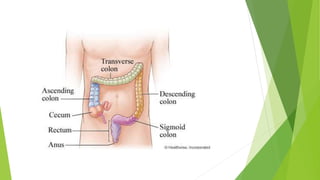
Colitis is inflammation of the inner lining of the large intestine. There are several types of colitis, including ulcerative colitis where the immune system attacks the digestive tract, causing bleeding ulcers. Pseudomembranous colitis occurs when an overgrowth of the Clostridium difficile bacteria disrupts the normal gut bacteria. Symptoms include abdominal pain, diarrhea, and weight loss. Treatment depends on the severity but may include anti-inflammatory drugs, immune suppressants, antibiotics, or surgery to remove all or part of the colon.