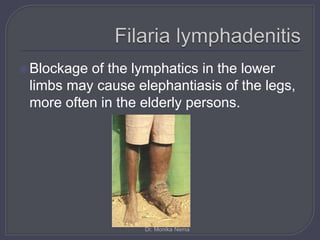
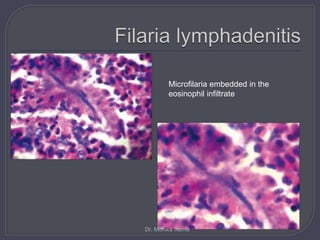
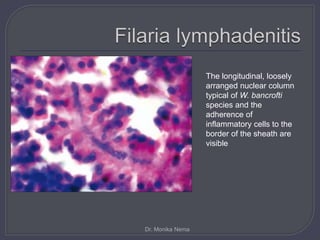
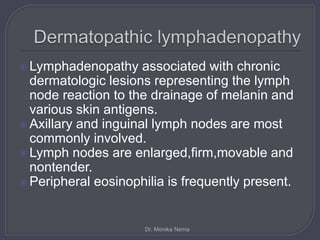
This document discusses various non-neoplastic and neoplastic conditions that can cause lymphadenopathy. It focuses on filariasis as a cause of non-neoplastic lymphadenopathy. Filarial parasites can infect the lymphatics and lymph nodes, causing inflammation and blockage. On pathology, the lymph nodes show an intense inflammatory reaction around dead or dying larvae with eosinophils and multinucleated giant cells. Rarely, microfilaria can be seen embedded in the lymph node tissue. The document emphasizes that a diligent search is needed to identify the parasite and make an accurate diagnosis.