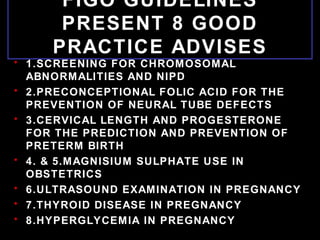
International Federation of Gynecology and Obstetrics Working Group on Best Practice on Maternal-Fetal Medicine presents 8 guidelines for good practice:
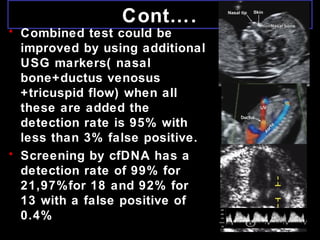
1) Screening for chromosomal abnormalities and NIPT, recommending first line screening be by combined test and that cfDNA be offered in combination with combined test from 11-13 weeks.
2) Preconceptional folic acid for prevention of neural tube defects, recommending all women of childbearing age take 400ug daily.
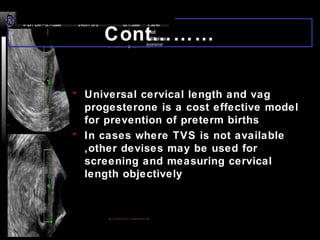
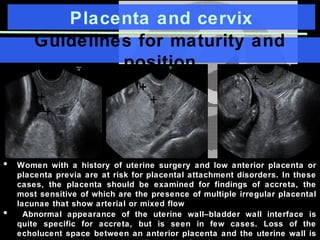
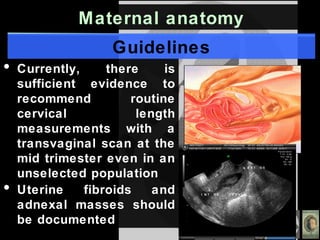
3) Cervical length screening and progesterone for prediction and prevention of preterm birth, recommending universal cervical length screening at 19-23 weeks and progesterone for women with short cervix.