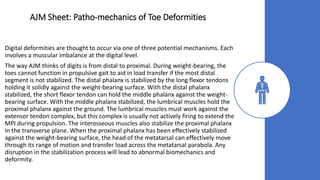
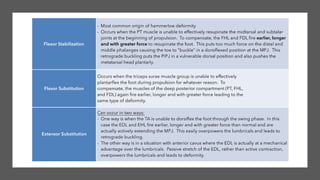
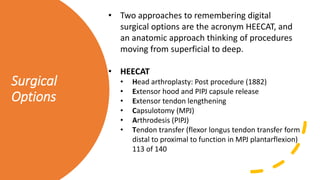
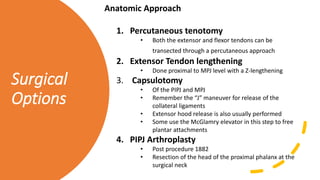
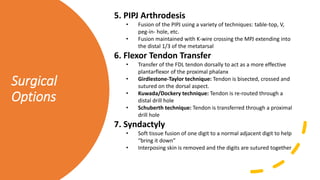
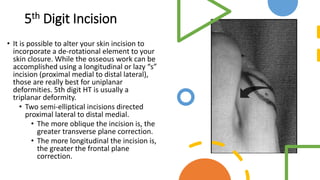
The document provides guidance on evaluating and treating lesser toe, lesser metatarsal, and 5th metatarsal deformities. It describes the subjective and objective findings to look for in the history and physical exam. It then outlines the various conservative and surgical treatment options for addressing the underlying biomechanical issues causing these forefoot deformities.



![Complications
• By far, the most common complications are floating
toe, recurrence and transfer lesions caused by
undercorrection and overcorrection. While you can
evaluate the parabola and transverse plane in the
OR with a C-arm, you really can’t appreciate the
sagittal plane.
• Studies have demonstrated that osteoclastic
procedures allowing the distal segment to find their
own plane without internal fixation have the least
occurrence of recurrence and transfer lesions, but
they also have a higher rate of malunion, delayed
union and non-union.
[Derner and Meyr. Complications and Salvage of
Elective Central Metatarsal Osteotomies. Clinics Pod
Med Surg. Jan 2009.]](https://image.slidesharecdn.com/ajmsheet-ffrecon-200517214108/85/AJM-Sheet-Digital-Deformity-Work-up-21-320.jpg)



![AJM Sheet: 5th
Metatarsal
Deformity
Treatment
Surgical
• Exostectomy: Removal of prominent lateral eminence
from 5th met head
• Arthroplasty: Removal of part/whole of 5th met head
• Distal Metatarsal Osteotomies:
• Reverse Hohmann
• Reverse Wilson
• Reverse Austin
• Crawford: “L” shaped osteotomy allows for insertion of cortical
screws
• LODO (Long Oblique Distal Osteotomy): similar to Crawford but
simply oblique
• Read [London BP, Stern SF, et al. Long oblique distal osteotomy of the
fifth metatarsal for correction of tailor's bunion: a retrospective review.
J Foot Ankle Surg. 2003 Jan- Feb;42(1):36-42.] Especially if externing at
Inova!
• Medially-based wedge
• Proximal Osteotomies:
• Transverse cuts
• Oblique cuts
• Medially based wedges](https://image.slidesharecdn.com/ajmsheet-ffrecon-200517214108/85/AJM-Sheet-Digital-Deformity-Work-up-28-320.jpg)
