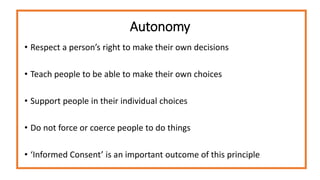
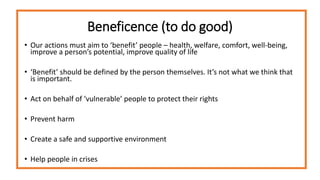
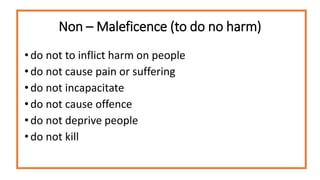
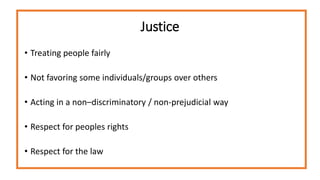
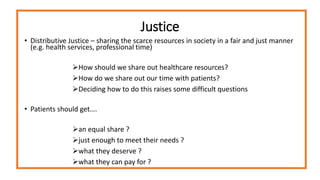
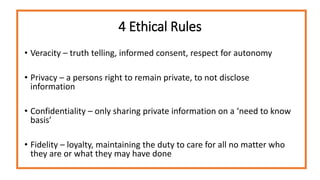
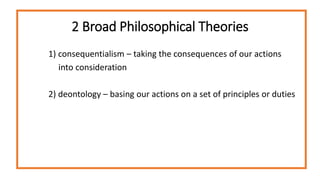
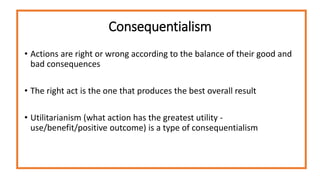
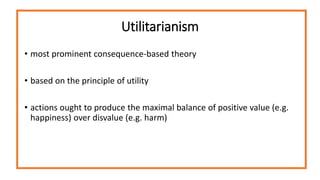
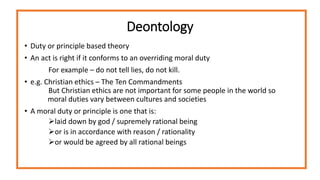
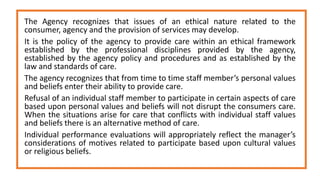
This document provides an introduction to healthcare ethics, discussing key concepts like ethical issues, principles of biomedical ethics, and broad philosophical theories of ethics. It defines an ethical issue as when one has to judge right from wrong in making difficult choices between options. Some major ethical issues in healthcare discussed are respecting patient autonomy, beneficence, non-maleficence, justice, and distributing scarce resources fairly. It also outlines four key ethical principles - autonomy, beneficence, non-maleficence, and justice - and four ethical rules - veracity, privacy, confidentiality, and fidelity. Utilitarianism and deontology are presented as two broad philosophical approaches to ethics.