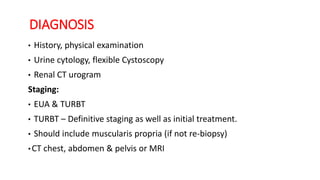
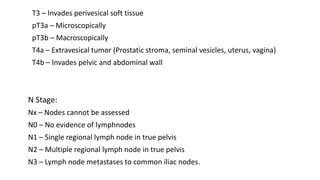
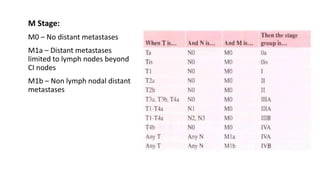
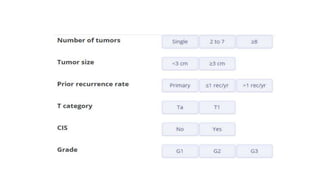
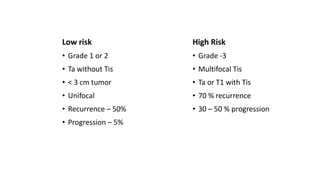
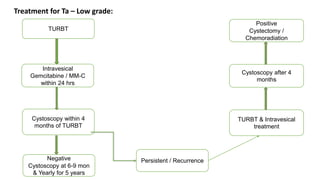
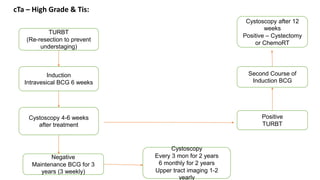
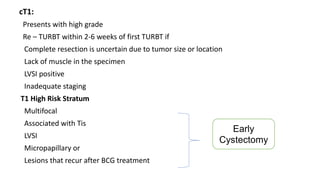
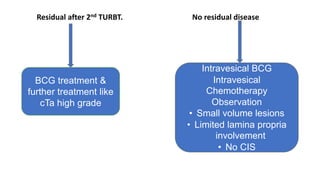
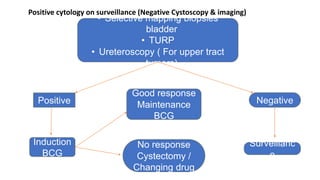
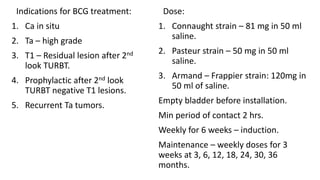
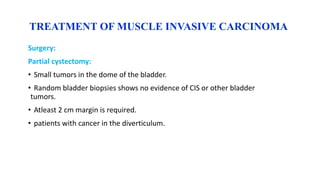
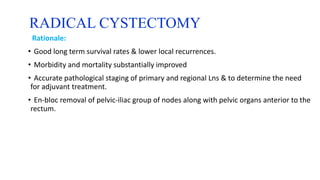
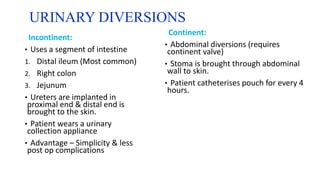
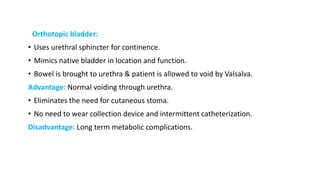
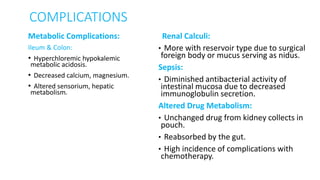
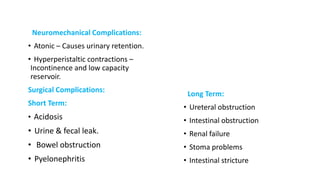
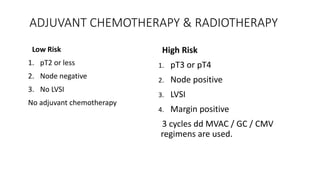
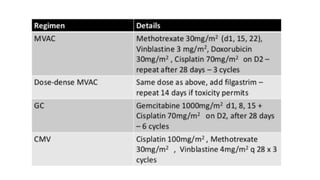
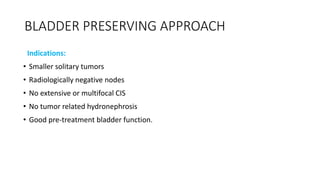
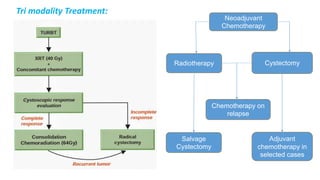
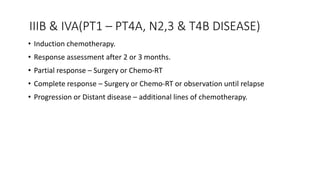
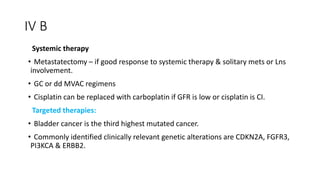
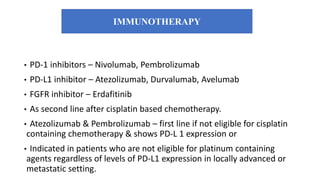
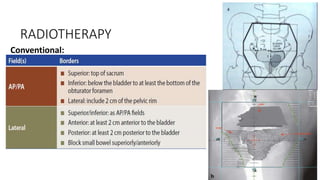
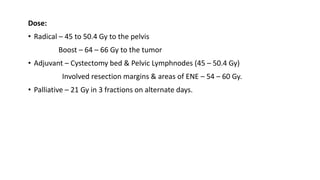
This document discusses the management of bladder carcinoma. It covers diagnosis through cystoscopy and imaging. Staging is described using the TNM system. Treatment options are provided for non-muscle invasive bladder cancer including transurethral resection and intravesical therapies. Muscle invasive bladder cancer treatment involves radical cystectomy with urinary diversion or bladder preservation approaches using chemoradiation. Adjuvant therapies and management of metastatic disease is also outlined. Complications of treatment and approaches to radiotherapy are summarized.