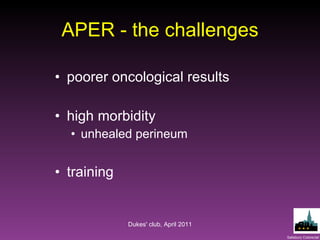
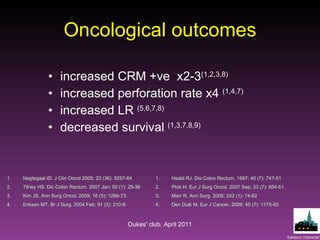
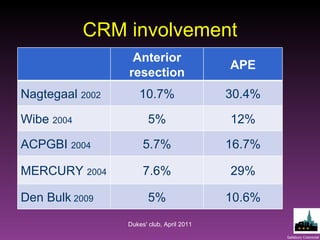
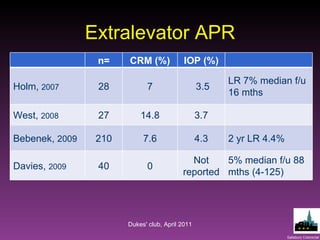
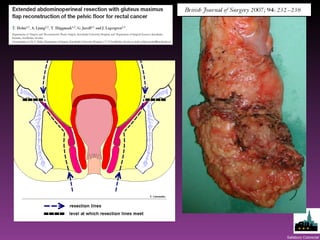
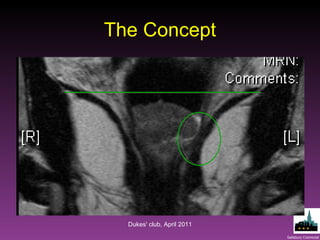
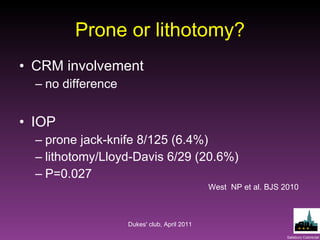
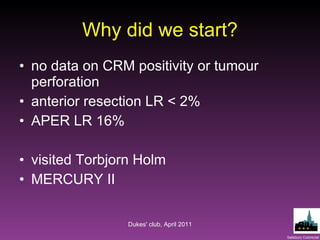
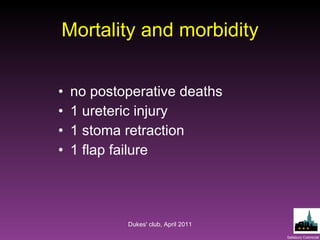
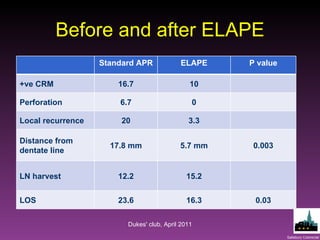
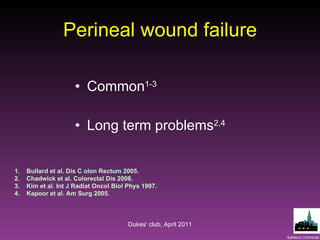
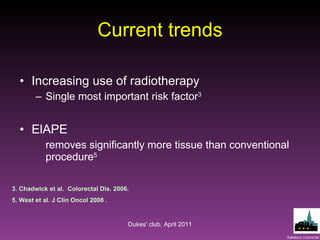
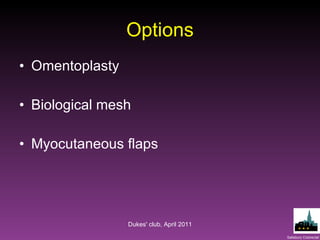
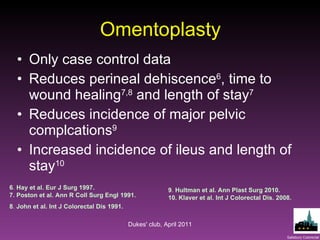
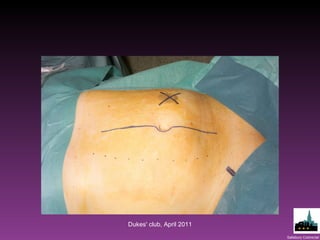
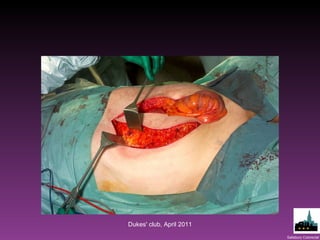
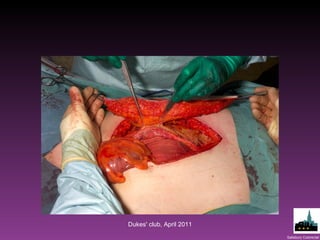
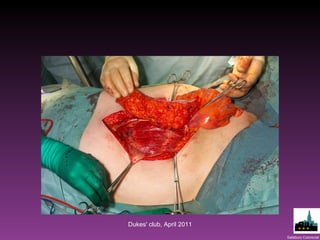
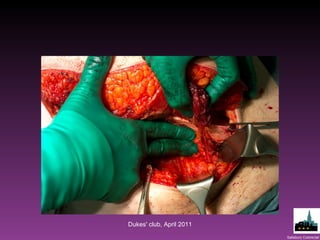
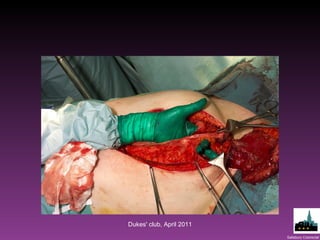
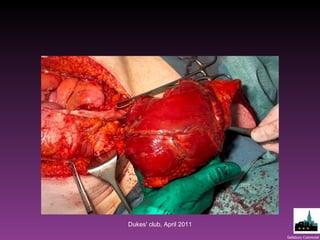
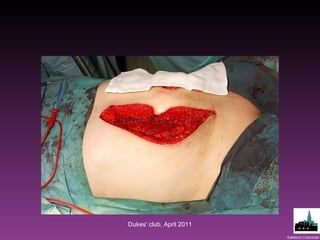
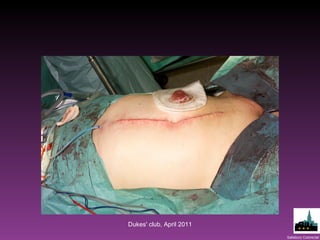
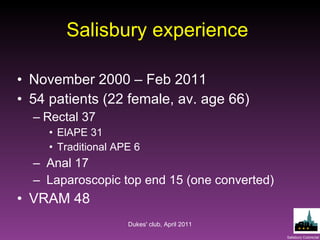
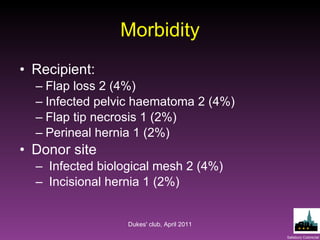
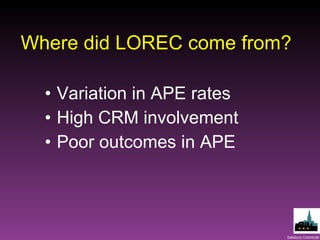
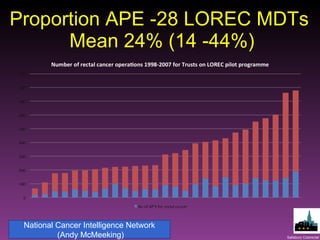
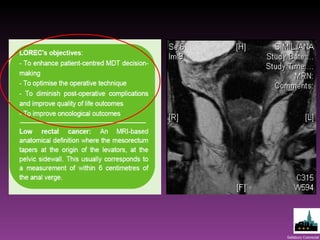
The document discusses surgical outcomes related to colorectal procedures, specifically addressing the challenges and morbidity associated with abdominoperineal excision (APE) and the benefits of extralevator APE (ELAPE). It details the impacts on circumferential resection margin (CRM) positivity, local recurrence rates, and wound healing techniques, suggesting that biological meshes and myocutaneous flaps are beneficial adjuncts for closure. The document emphasizes the need for comparative data to evaluate different surgical methods and improve patient outcomes.