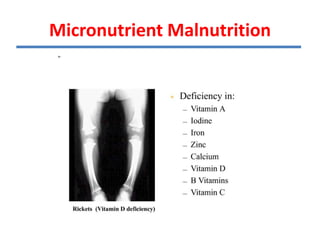
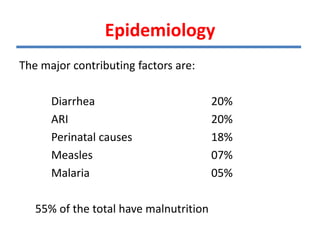
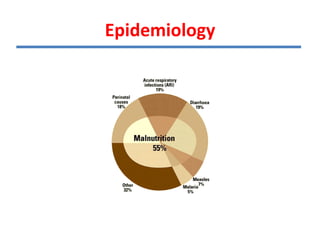
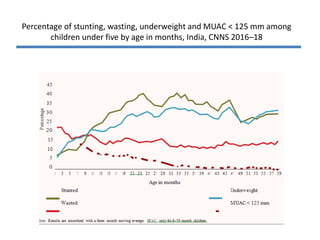
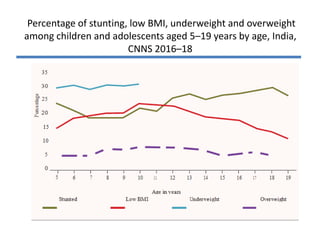
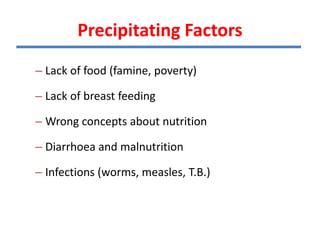
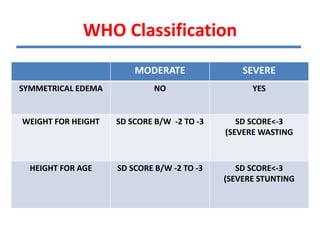
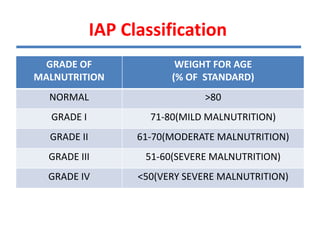
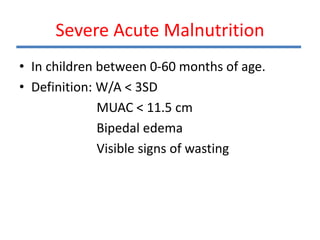
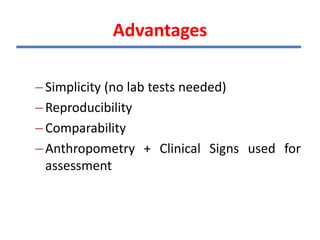
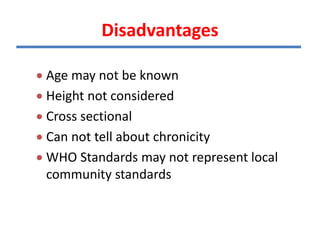
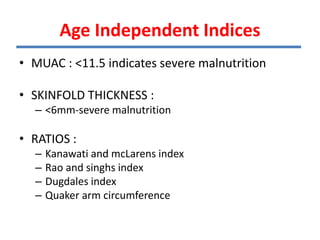
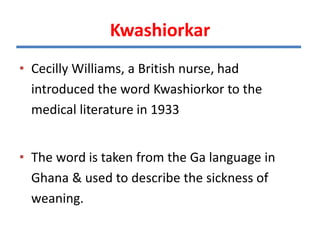
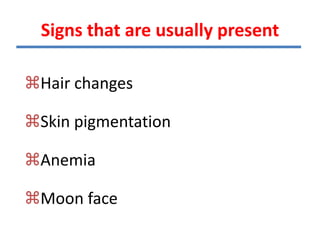
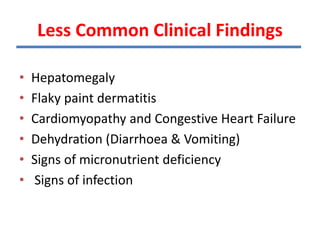
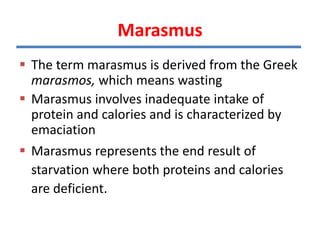
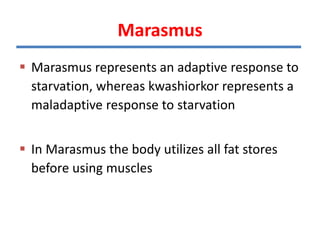
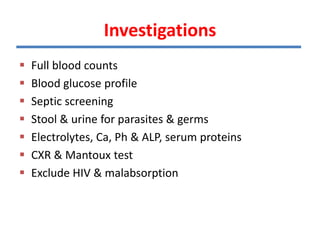
This document discusses malnutrition including definitions of overnutrition, undernutrition, and micronutrient malnutrition. It describes protein energy malnutrition and provides details on etiology, assessment methods, clinical features, worldwide prevalence, and classifications like WHO and IAP. Specific forms of severe acute malnutrition like kwashiorkor and marasmus are explained in terms of etiology, epidemiology, clinical features, and management. Assessment methods covered include clinical exam, anthropometry, laboratory tests, and epidemiological analysis.