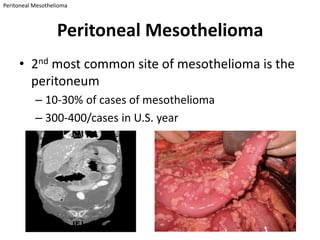
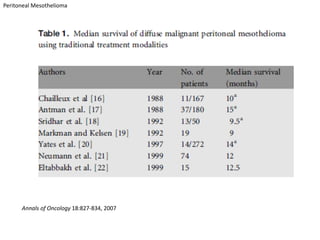
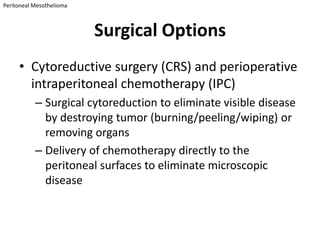
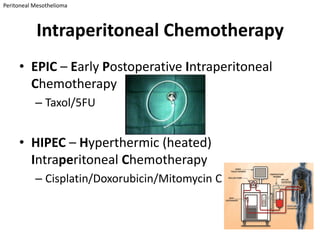
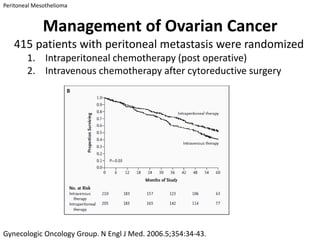
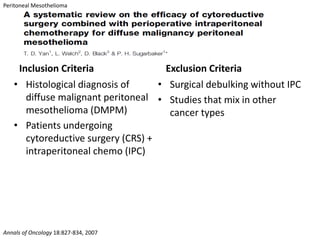
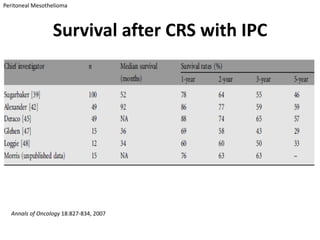
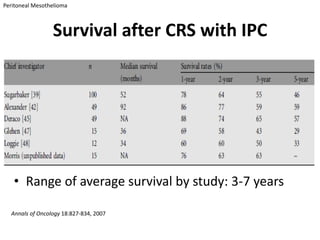
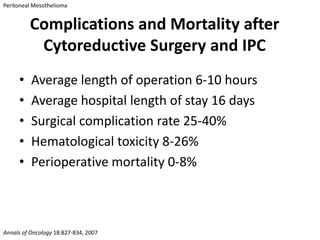
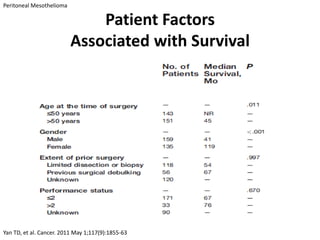
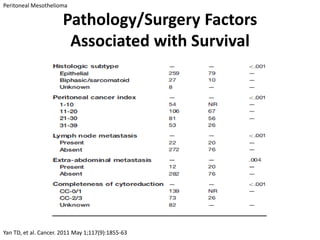
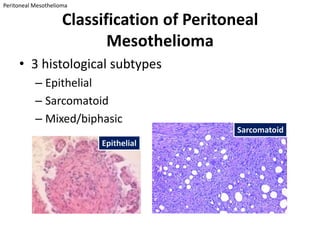
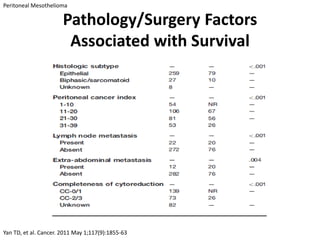
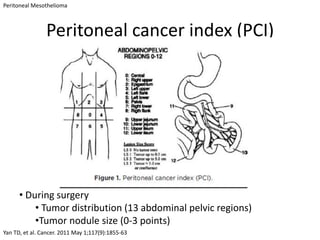
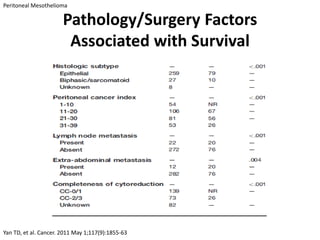
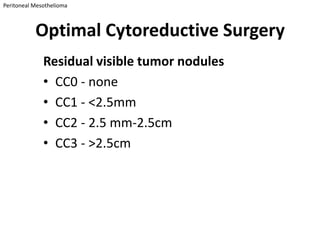
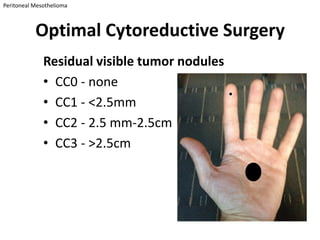
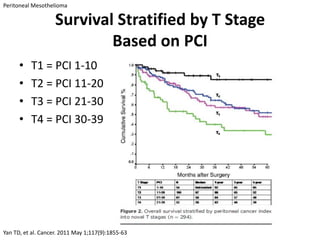
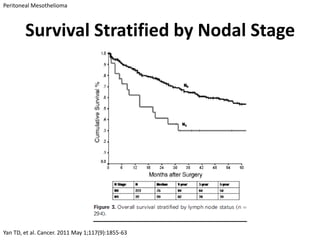
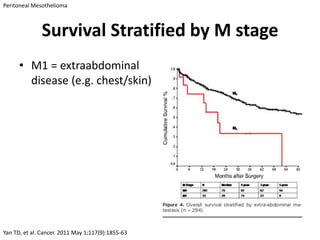
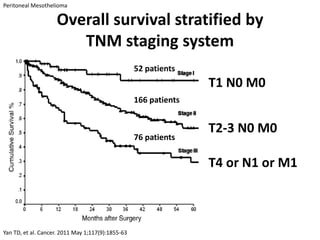
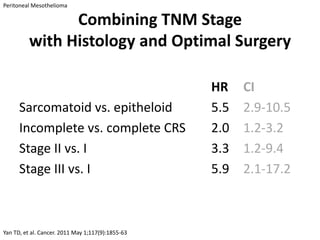
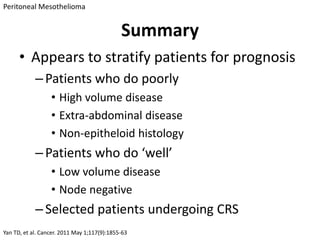
The document discusses peritoneal mesothelioma, focusing on its surgical options, treatment outcomes, and prognosis. It highlights cytoreductive surgery combined with intraperitoneal chemotherapy as a promising treatment, with survival rates ranging from 3 to 7 years. Factors influencing prognosis include tumor volume, histology, and the presence of extra-abdominal disease.