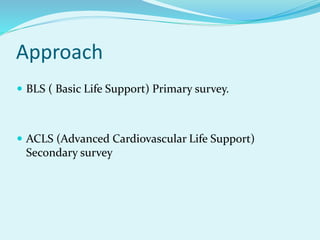
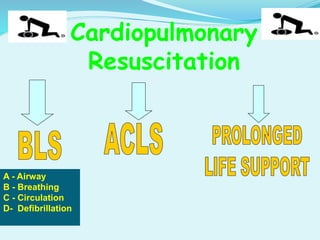
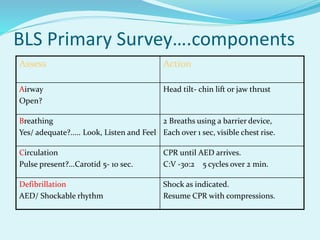
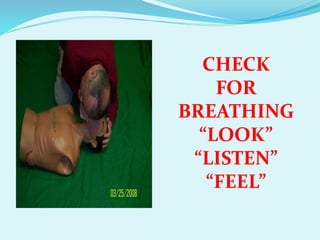
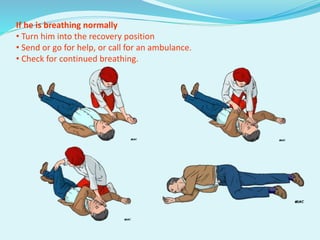
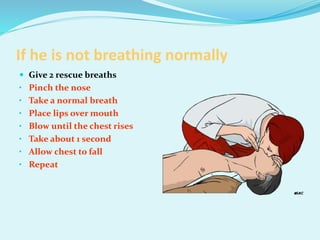
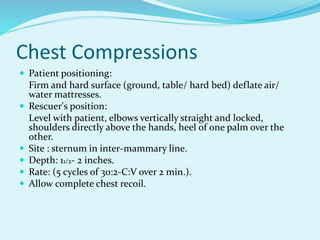
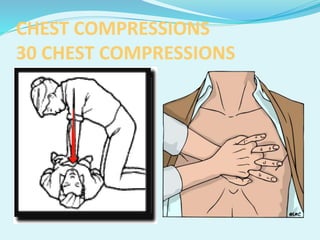
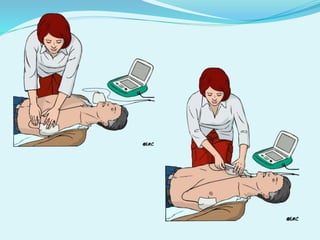
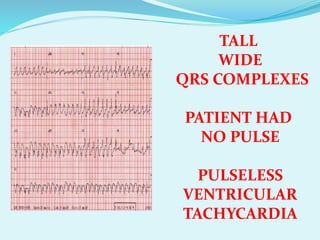
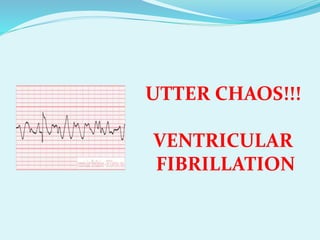
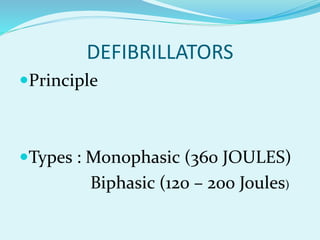
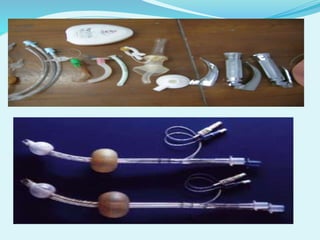
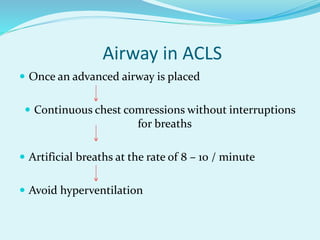
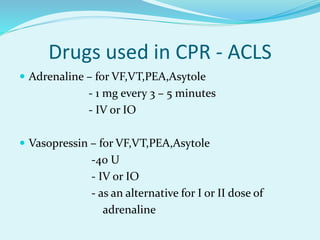
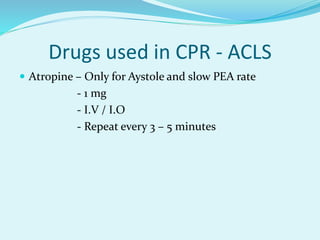
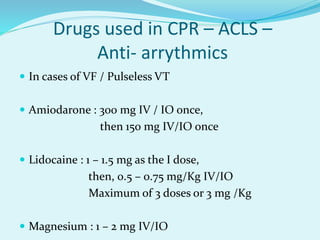
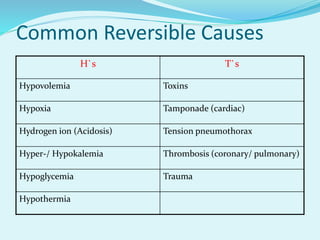
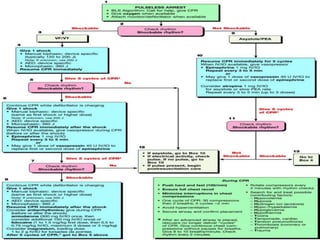
This document discusses cardiopulmonary resuscitation (CPR) and the steps of basic and advanced life support. It states that CPR should begin immediately as brain damage can start within 4-6 minutes. The goals of CPR are to support oxygenation, ventilation and circulation until spontaneous circulation returns. Basic life support involves opening the airway, checking for breathing, giving breaths, checking the pulse and providing chest compressions. Advanced life support uses additional airway techniques and drugs to treat cardiac rhythms and reversible causes of cardiac arrest.