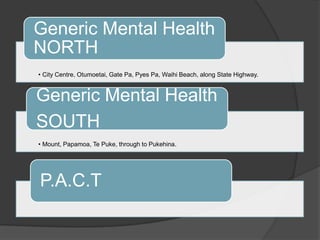
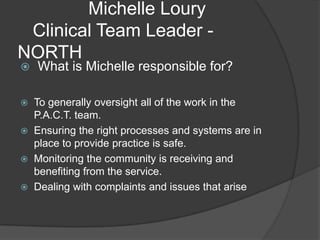
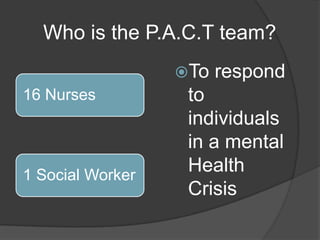
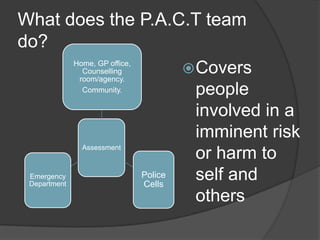
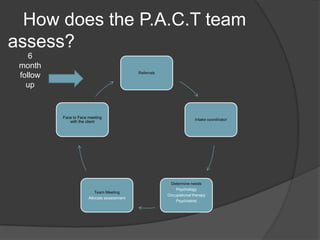
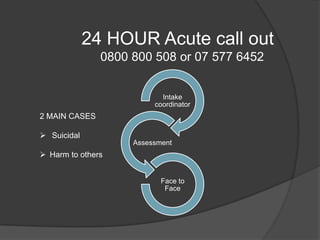
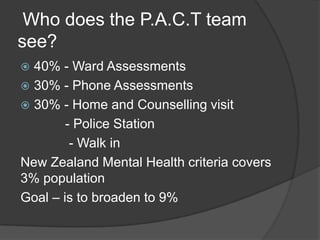
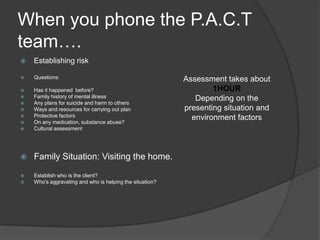
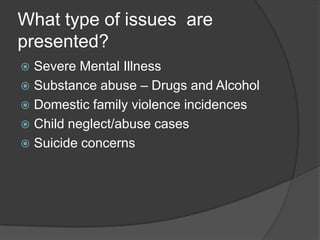
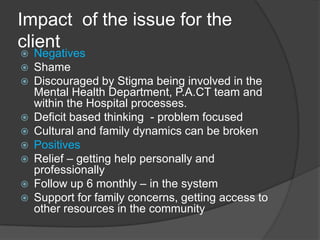
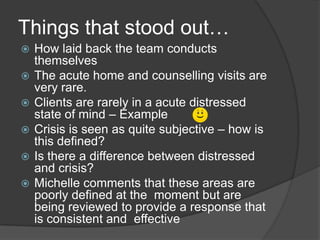
The document describes the roles and responsibilities of the P.A.C.T. mental health team in the north region, which is led by Michelle Loury and responds to individuals in mental health crises through assessments, referrals, treatment, and 6 month follow ups. It provides details on how the team operates, the types of issues they see, and their process for assessing and supporting clients in various locations throughout the community.