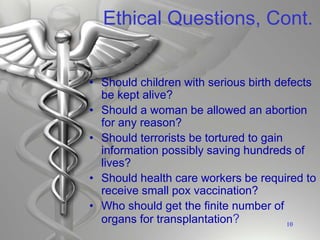
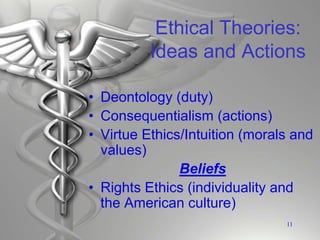
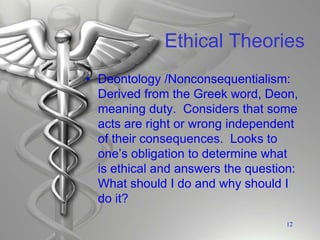
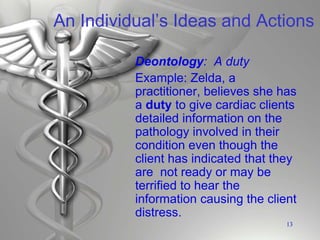
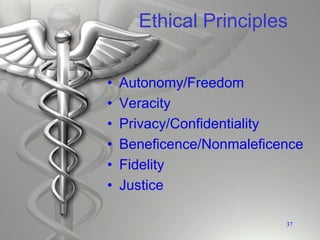
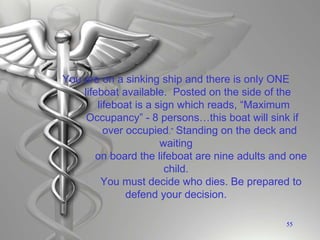
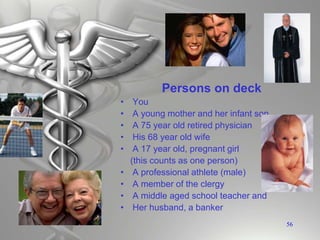
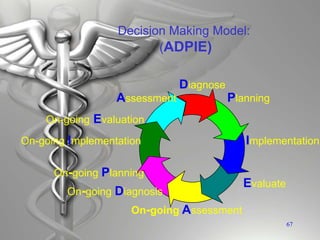
This document provides an overview of key concepts in health care ethics including ethics, morality, law, bioethics, and cultural diversity. It discusses ethical theories like deontology, consequentialism, and virtue ethics. It also covers ethical principles such as autonomy, beneficence, and justice. The document notes that ethics and law are interrelated and influence each other. It presents examples of ethical dilemmas and discusses how cultural values impact decision making. Finally, it introduces a decision making model called ADPIE that can be used to analyze ethical issues.