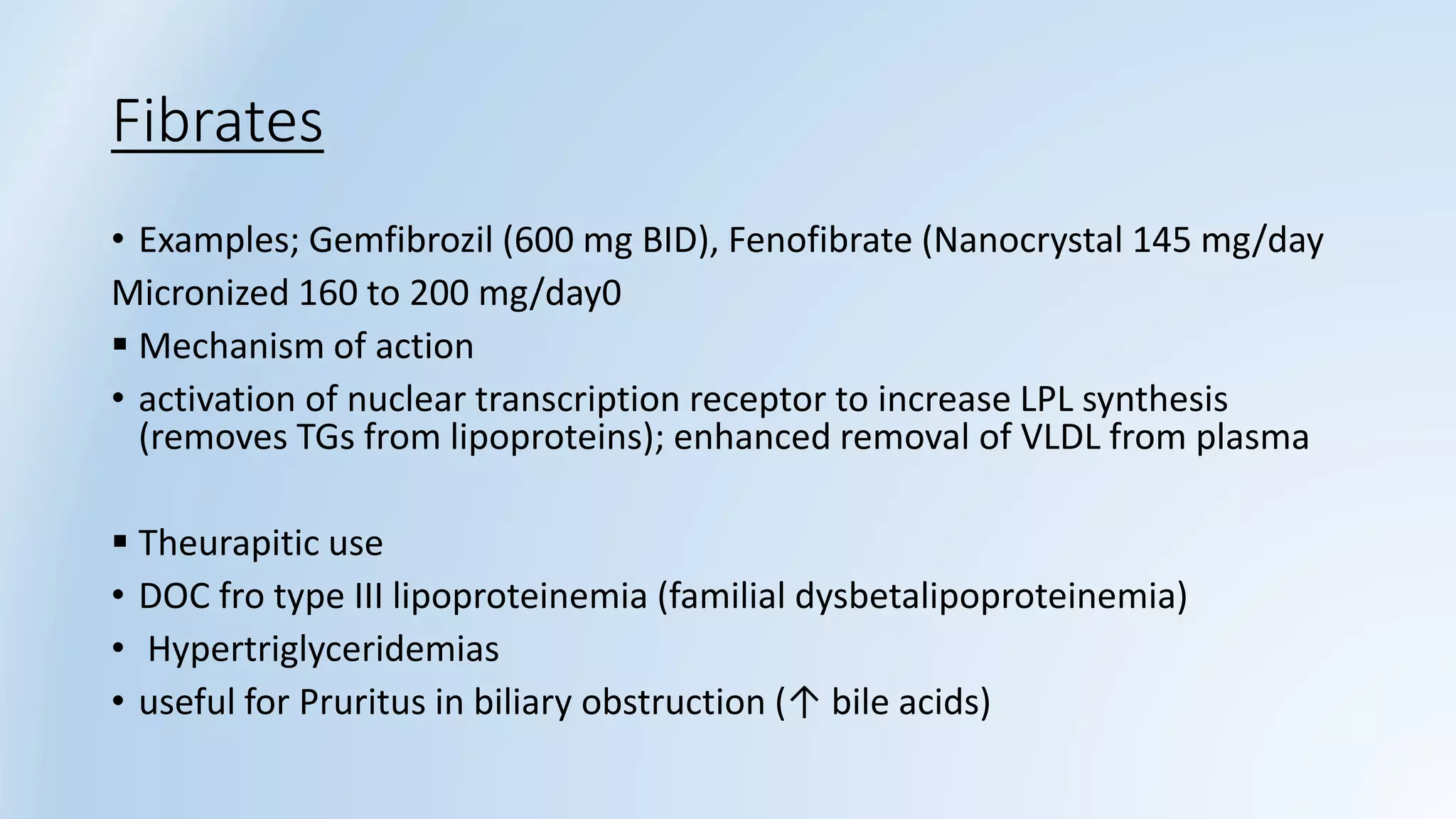
This document discusses antihyperlipidemic drugs used to treat hyperlipidemia. It begins by defining hyperlipidemia and describing risk factors. It then covers the various classes of lipid-lowering drugs including HMG-CoA reductase inhibitors (statins), bile acid sequestrants, fibrates, nicotinic acid, cholesterol absorption inhibitors, and PCSK9 inhibitors. For each class, it provides examples of drugs, their mechanisms of action, therapeutic uses, and major side effects and drug interactions. The document concludes with recommendations on drug therapy and monitoring treatment effectiveness.