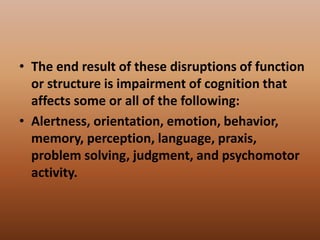
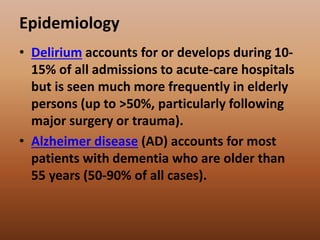
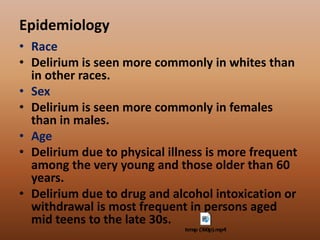
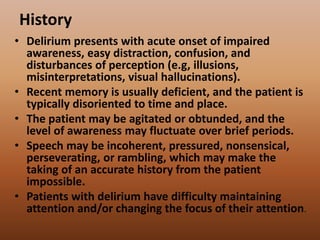
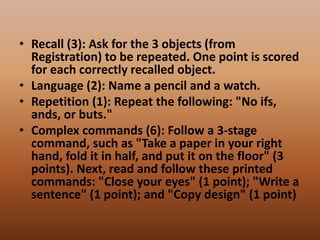
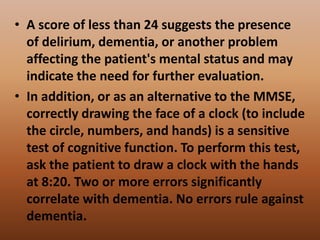
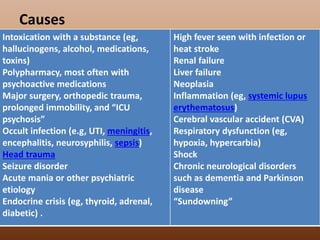
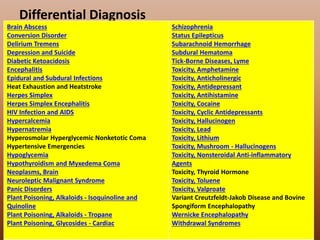
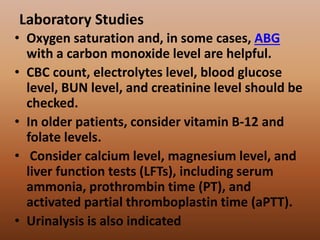
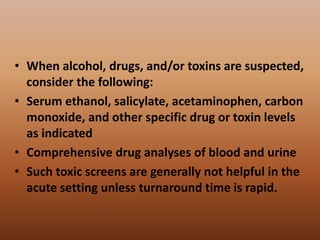
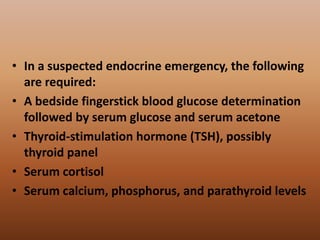
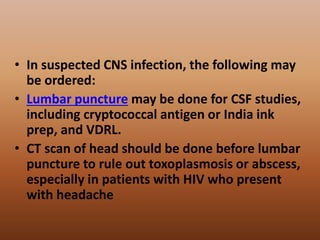
This document provides information about acute confusional state (delirium) including its pathophysiology, epidemiology, history, physical exam findings, assessment tools, causes, differential diagnosis, laboratory and imaging studies, and emergency department care. It describes how delirium involves an acute alteration in mental status due to changes in brain function or structure. Common causes include infection, metabolic disturbances, drugs/toxins, and brain insults. The document emphasizes safety, treatment of reversible factors, and minimizing sedation in delirium management.