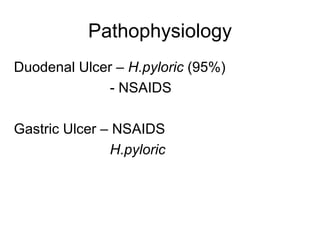
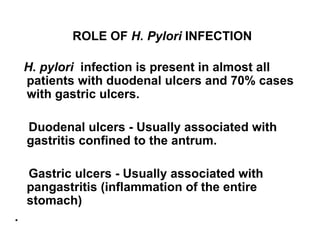
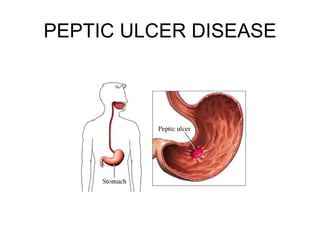
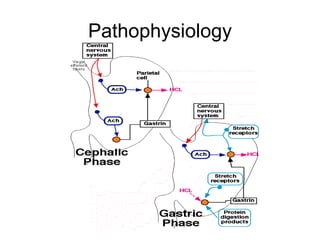
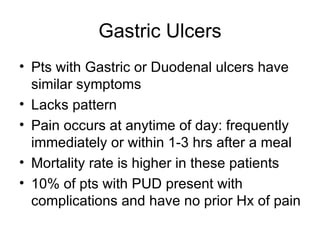
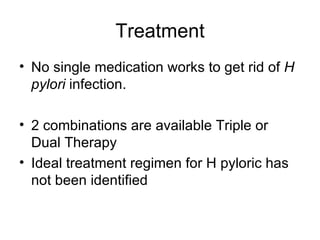
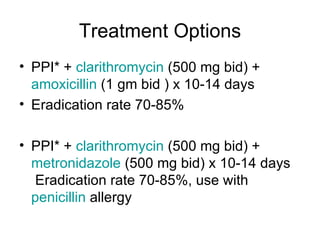
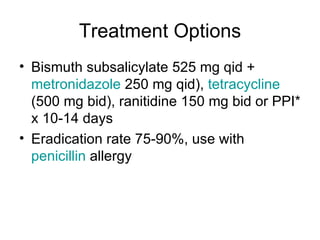
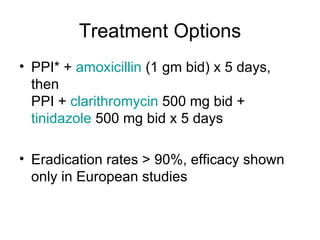
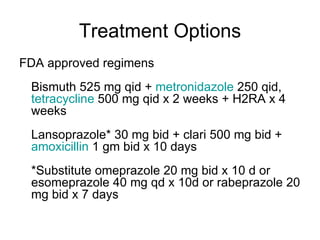
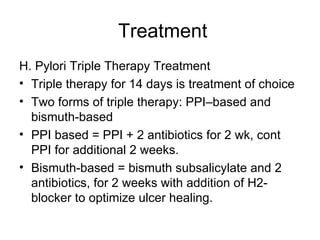
Peptic ulcer disease is caused by an imbalance between aggressive gastric factors like acid and pepsin and protective mucosal defenses. H. pylori infection plays a key role in most peptic ulcers by damaging the mucosal layer. Treatment involves eradicating H. pylori with triple therapy using a PPI and two antibiotics for 2 weeks, and continuing PPI therapy for an additional 2 weeks to aid ulcer healing. Adherence to the full treatment course is important for successful eradication.