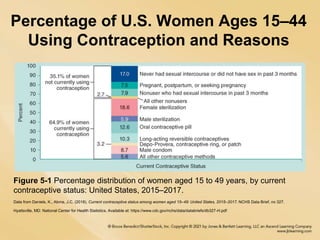
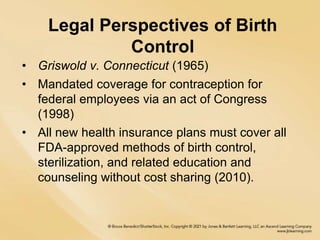
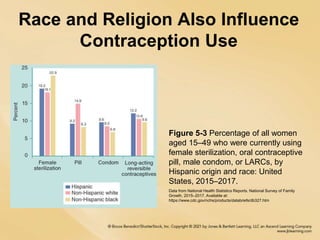
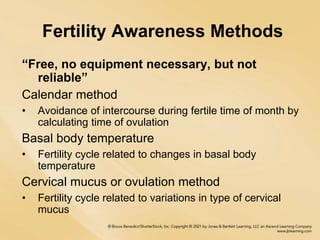
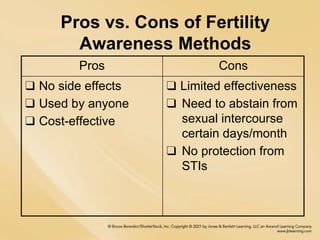
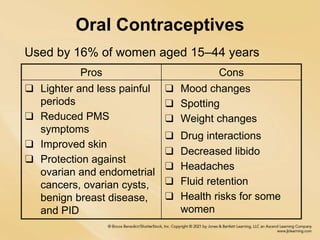
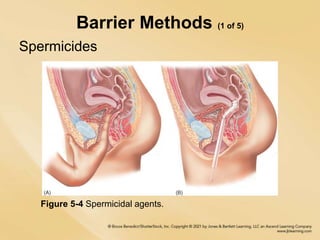
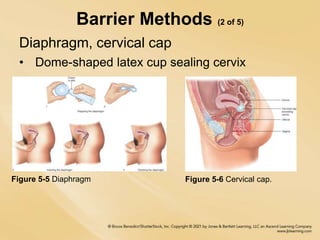
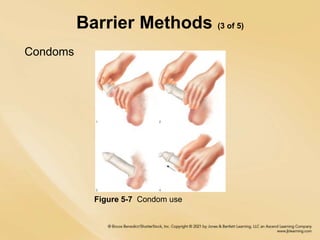
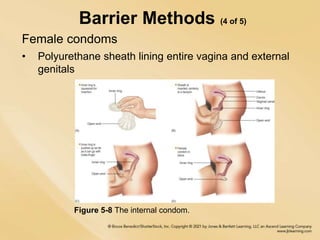
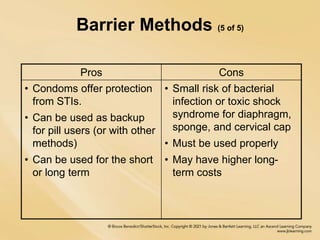
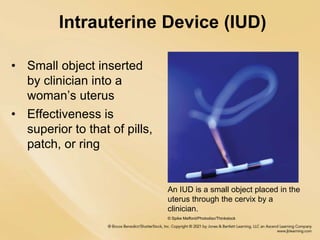
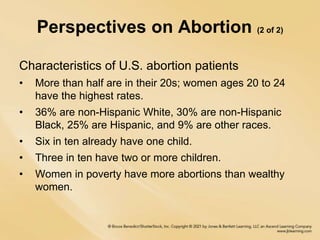
This document provides an overview of reproductive health topics including birth control methods, contraception use in the US, perspectives on abortion, and global maternal health issues. It discusses the types of birth control including hormonal methods (pills, IUDs), barrier methods (condoms, diaphragms), fertility awareness techniques, and permanent sterilization. Abortion procedures like medical and surgical abortion are also outlined. The perspectives section notes common reasons women choose abortion and characteristics of US abortion patients. A discussion of informed decision making and reducing unsafe abortion globally is presented.