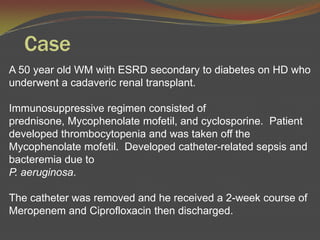
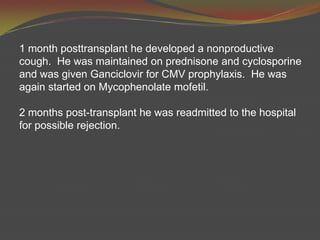
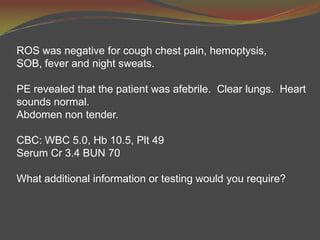
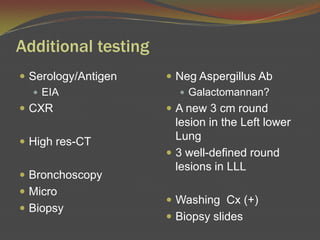
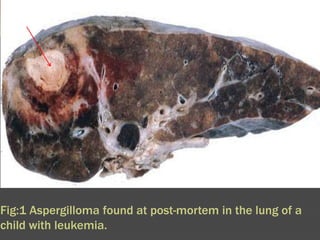
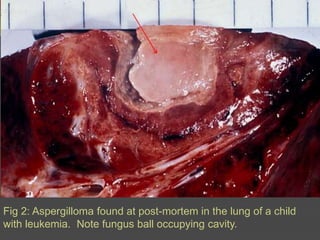
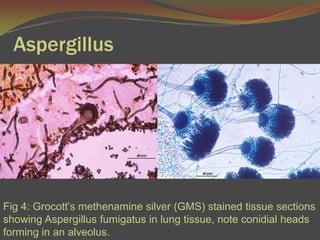
A 50-year-old man with a history of end-stage renal disease and diabetes underwent a kidney transplant. He later developed a nonproductive cough. Additional testing showed a new lung lesion and biopsy revealed Aspergillus fungus. Invasive pulmonary aspergillosis was diagnosed. Treatment guidelines recommend the antifungal drug voriconazole as the primary treatment, with alternative options including other antifungals depending on the patient's condition and test results.