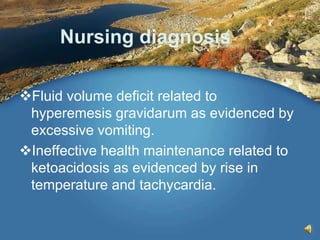
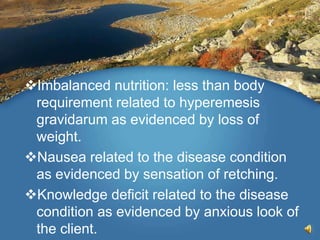
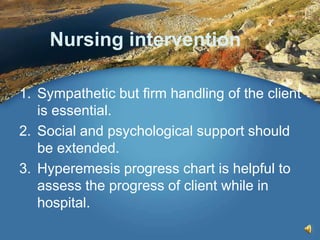
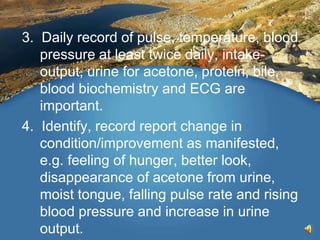
Hyperemesis gravidarum is excessive vomiting during pregnancy that negatively impacts a mother's health or daily activities. It is rare, occurring in less than 1 in 1000 pregnancies. While the exact cause is unknown, it seems to involve high levels of the hormone HCG. Clinical manifestations range from frequent vomiting to signs of dehydration like a dry tongue and jaundice. Management involves hospitalization, IV fluids, antiemetic drugs, nutritional supplements, and in severe cases termination of pregnancy may be considered. The document outlines the definition, causes, symptoms, diagnostic evaluation, complications and nursing management of hyperemesis gravidarum.