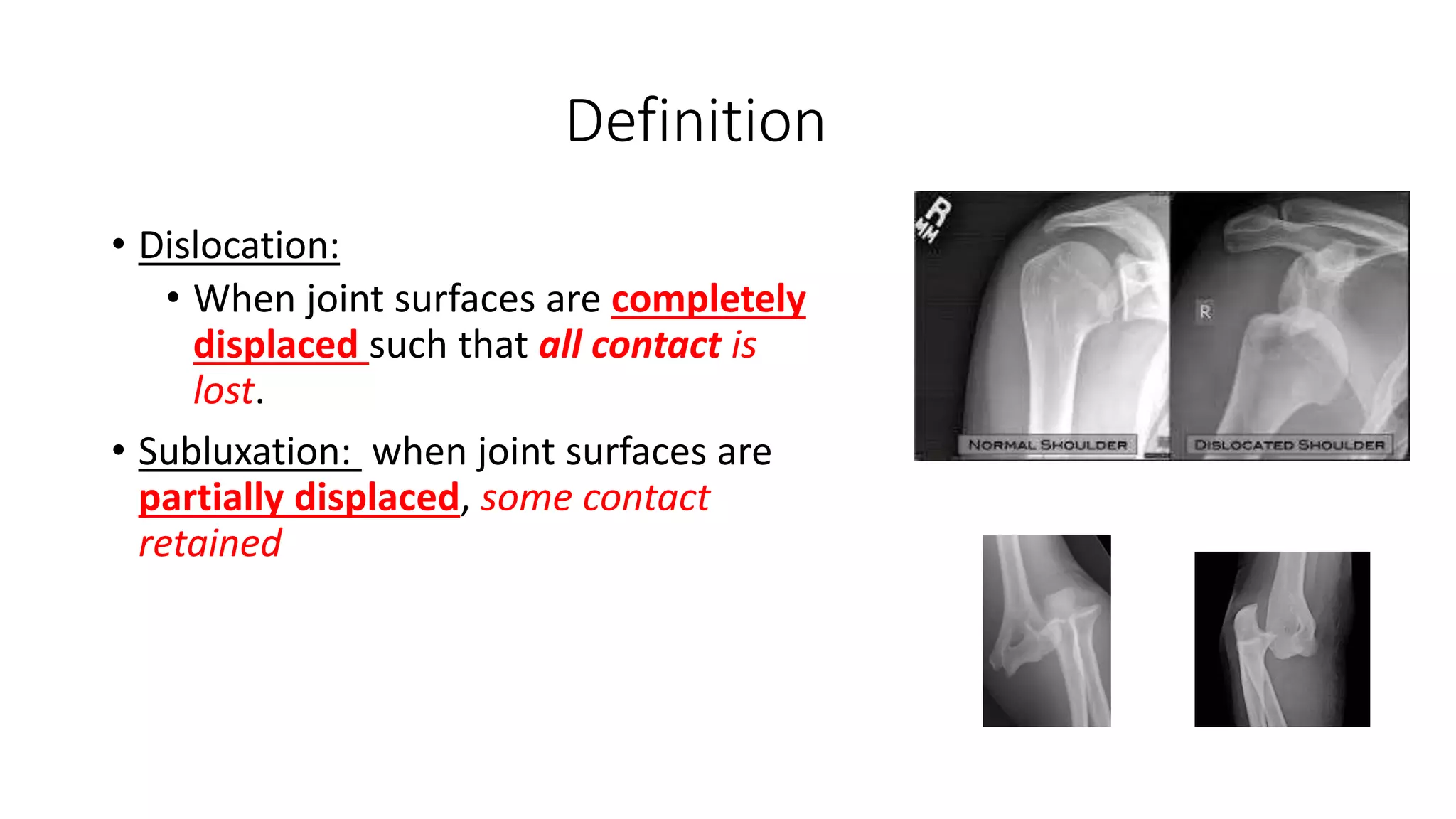
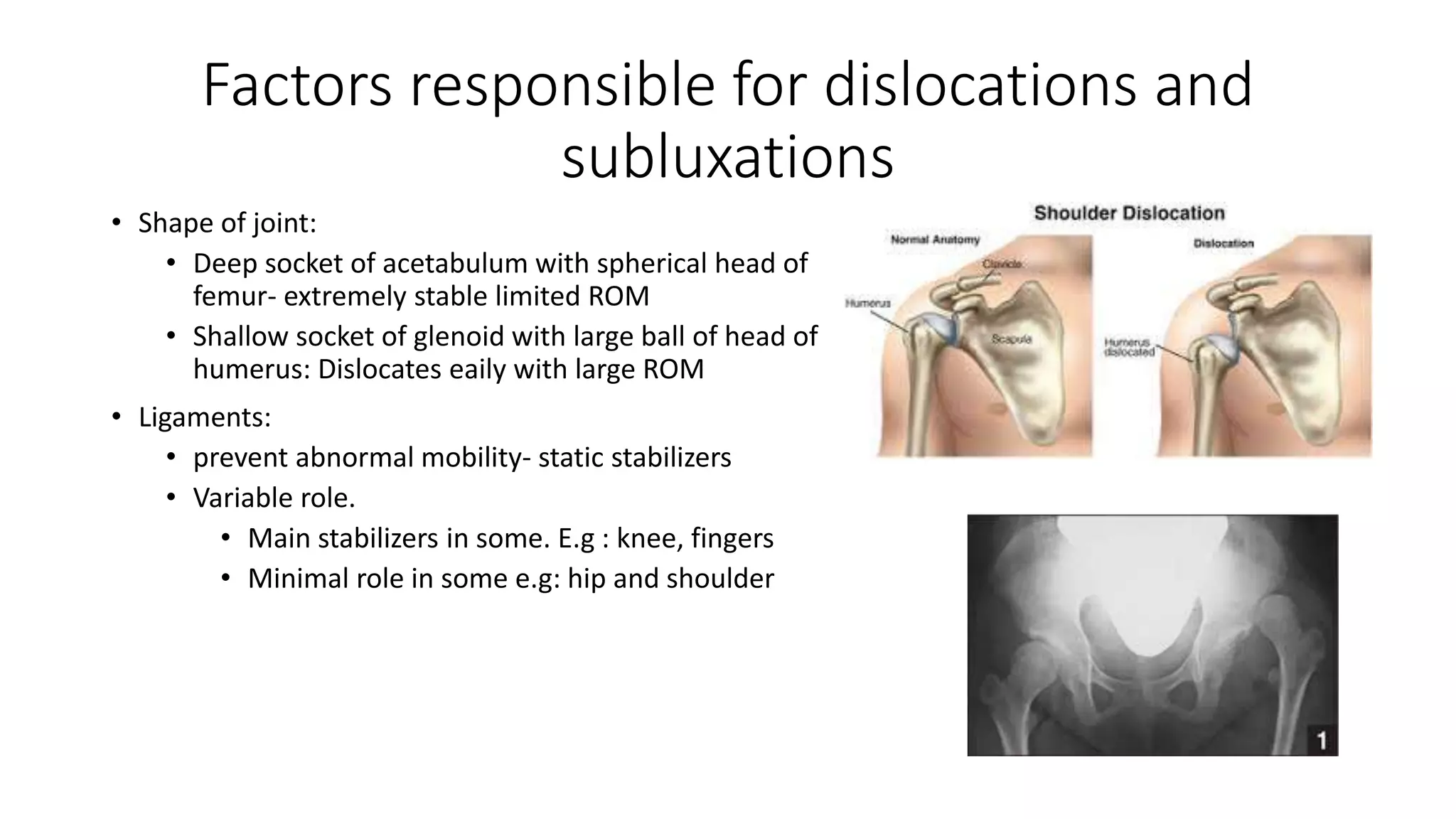
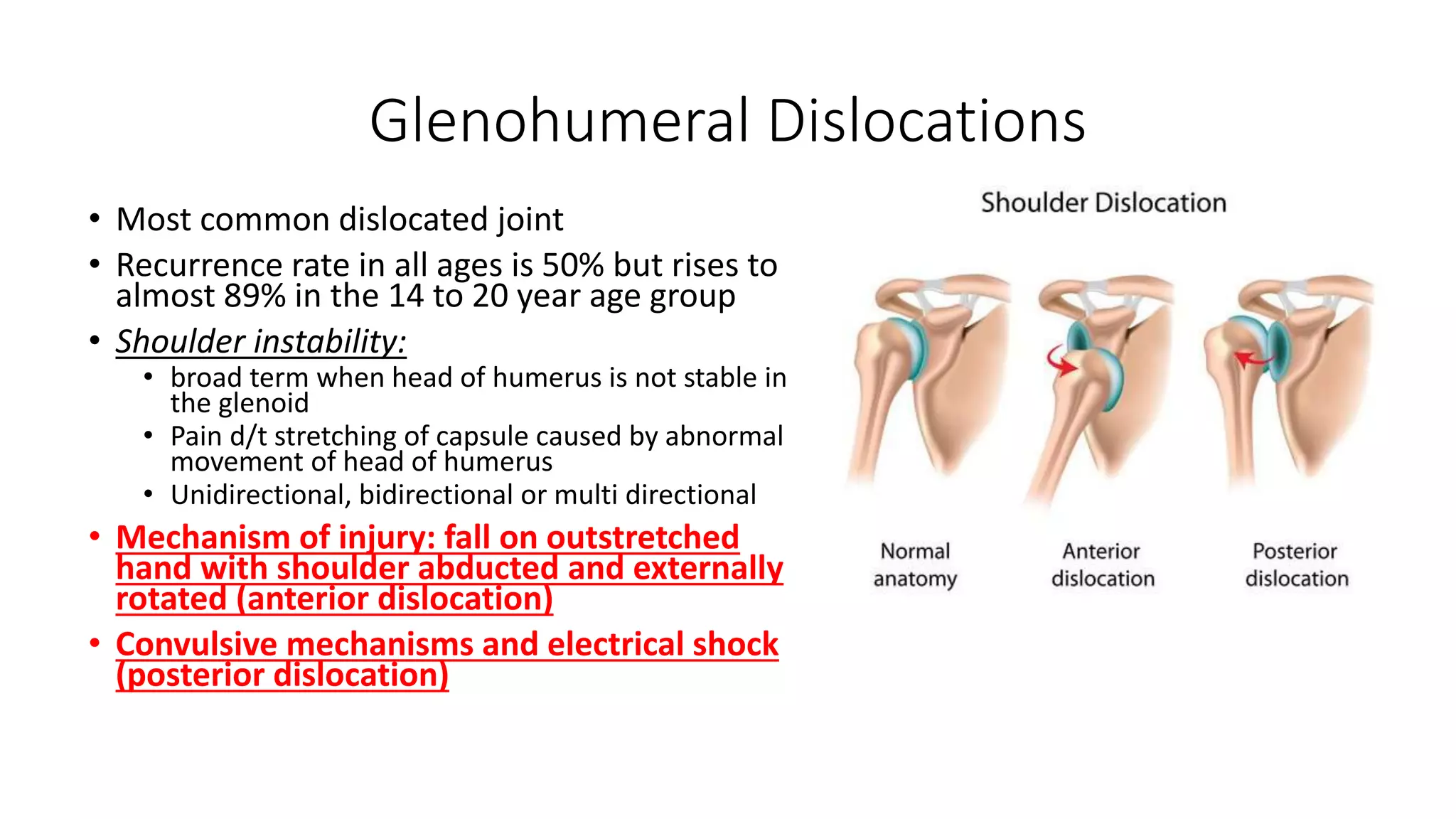
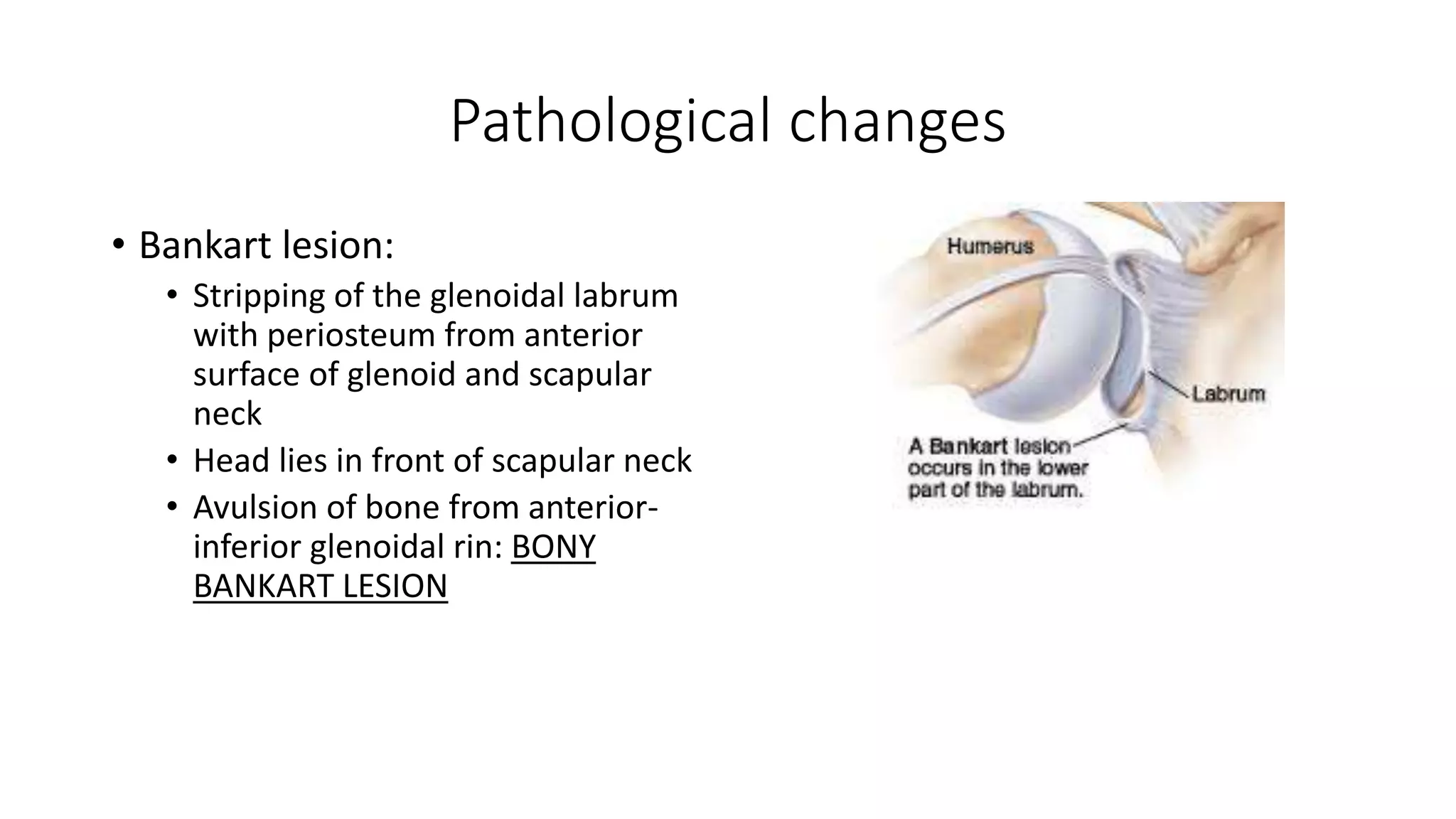
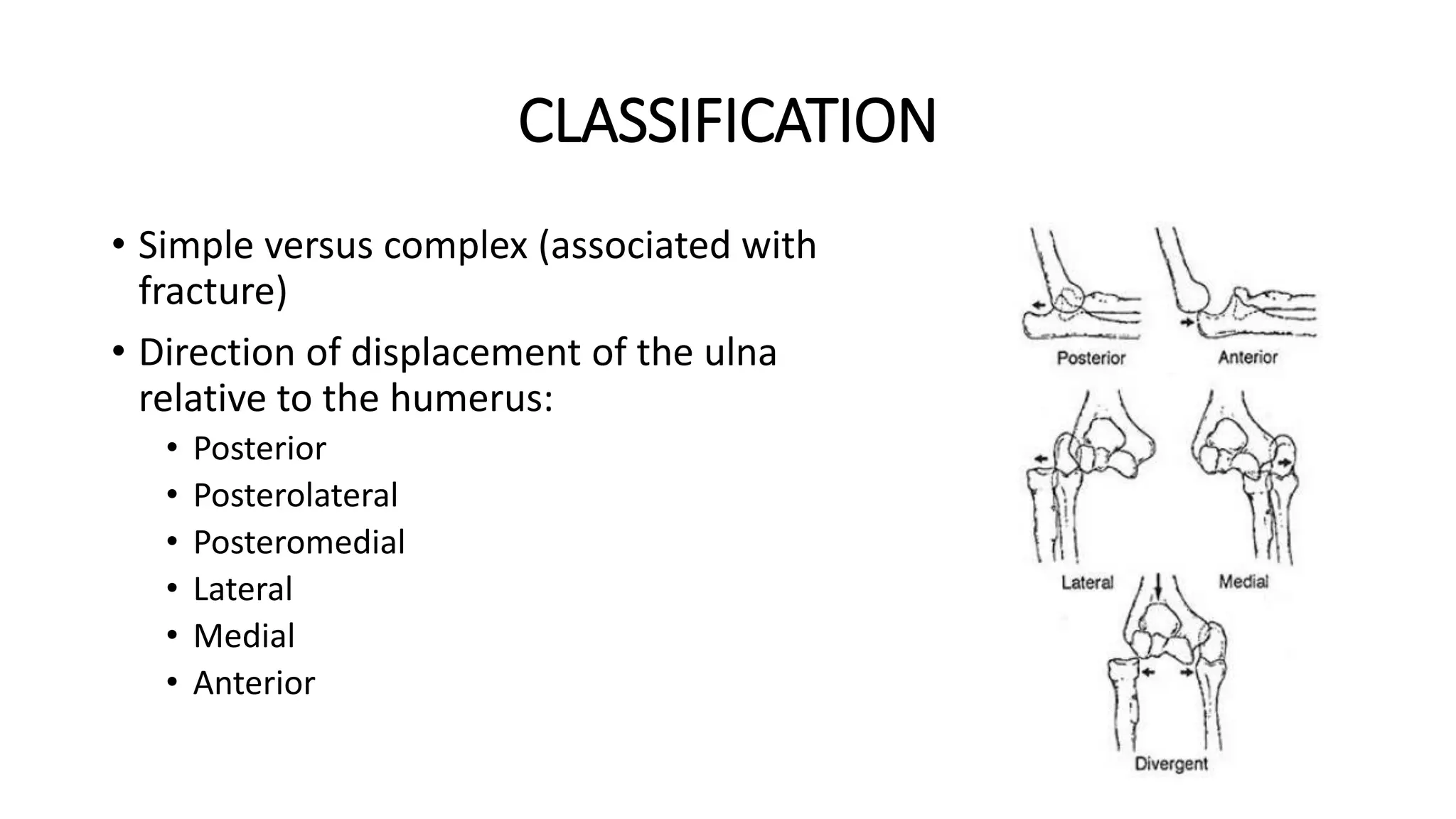
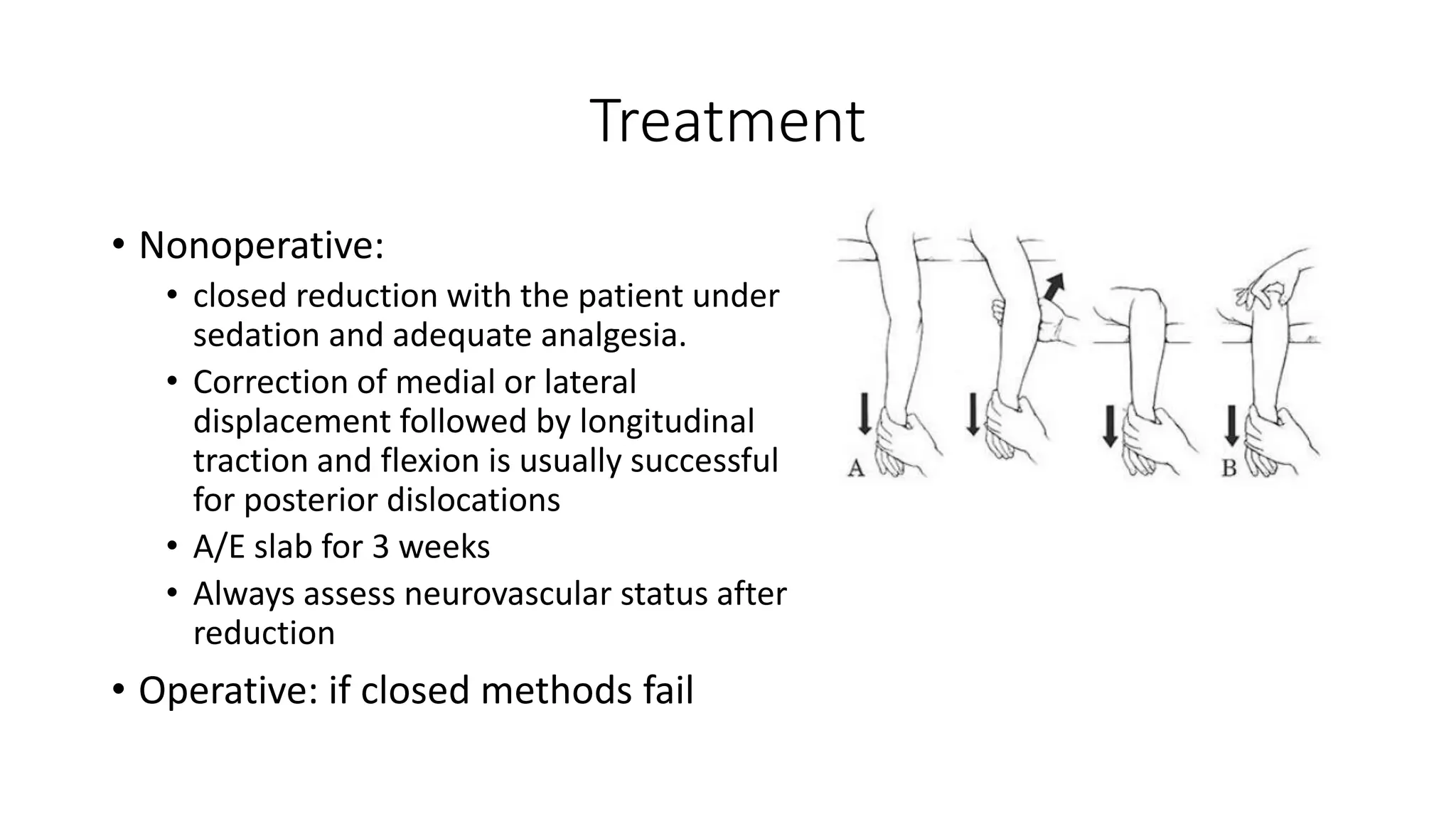
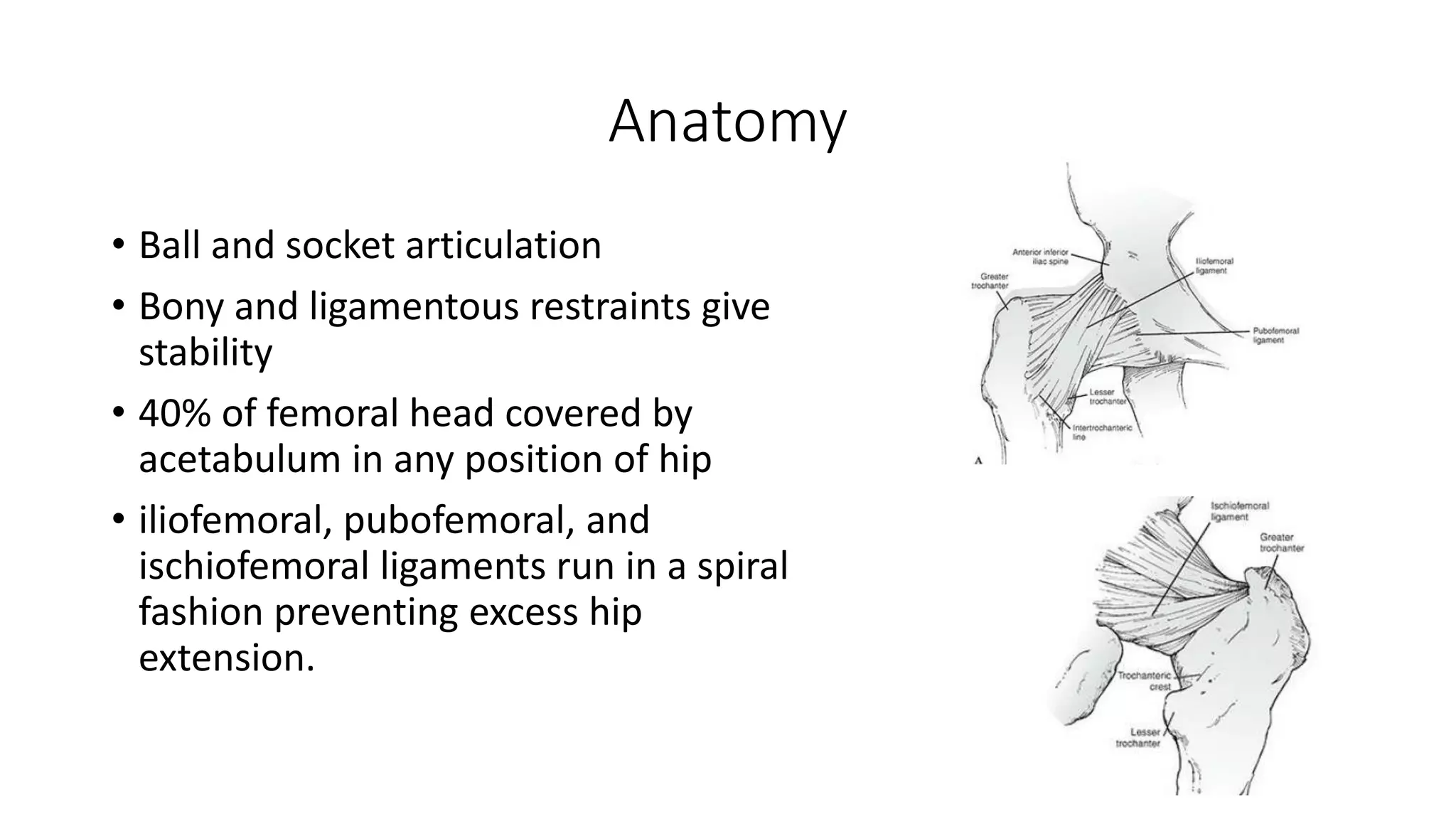
Dislocations and subluxations involve the displacement of joint surfaces. A dislocation is a complete displacement where all contact is lost, while a subluxation is a partial displacement where some contact is retained. Key factors that can cause dislocations are the shape and stability of the joint, surrounding ligaments and muscles. Dislocations are classified based on cause (traumatic vs pathological), direction of displacement, and presence of fractures. Treatment involves closed or open reduction depending on the severity of the injury. Complications can include neurovascular injuries, recurrent dislocations, fractures, stiffness and osteoarthritis.