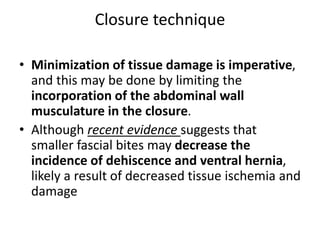
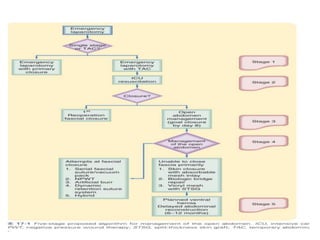
The document discusses difficult abdominal wall closure, techniques for temporary abdominal closure, and definitive abdominal wall reconstruction. It provides details on:
- Ideal suture materials that resist infection and provide strength for closure.
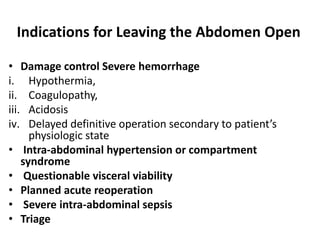
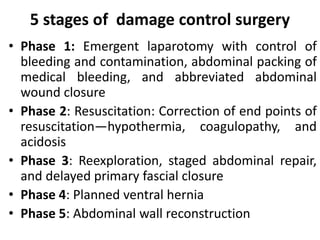
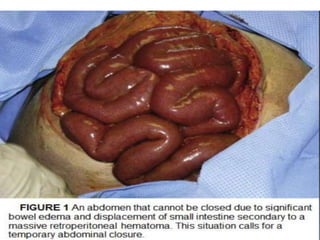
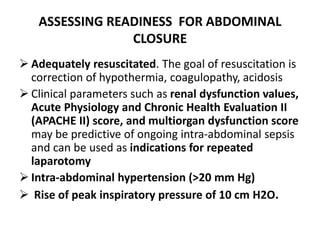
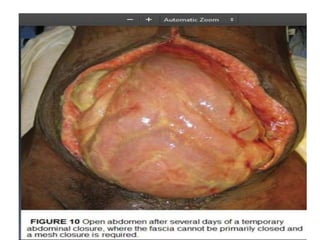
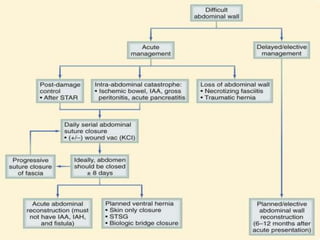
- Indications for leaving the abdomen open such as damage control surgery or intra-abdominal hypertension.
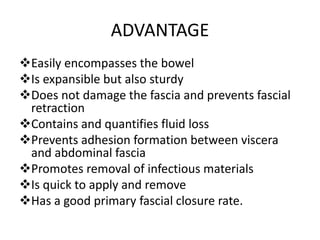
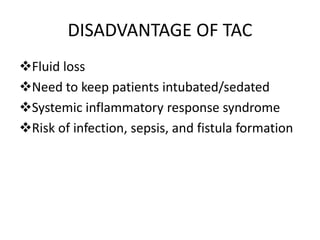
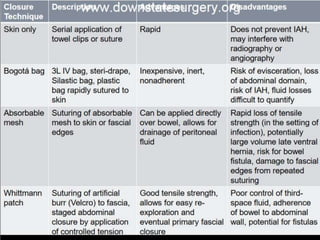
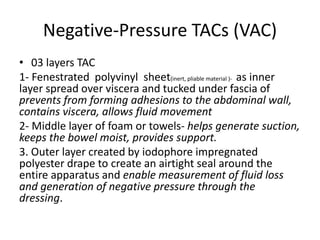
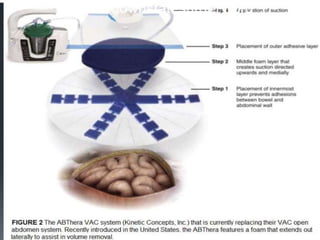
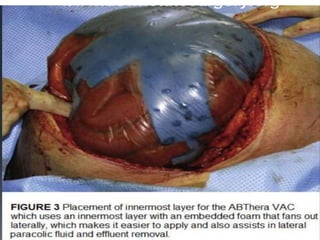
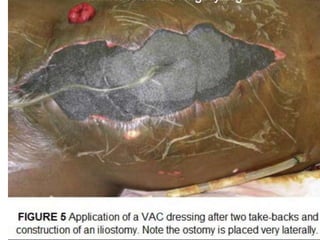
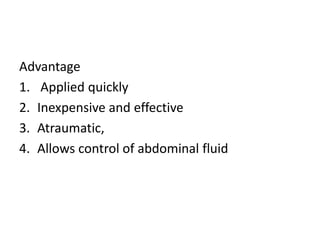
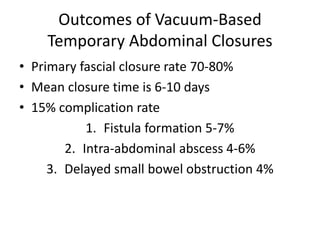
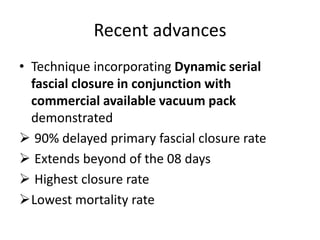
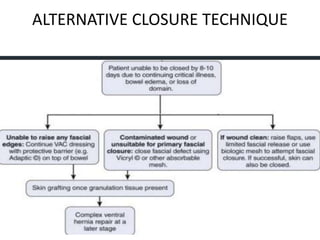
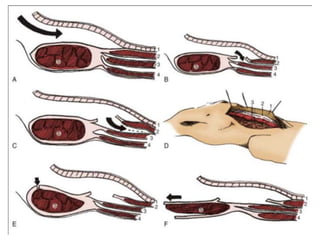
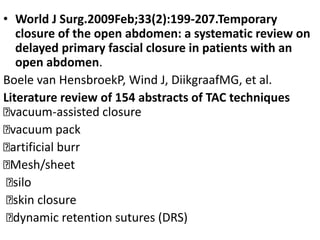
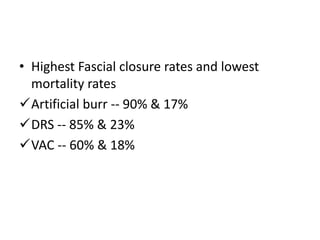
- Temporary abdominal closure techniques including negative pressure devices that control fluids and promote primary fascial closure in 70-80% of cases.
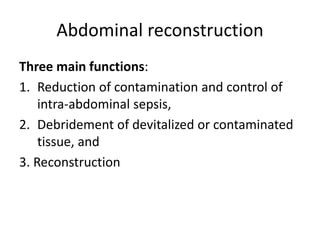
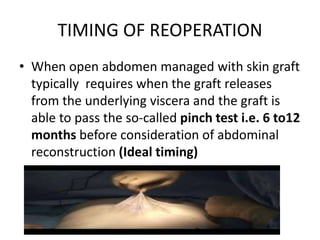
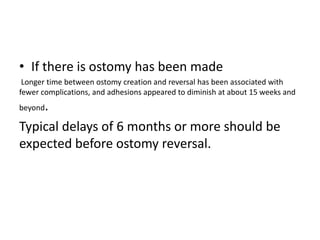
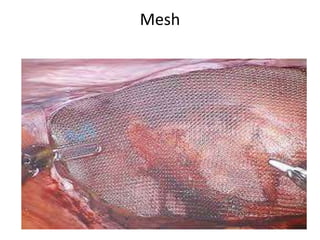
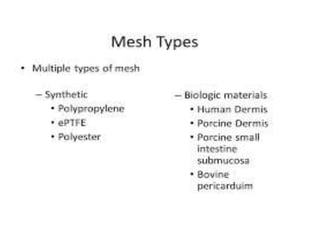
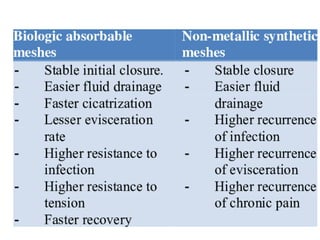
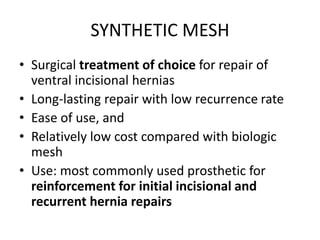
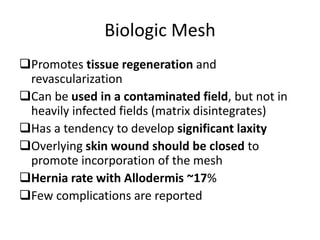
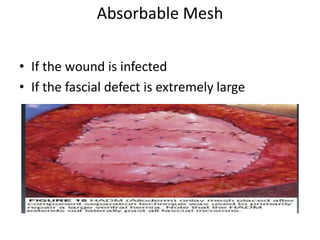
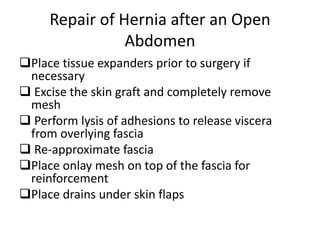
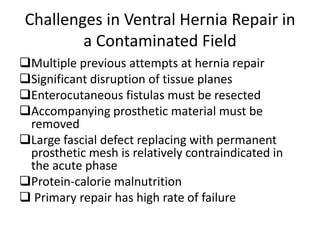
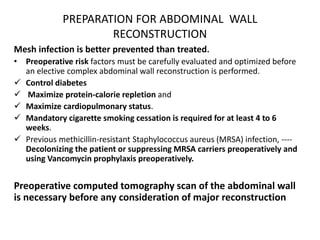
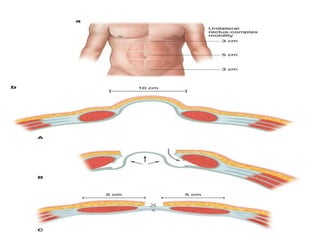
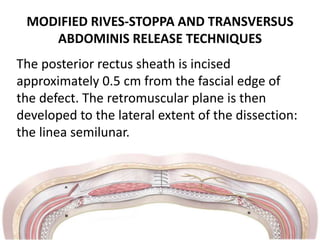
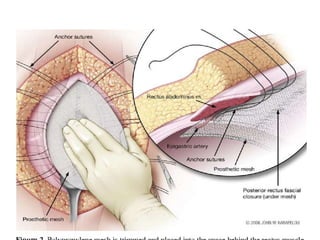
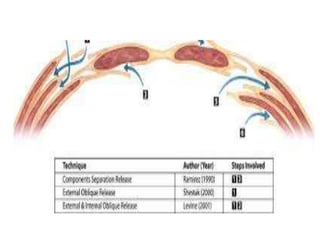
- Factors to consider before definitive reconstruction such as optimizing patient status and using tension-free techniques like component separation with mesh reinforcement for a durable repair.