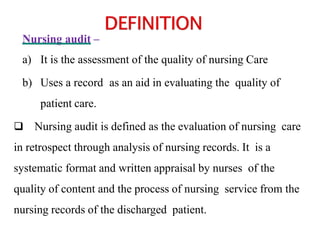
The document discusses nursing audit, which is defined as the evaluation of nursing care through retrospective analysis of nursing records. It aims to assess the quality of clinical nursing care against established standards. The summary includes three key points about nursing audit:
1. Nursing audit involves a systematic review of nursing records to evaluate whether good nursing practices were followed and standards of care were met.
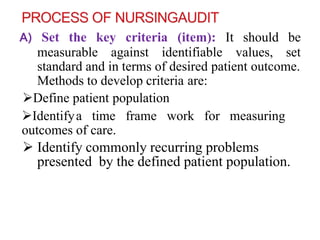
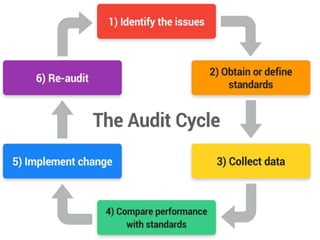
2. The audit process generally involves setting criteria, designing a tool, implementing the tool to collect data from patient records, analyzing the data, and using results to modify nursing care plans and processes.
3. Results from nursing audits can be used to identify areas of weak performance, guide education programs, and help with resource allocation to improve the