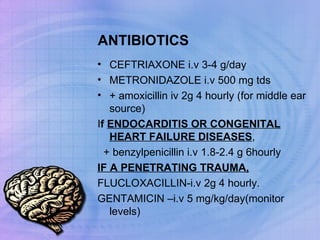
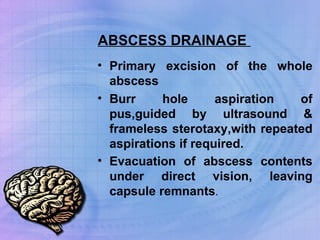
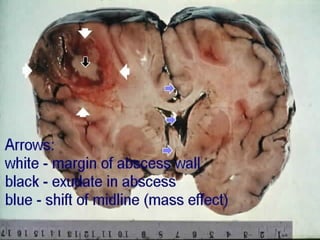
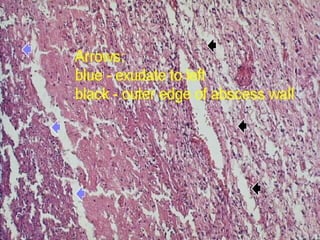
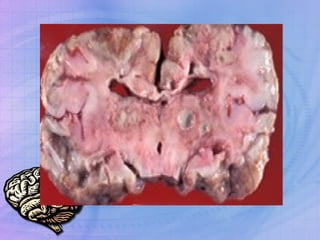
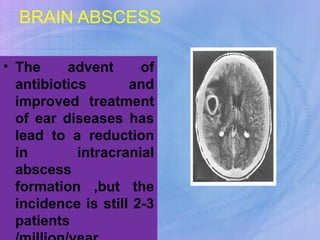
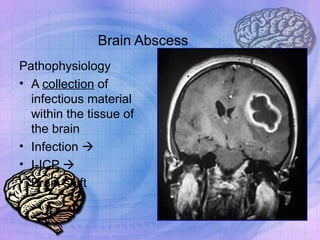
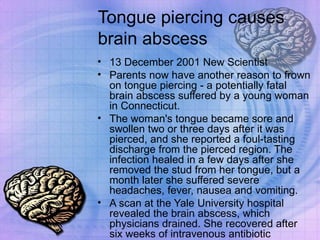
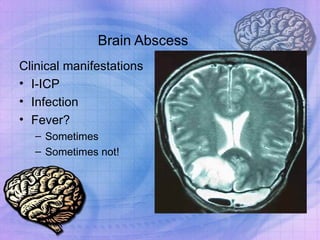
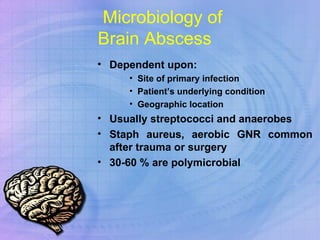
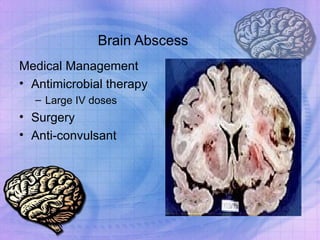
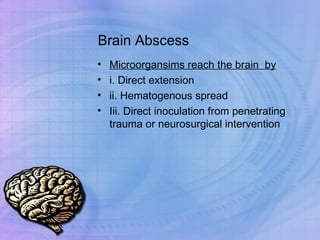
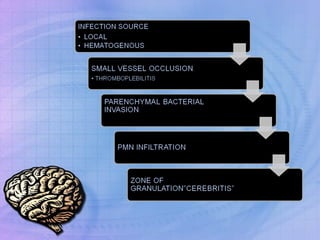
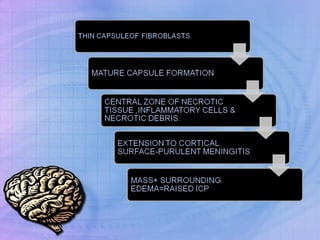
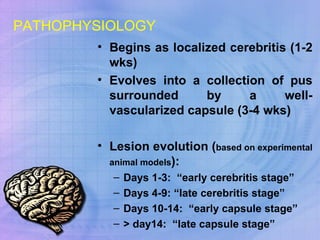
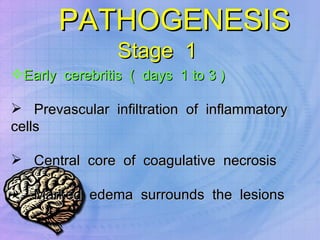
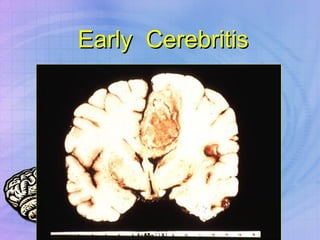
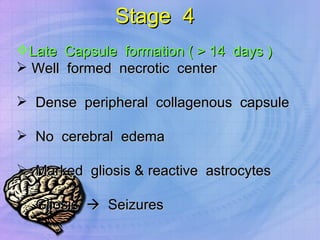
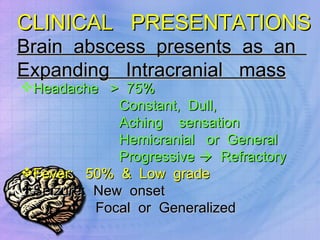
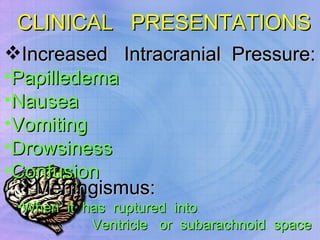
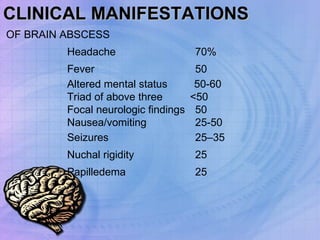
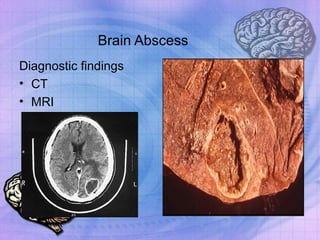
Brain abscesses occur when bacteria or other microorganisms infect the brain tissue. They are usually caused by infections that have spread from other areas of the body, such as the ears, sinuses, or lungs. Common symptoms include headache, fever, nausea, and seizures. Diagnosis involves CT or MRI scans of the brain. Treatment consists of intravenous antibiotics for 6-8 weeks along with surgical drainage or resection of the abscess when possible.



![MEDICAL TREATMENT ONLY Only in pts with prohibitive surgical risk: poor surgical candidate, multiple abscesses, in a dominant location, Abscess size < 2.5 cm concomitant meningitis, ependymitis, early abscess (cerebritis?) with improvement on abx, [Better-vascularized cortical lesions more likely to respond to abx alone] [ Subcortical/white-matter lesions are poorly vascularized]](https://image.slidesharecdn.com/hbrainabscess-jas-090314153004-phpapp02/85/BRAIN-ABSCESS-48-320.jpg)