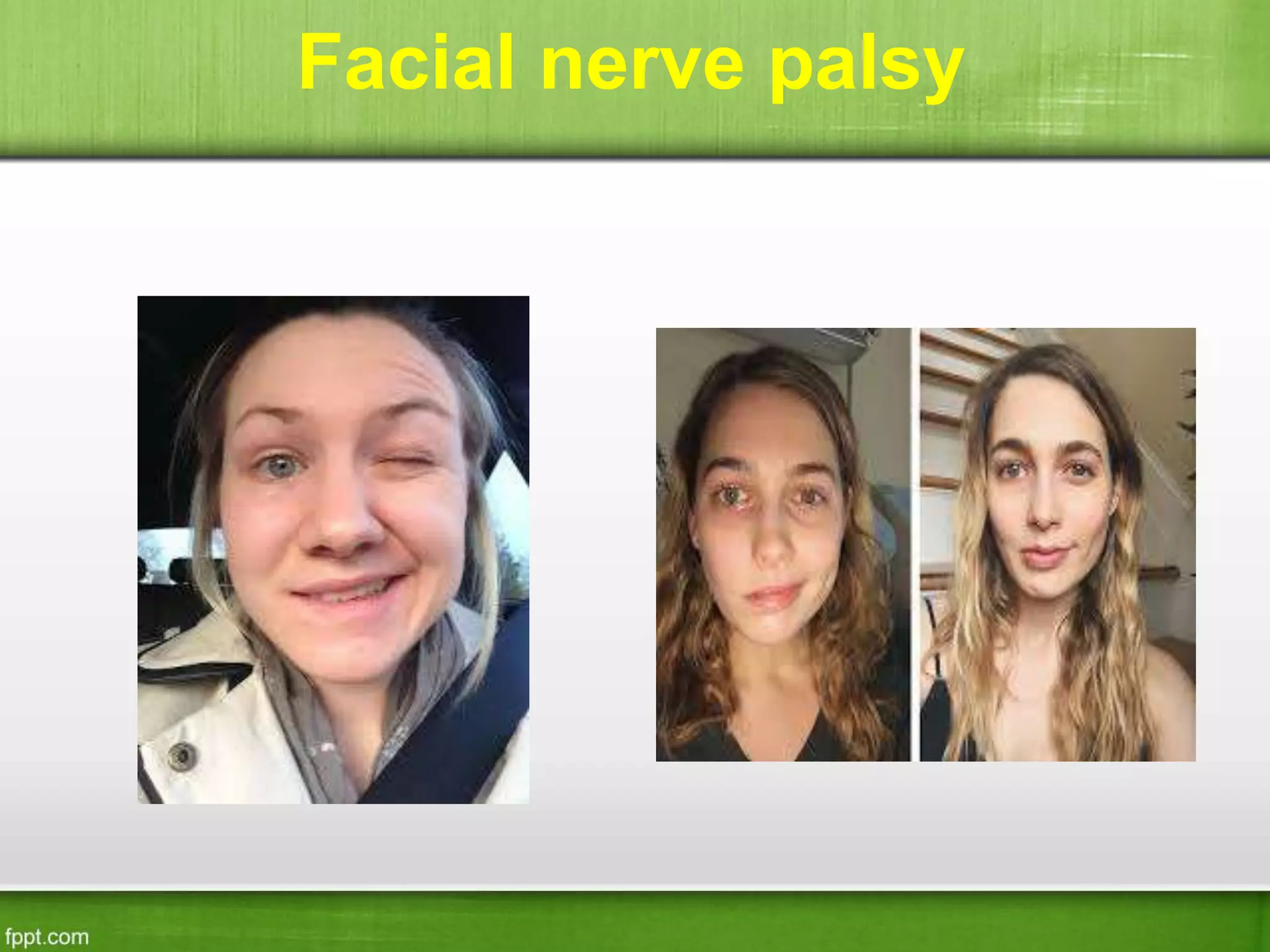
![Nervous system
• HSV encephalitis [rare]
• HSV meningitis
• Transverse myelitis [rare]
• Sacral autonomic dysfunction
• Guillian Barre syndrome [rare]
• Bell’s palsy [rare]](https://image.slidesharecdn.com/herpesvirusandvaricella-221203063807-e3f4f814/75/Herpes-Virus-and-Varicella-19-2048.jpg)
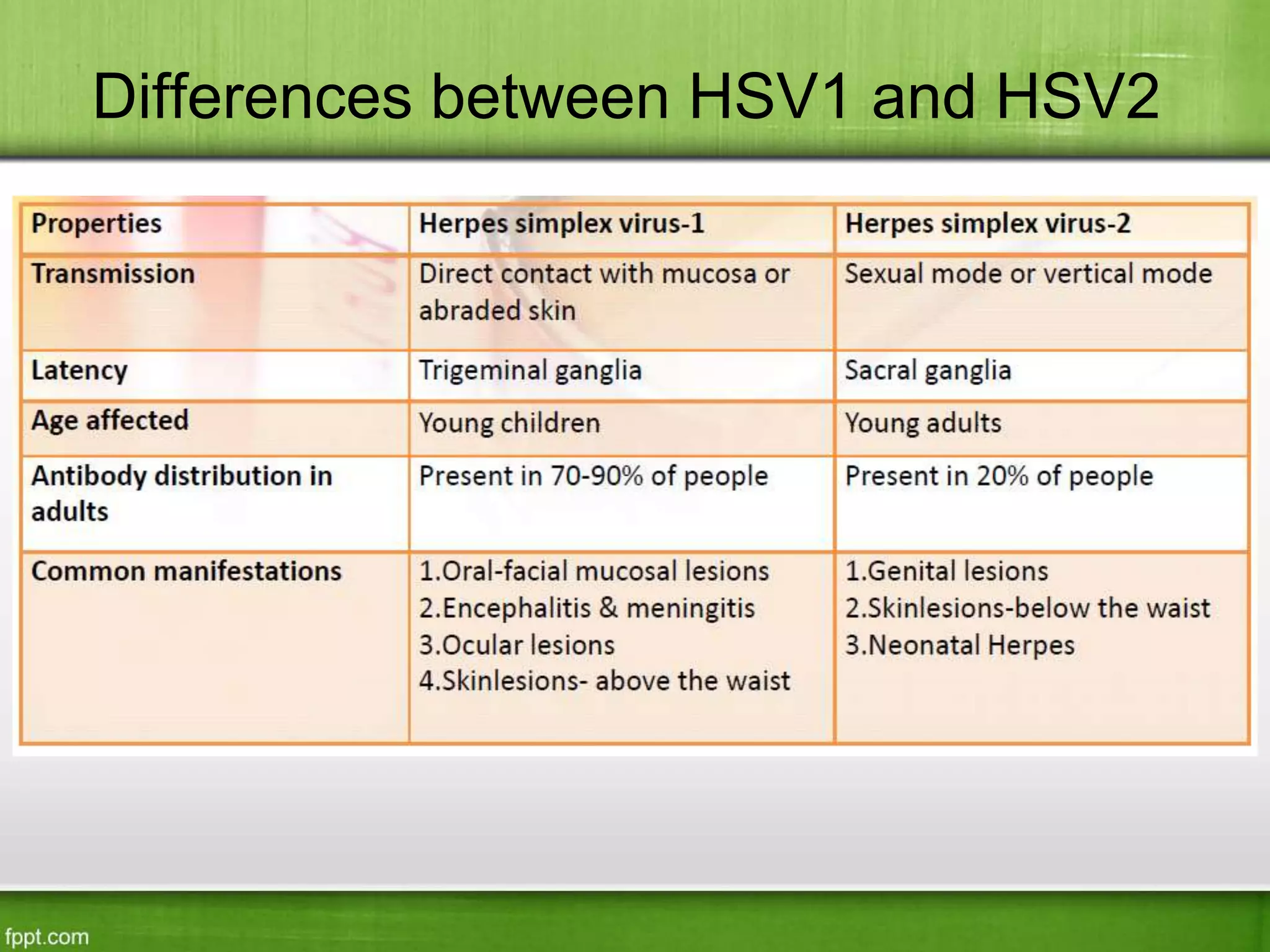
![Visceral
• HSV esophagitis
• Tracheobronchitis & Pneumonitis
• Hepatitis [uncommon]
• Disseminated HSV infection](https://image.slidesharecdn.com/herpesvirusandvaricella-221203063807-e3f4f814/75/Herpes-Virus-and-Varicella-20-2048.jpg)