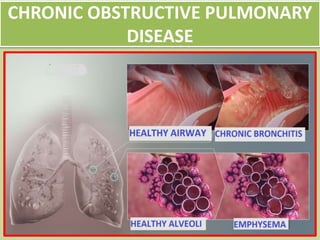
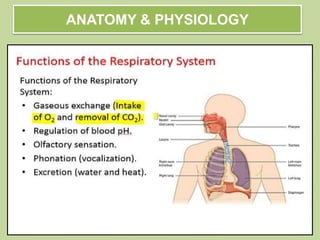
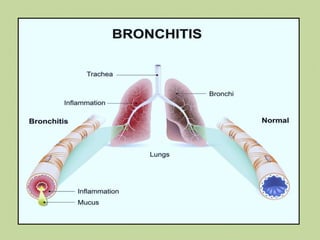
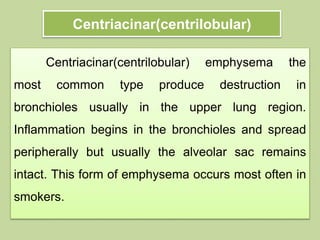
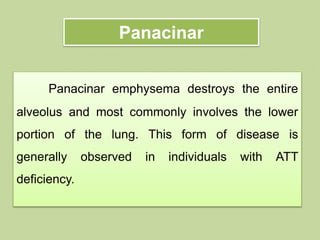
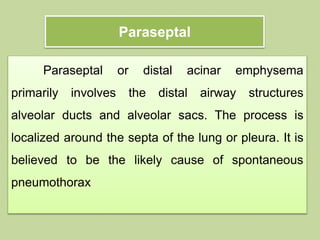
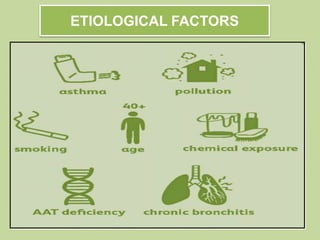
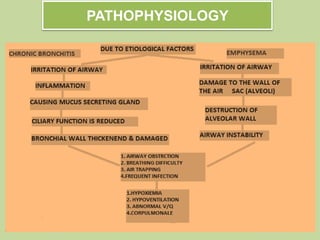
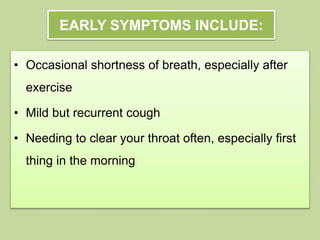
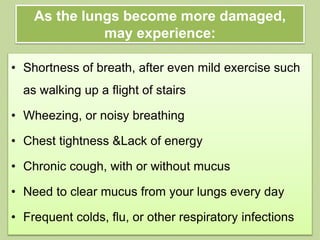
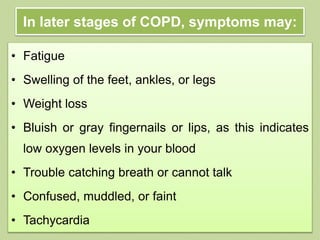
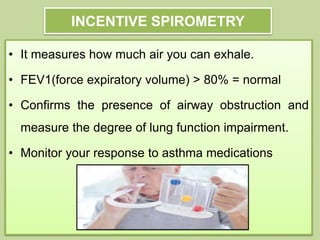
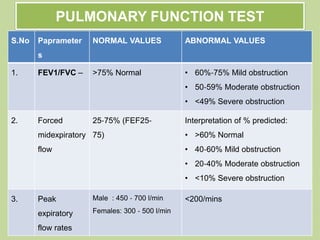
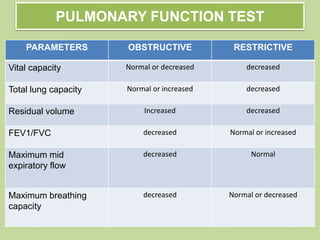
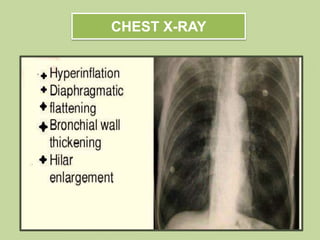
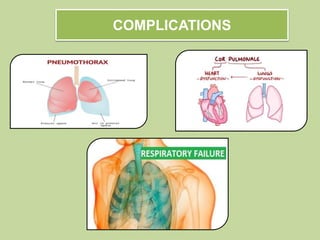
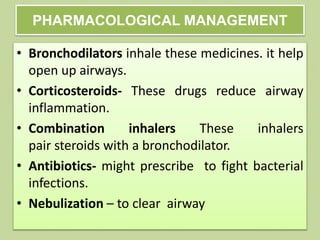
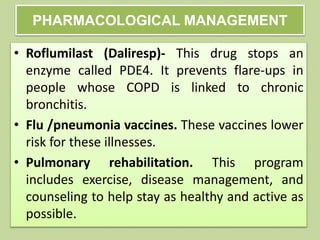
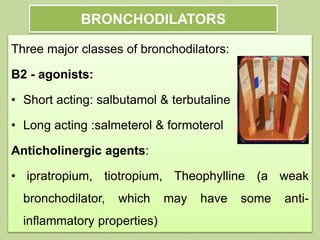
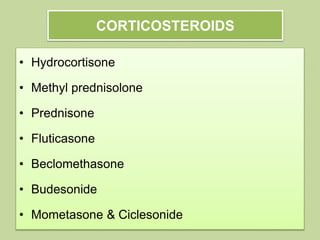
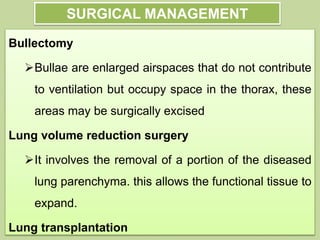
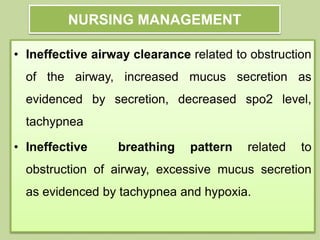
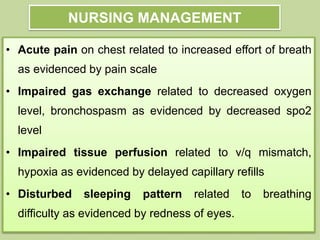
This document provides an overview of Chronic Obstructive Pulmonary Disease (COPD). It begins with an introduction to COPD, describing it as a common lung disease that makes breathing difficult. It then covers the anatomy and physiology of COPD, defining it as a progressive lung disease involving chronic inflammation and airflow obstruction. The document discusses the incidence of COPD globally and risk factors. It provides details on the pathophysiology, stages and symptoms of the disease. Diagnostic tests like spirometry and chest x-rays are described. The document outlines complications of COPD and approaches to medical management including pharmacology, surgery, and nursing care. It provides details on specific drugs like bronchodilators and corticosteroids used to