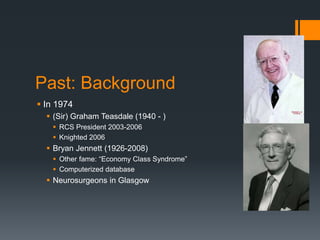
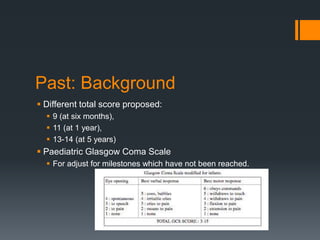
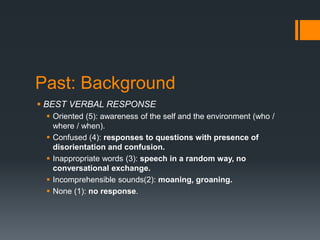
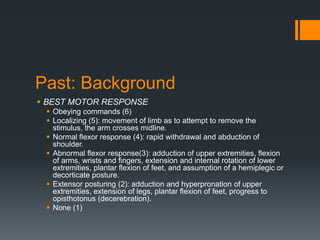
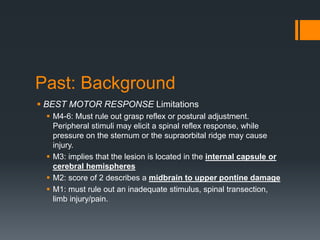
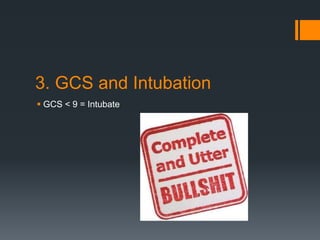
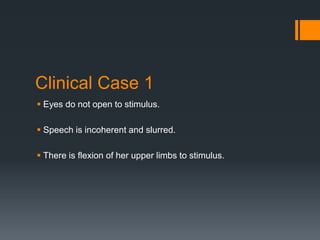
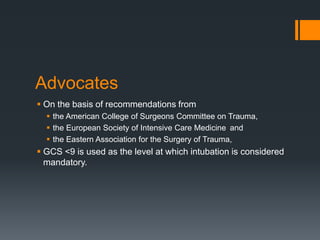
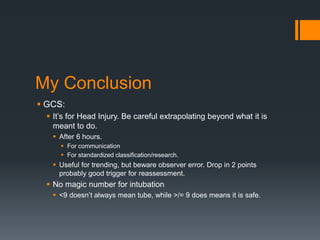
The Glasgow Coma Scale (GCS) was developed in 1974 to provide a standardized assessment of consciousness and brain injury severity, particularly after head trauma. While GCS is widely used and has had significant influence, its ability to predict outcomes and guide clinical decisions like intubation has limitations due to observer bias and variable scoring interpretations. The future of GCS assessment remains uncertain and should be carefully applied, particularly outside its intended use for head injuries.