This document provides an overview of bronchiolitis including pathogenesis, microbiology, risk factors, clinical presentation, diagnosis, and treatment recommendations. Bronchiolitis is typically caused by viral infection, most commonly RSV, and causes inflammation in the small airways. Clinical diagnosis is based on symptoms of fever, cough and respiratory distress. Treatment focuses on supportive care like hydration and supplemental oxygen rather than medications like bronchodilators or steroids which studies have shown are not effective. High flow nasal cannula may help reduce respiratory distress. Prevention involves reducing exposure to tobacco smoke which increases risk and severity.
![■ Clinical presentation: Fever (usually ≤38.3ºC [101ºF]), cough, and respiratory distress
(eg, increased respiratory rate, retractions, increased work of breathing, wheezing,
crackles, hypoxia). It often is preceded by a one- to three-day history of upper
respiratory tract symptoms (eg, nasal congestion and/or discharge)
■ Clinical course:Typical illness with bronchiolitis begins with upper respiratory tract
symptoms, followed by lower respiratory tract signs and symptoms on days two to
three, which peak on days three to five and then gradually resolve.
In a systematic review of four studies including 590 children with bronchiolitis, the
mean time to resolution of cough ranged from 8 to 15 days.1
■ Dehydration a major complication: Infants with bronchiolitis may have difficulty
maintaining adequate hydration because of increased fluid needs (related to fever and
tachypnea), decreased oral intake (related to tachypnea and respiratory
distress), and/or vomiting2.They should be monitored for dehydration (eg, increased
heart rate, dry mucosa, sunken fontanelle, decreased urine output](https://image.slidesharecdn.com/bronchiolitis-200527193507/85/Bronchiolitis-4-320.jpg)
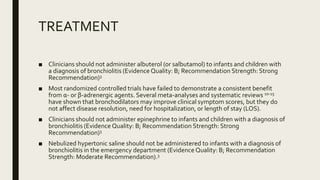
![■ Clinicians should not administer systemic corticosteroids to infants with a diagnosis of
bronchiolitis in any setting (Evidence Quality:A; Recommendation Strength: Strong
Recommendation).3
■ Clinicians may choose not to administer supplemental oxygen if the oxyhemoglobin
saturation exceeds 90% in infants and children with a diagnosis of bronchiolitis
(Evidence Quality: D; Recommendation Strength:Weak Recommendation [based on
low-level evidence and reasoning from first principles])3
■ Clinicians should not administer systemic corticosteroids to infants with a diagnosis of
bronchiolitis in any setting (Evidence Quality:A; Recommendation Strength: Strong
Recommendation).3
■ Use of humidified, heated, high-flow nasal cannula to deliver air-oxygen mixtures
provides assistance to infants with bronchiolitis through multiple proposed
mechanisms.16 There is evidence that high-flow nasal cannula improves physiologic
measures of respiratory effort and can generate continuous positive airway pressure in
bronchiolitis.17-20
Clinical evidence suggests it reduces work of breathing21,22 and may decrease need for
shown by the retrospective study from Australia,23 which showed a decline in
intubation rate in the subgroup of infants with bronchiolitis from 37% to 7% after the
introduction of high-flow nasal cannula](https://image.slidesharecdn.com/bronchiolitis-200527193507/85/Bronchiolitis-12-320.jpg)