1. Acute pyelonephritis is a sudden, severe bacterial infection of the kidneys that commonly affects young women. It is caused by bacteria like E. coli traveling from the bladder to the kidneys.
2. Symptoms include fever over 102°F, flank pain, painful or frequent urination, and other urinary symptoms. Risk factors include female anatomy, kidney stones, diabetes, and other underlying conditions.
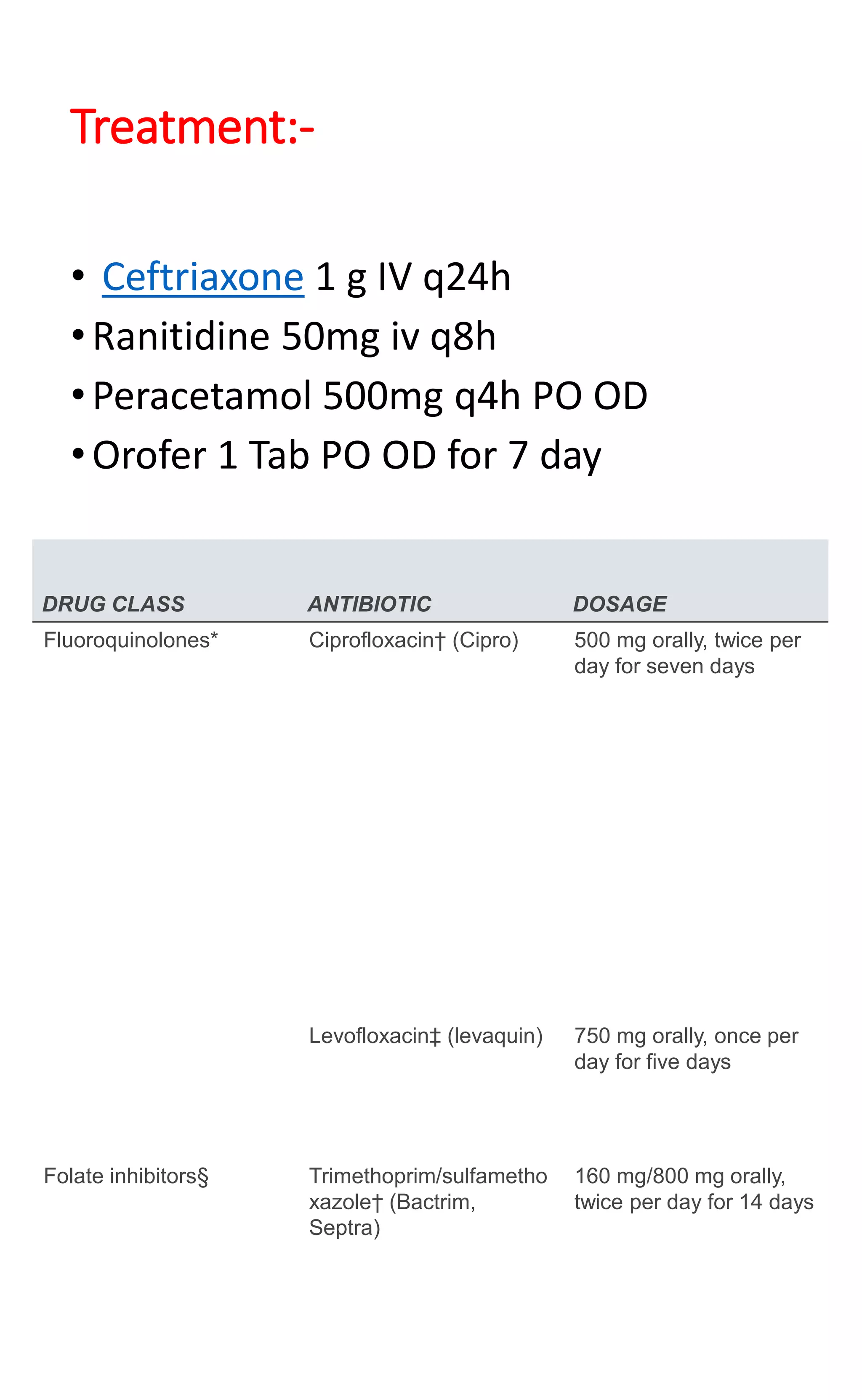
3. Diagnosis involves urine and blood tests showing white blood cells and bacteria. Imaging tests can confirm infection in the kidneys. Treatment consists of intravenous or oral antibiotics like ciprofloxacin or trimethoprim/sulfamethoxazole for 5-14 days.