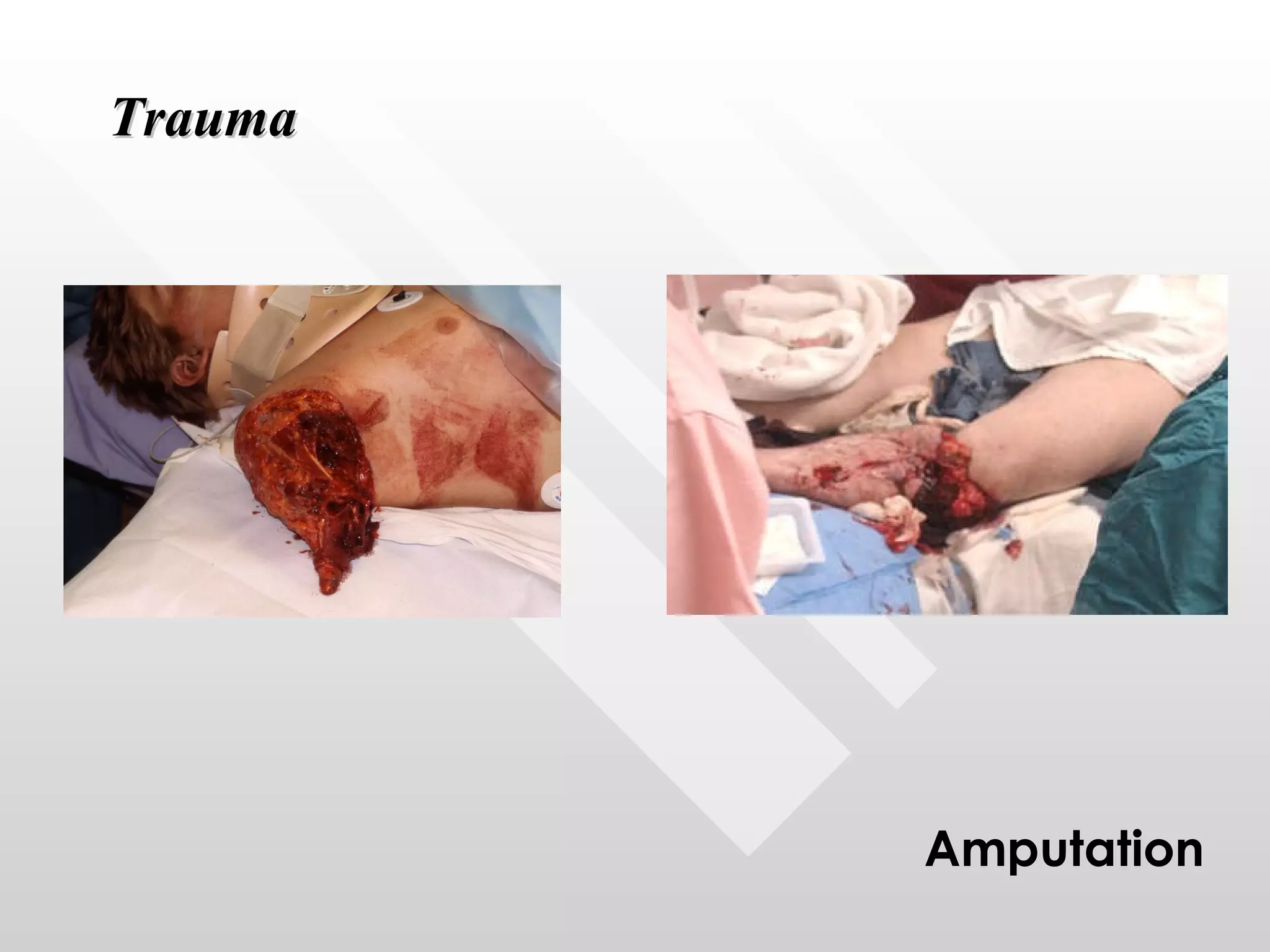
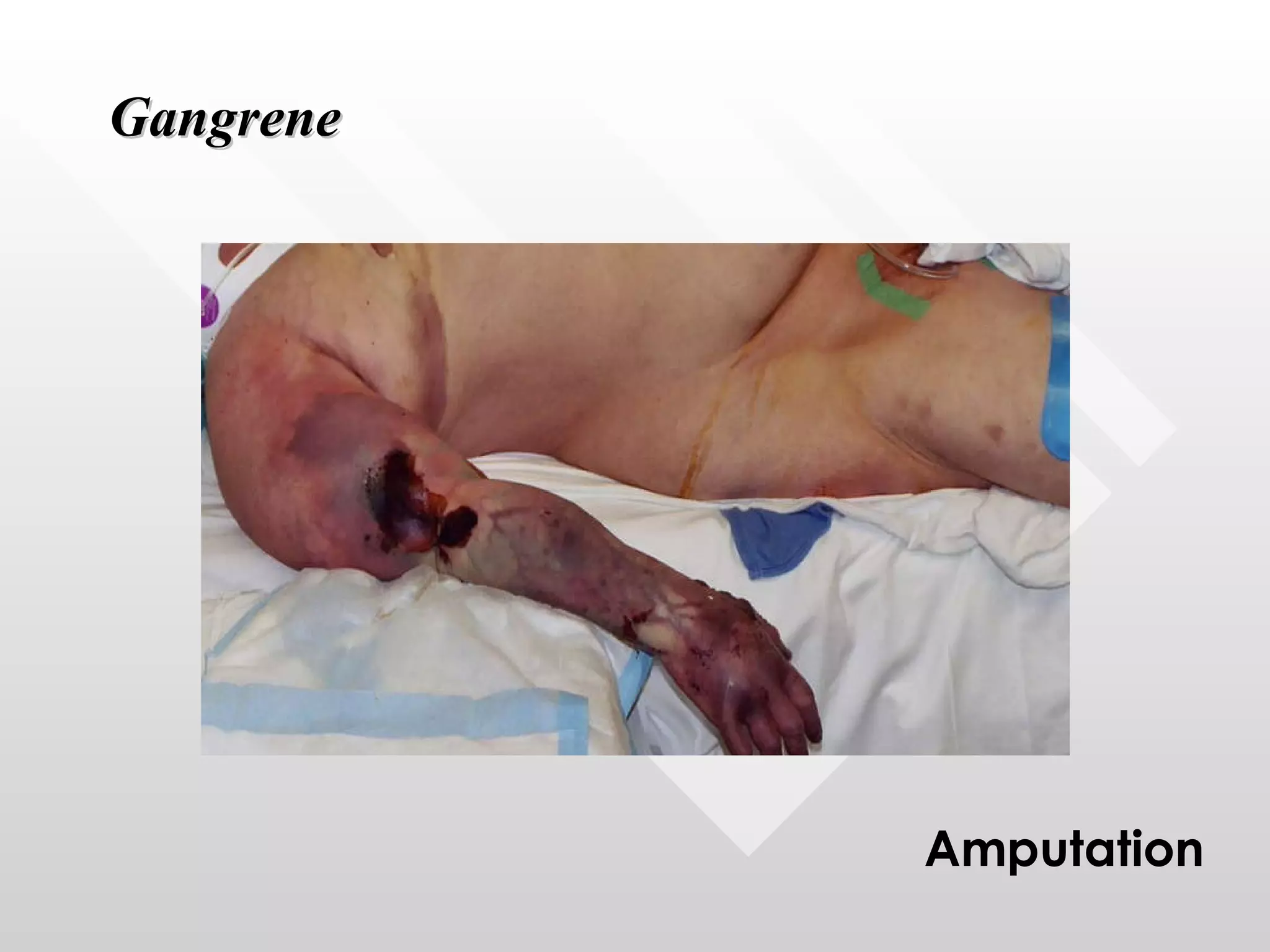
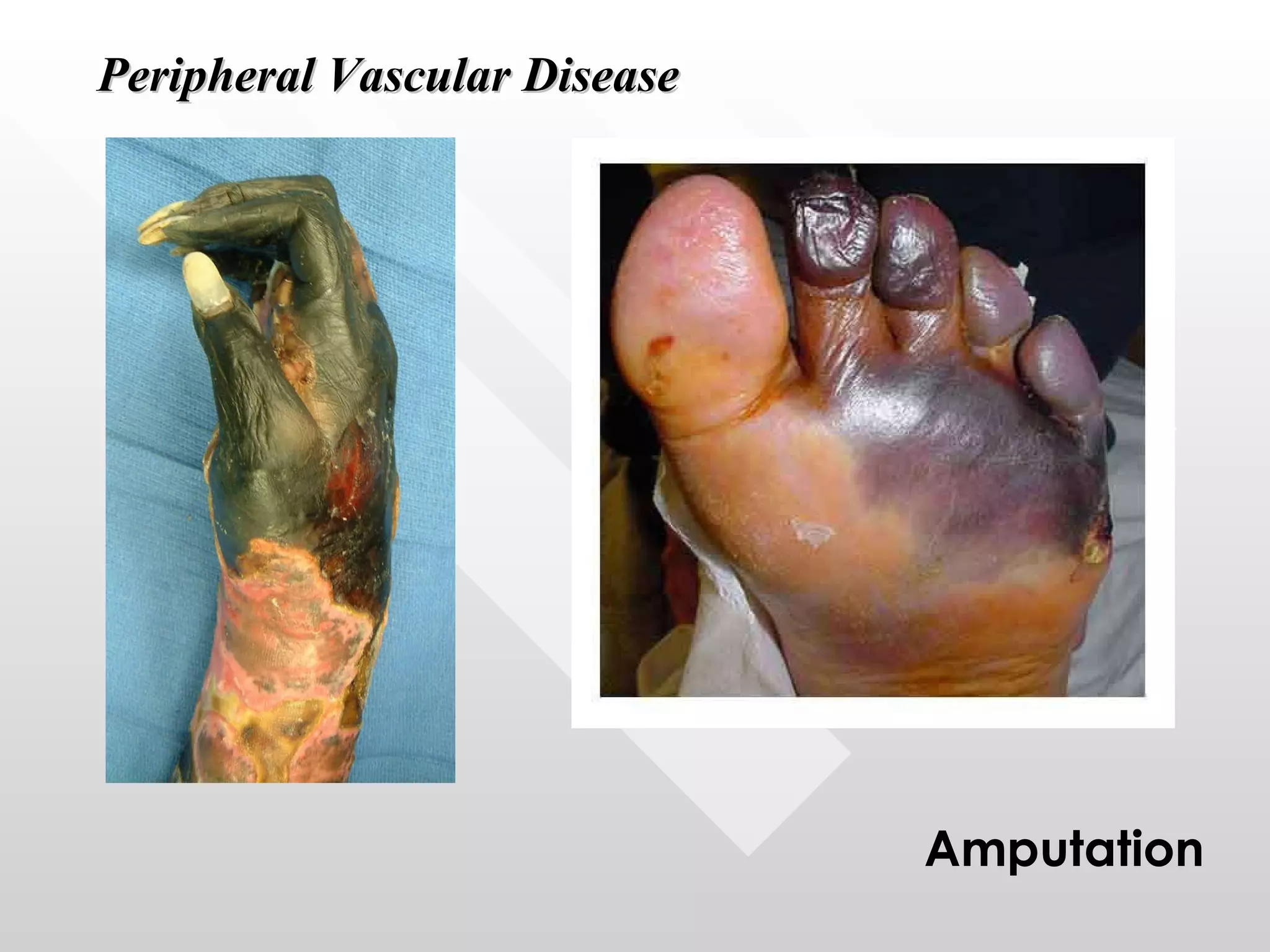
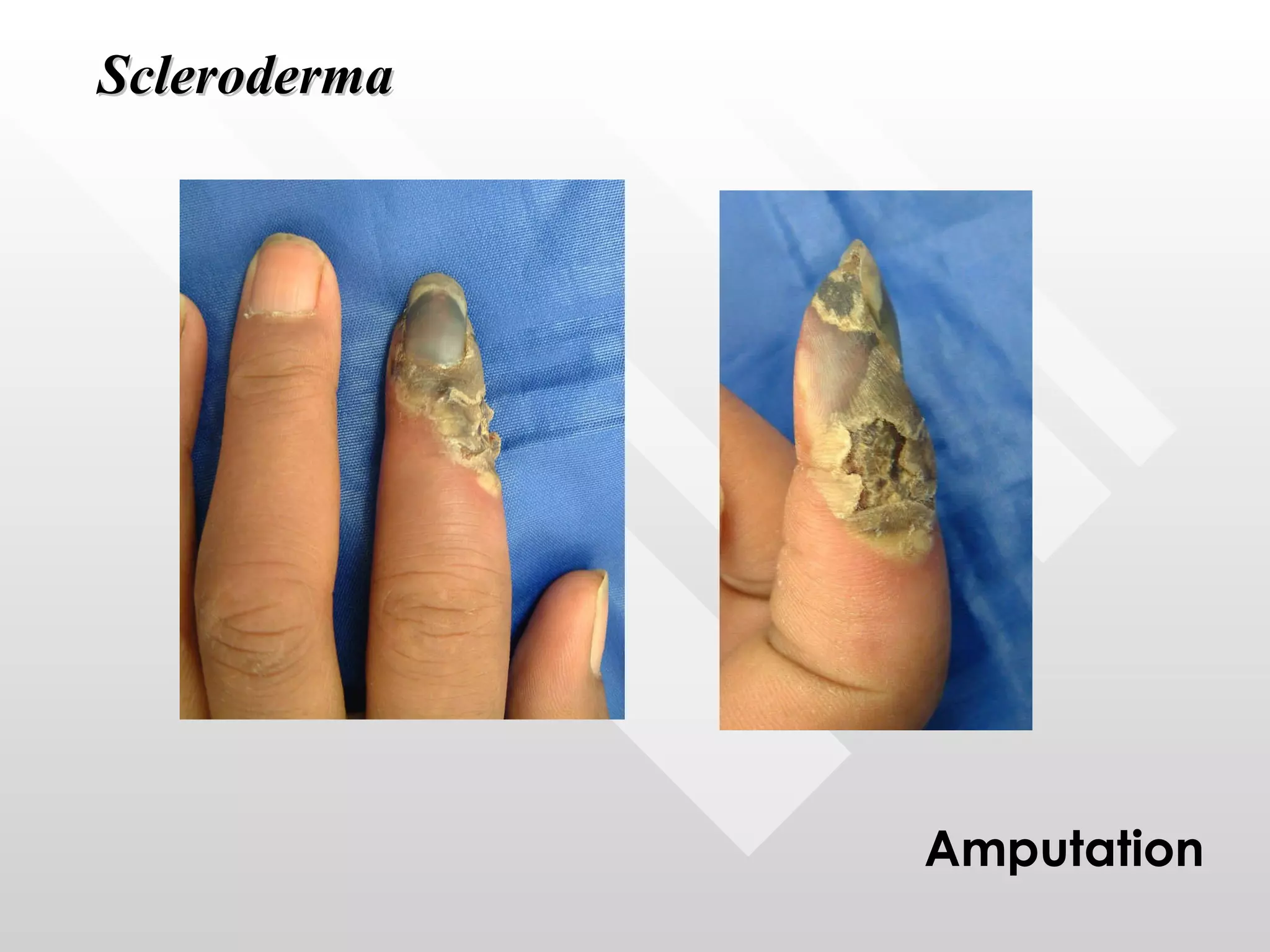
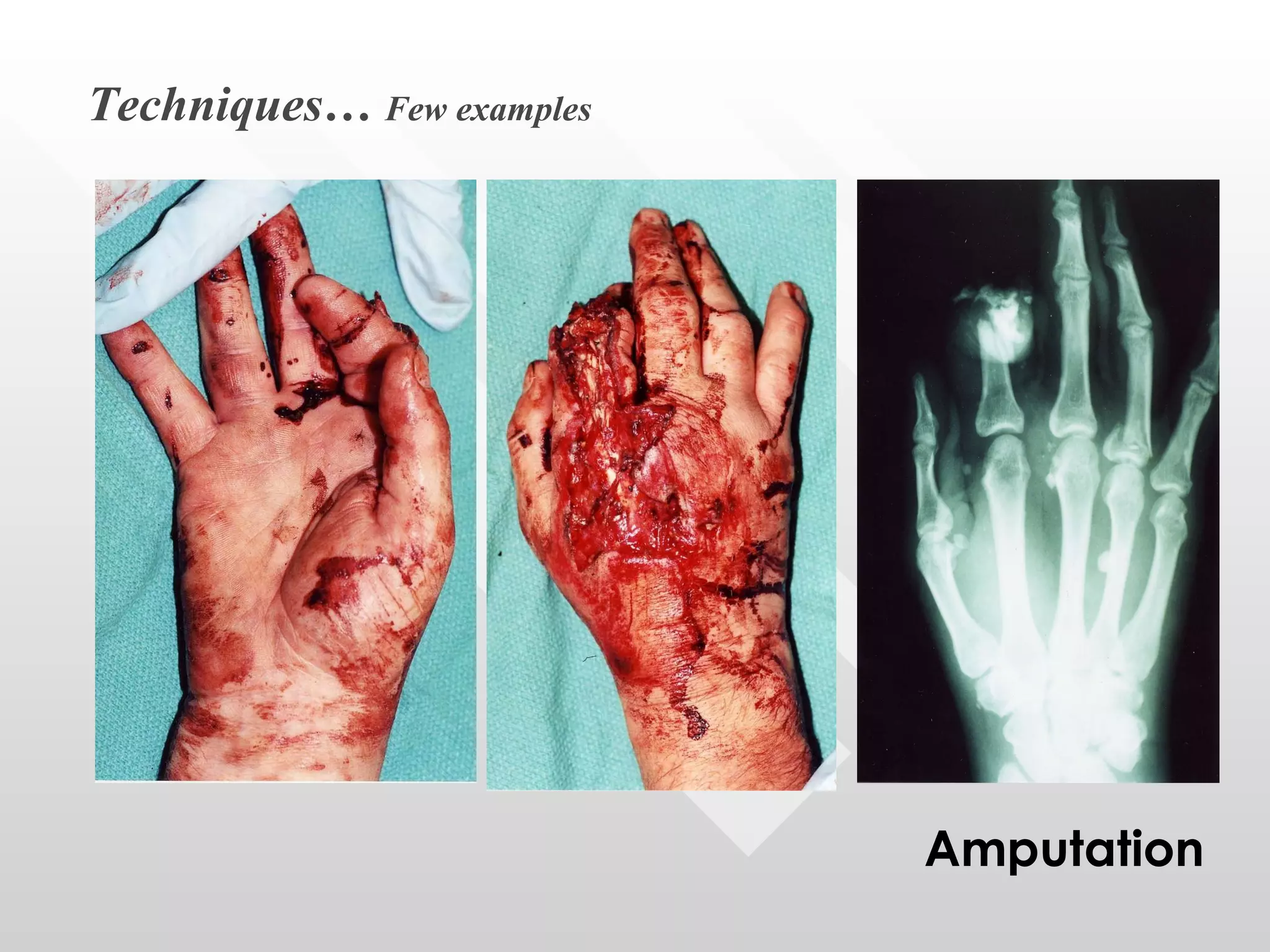
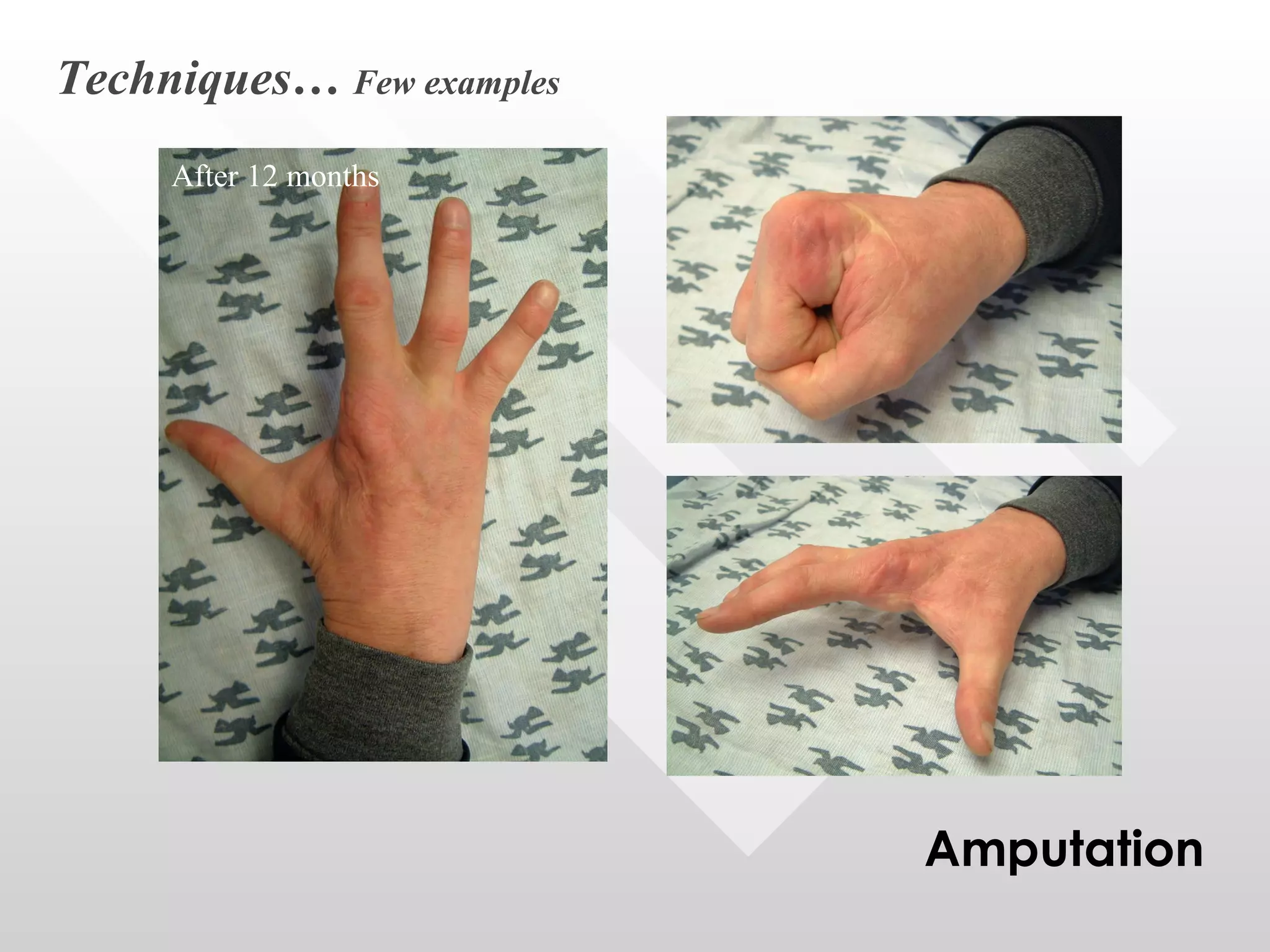
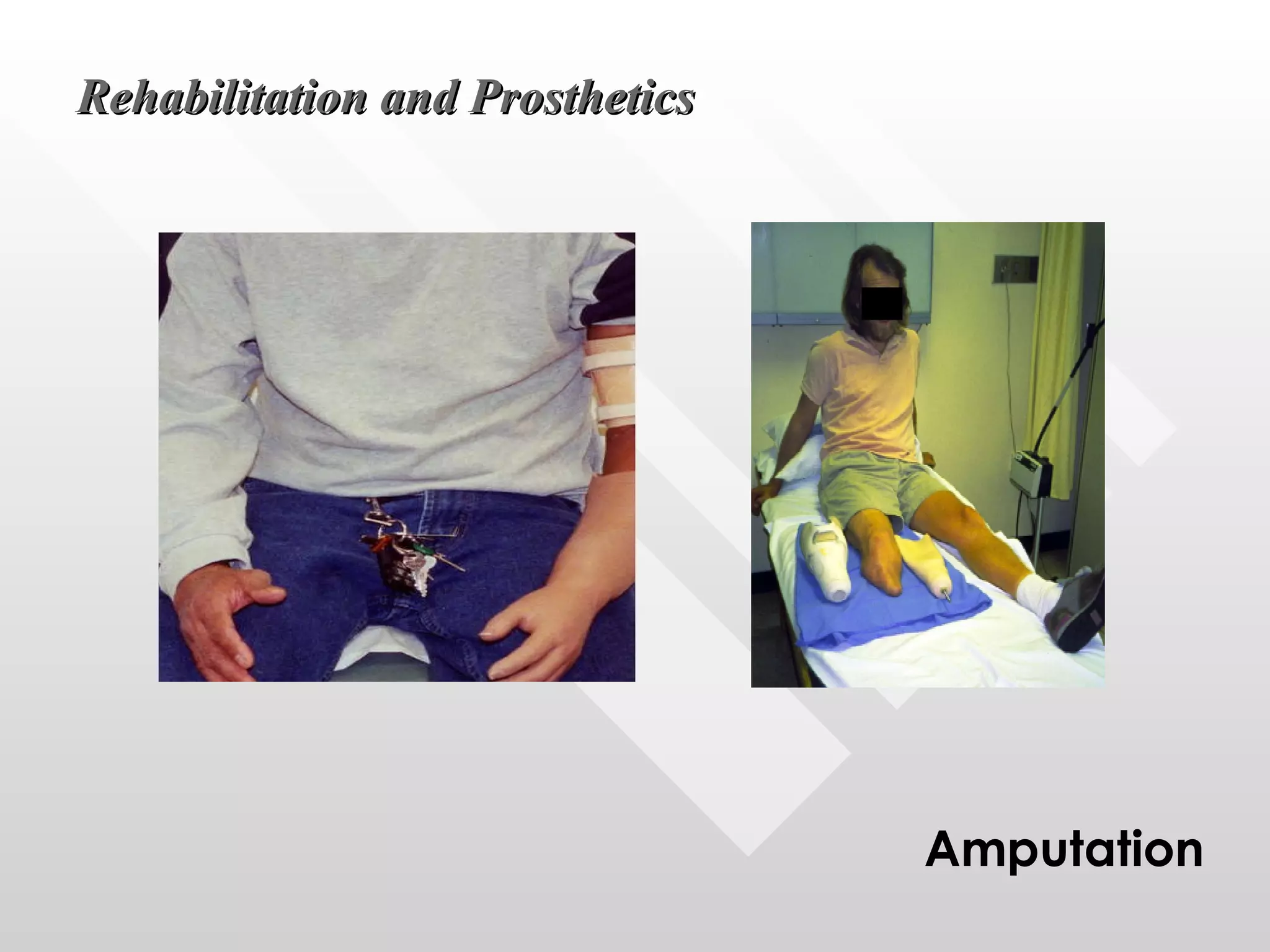
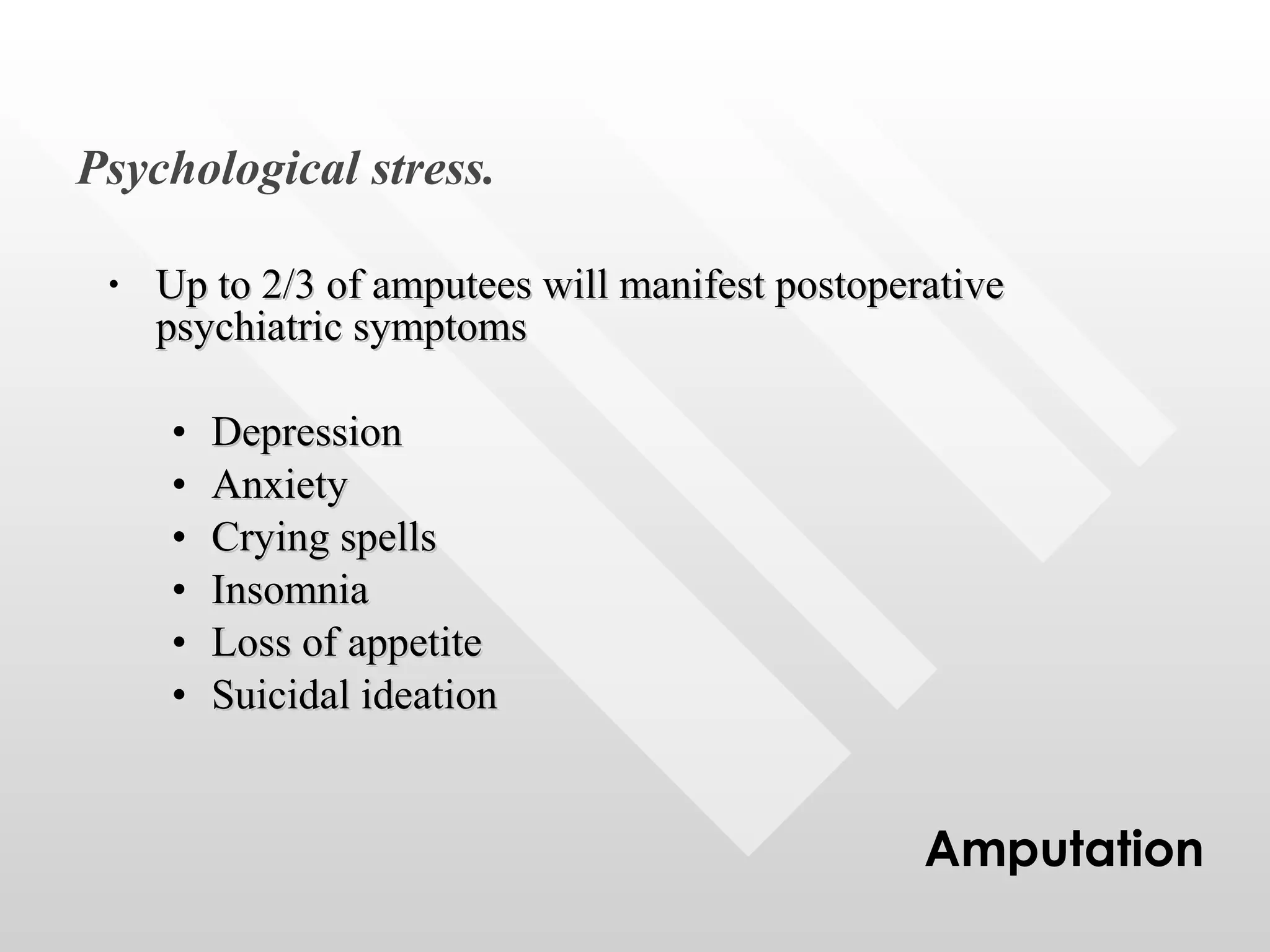
Amputation is the complete removal of an injured or deformed body part. It has been performed since ancient times, often crudely without anesthesia to treat war injuries. Modern amputation techniques focus on debriding nonviable tissue, preventing neuroma formation, achieving hemostasis and wound closure. Postoperative management aims for prompt healing while controlling pain, edema and preventing contractures through rehabilitation and sometimes prosthetics.