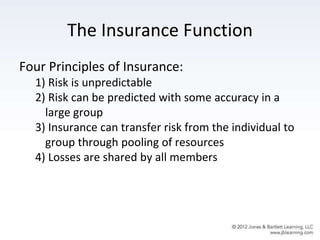
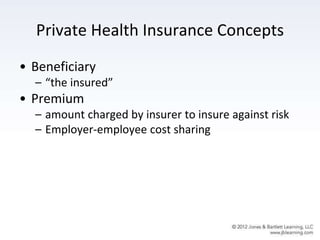
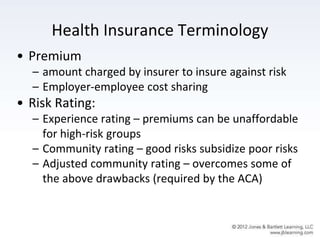
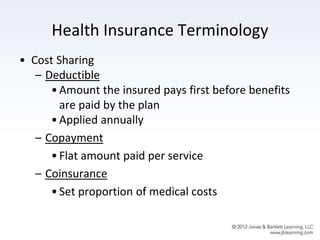
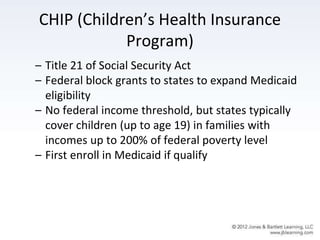
This document discusses various methods of health care financing in the United States including private insurance, public programs, and the Affordable Care Act. It covers key topics like the role of insurance, common health insurance terminology, types of private plans including employer-sponsored and individual plans, public programs like Medicare and Medicaid, and provisions and impacts of the ACA. The learning objectives are to understand concepts of health insurance, distinguish various plan types, examine public programs and insurance trends, and assess directions in health care financing.