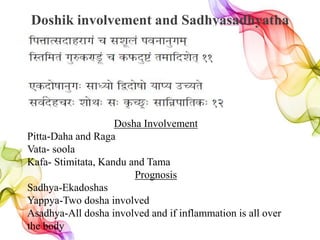
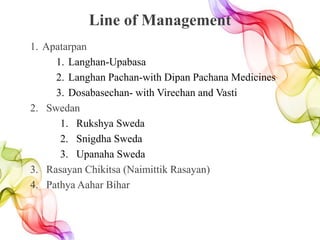
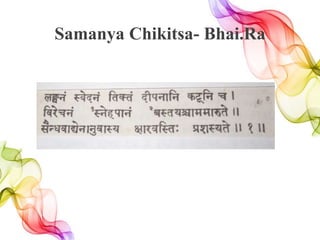
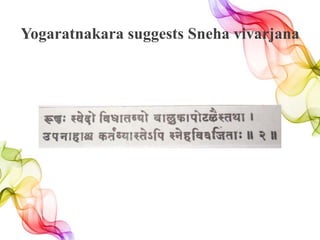
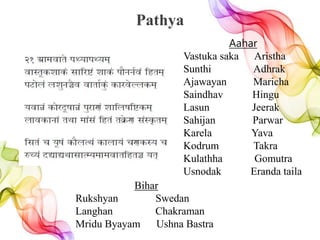
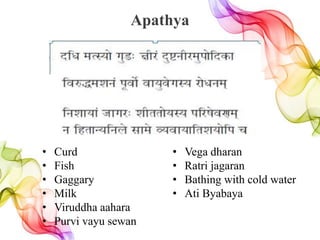
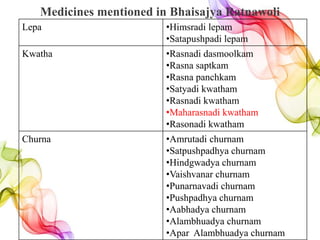
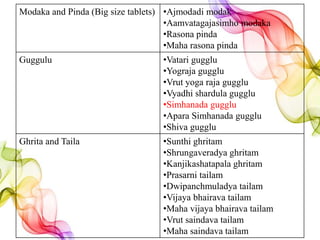
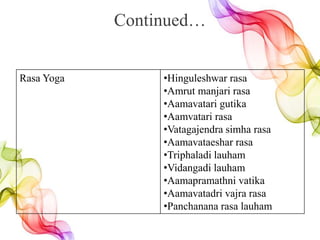
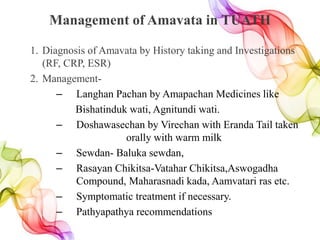
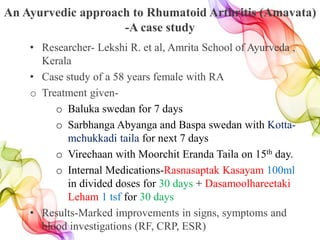
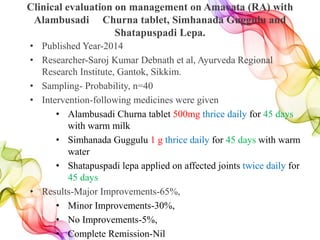
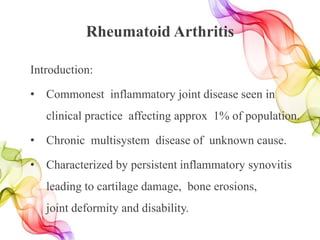
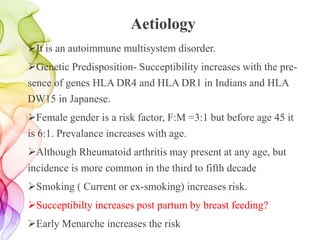
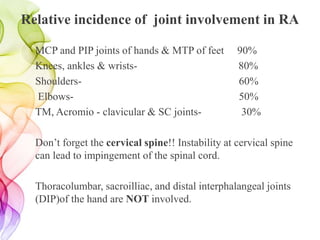
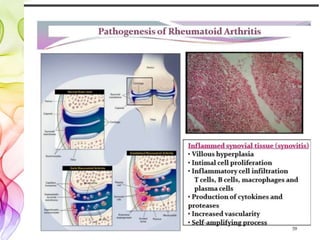
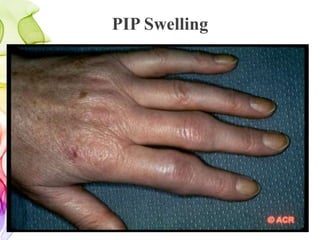
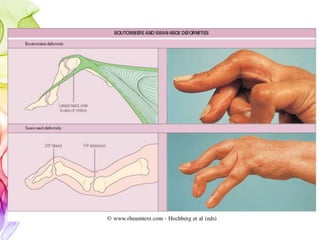
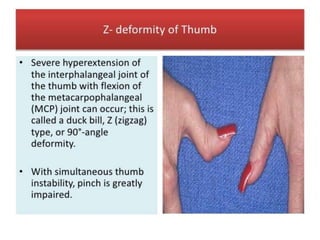
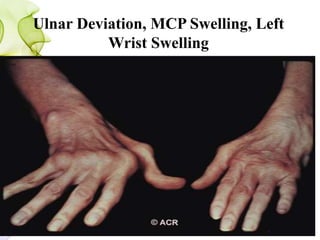
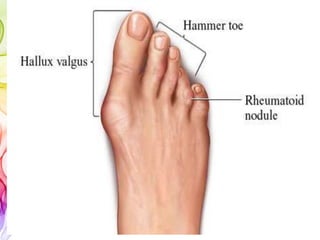
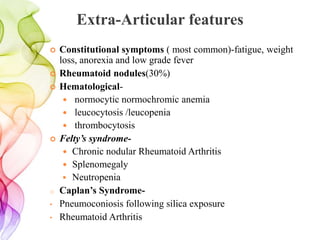
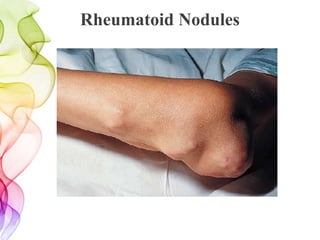
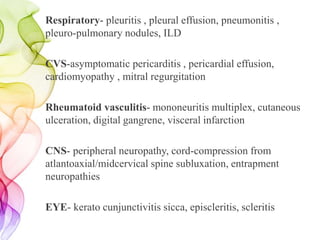
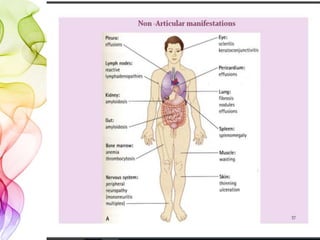
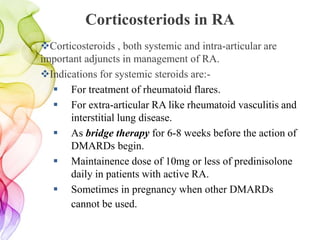
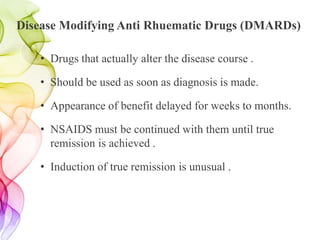
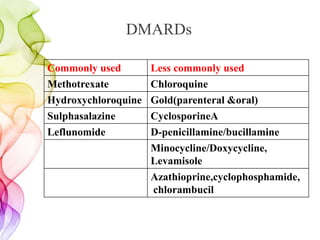
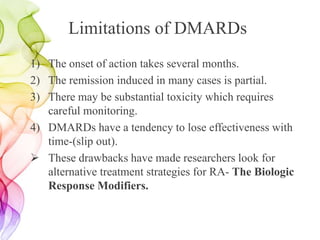
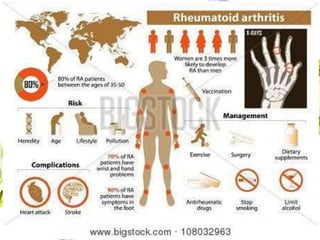
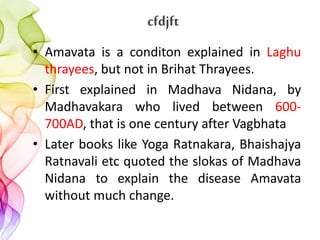
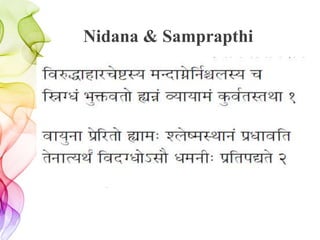
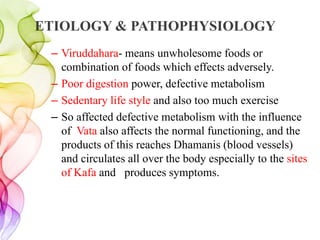
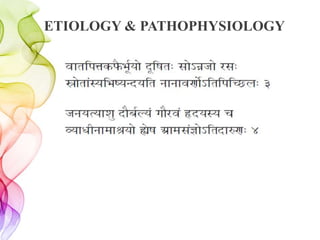
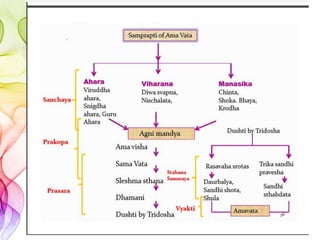
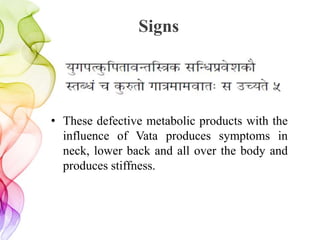
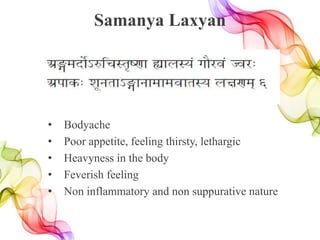
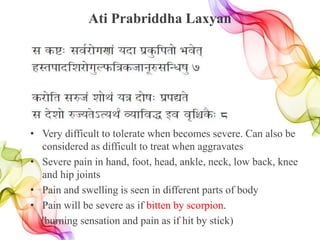
Rheumatoid arthritis is a chronic inflammatory disease that affects the joints, causing pain, stiffness, and swelling. It can lead to long-term joint damage, resulting in disability. The presentation discussed the etiology, pathogenesis, clinical features and management approaches to rheumatoid arthritis from both modern and Ayurvedic perspectives. Key points included that it is an autoimmune disease more common in females, often starts between ages 30-50, involves the small joints of the hands and feet, and can have extra-articular features like rheumatoid nodules. Ayurveda correlates it with the condition of Amavata and emphasizes management through langhan, shodhan, swedan, rasayana and lifestyle modifications
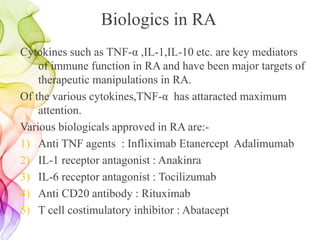
![Nirukti
cfd+ r jft+cfdjftd. -laho/lIft_
cfd]g;lxtf]jftM cfdjftM.-laho/lIft_](https://image.slidesharecdn.com/aamvata-170818164704/85/Amavata-3-320.jpg)
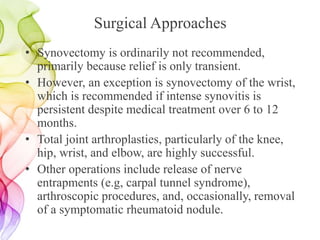
![Complications
Yogaratnakar added Grahani as a complication
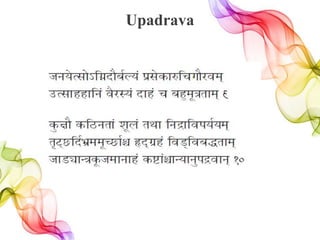
Hfgo]T;f]˜lUgbf}a{No+k|;]sf?lruf}/jd.
pT;fxxflg{ j}/:o+ bfx+ r ax'd'qtfd.
s/f]ltu|x0fLbf]if+ ljz]iffbfd;+1sd .
cjSj+;ht] rfZr+ s]jn+rfdd]j r ..](https://image.slidesharecdn.com/aamvata-170818164704/85/Amavata-14-320.jpg)