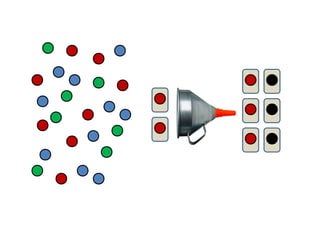
The document discusses improving patient experience in the emergency department at Saint Agnes Medical Center through expediting the time from when a patient arrives to seeing a doctor. The redesign process focused on golden rules of intake to reduce wait times. Results were immediate, with left without being seen rates dropping from 13% to 1%, minutes to see a provider reduced from 90 to 14, and patient satisfaction scores increasing. Security incidents and admit times also improved following the process redesign.