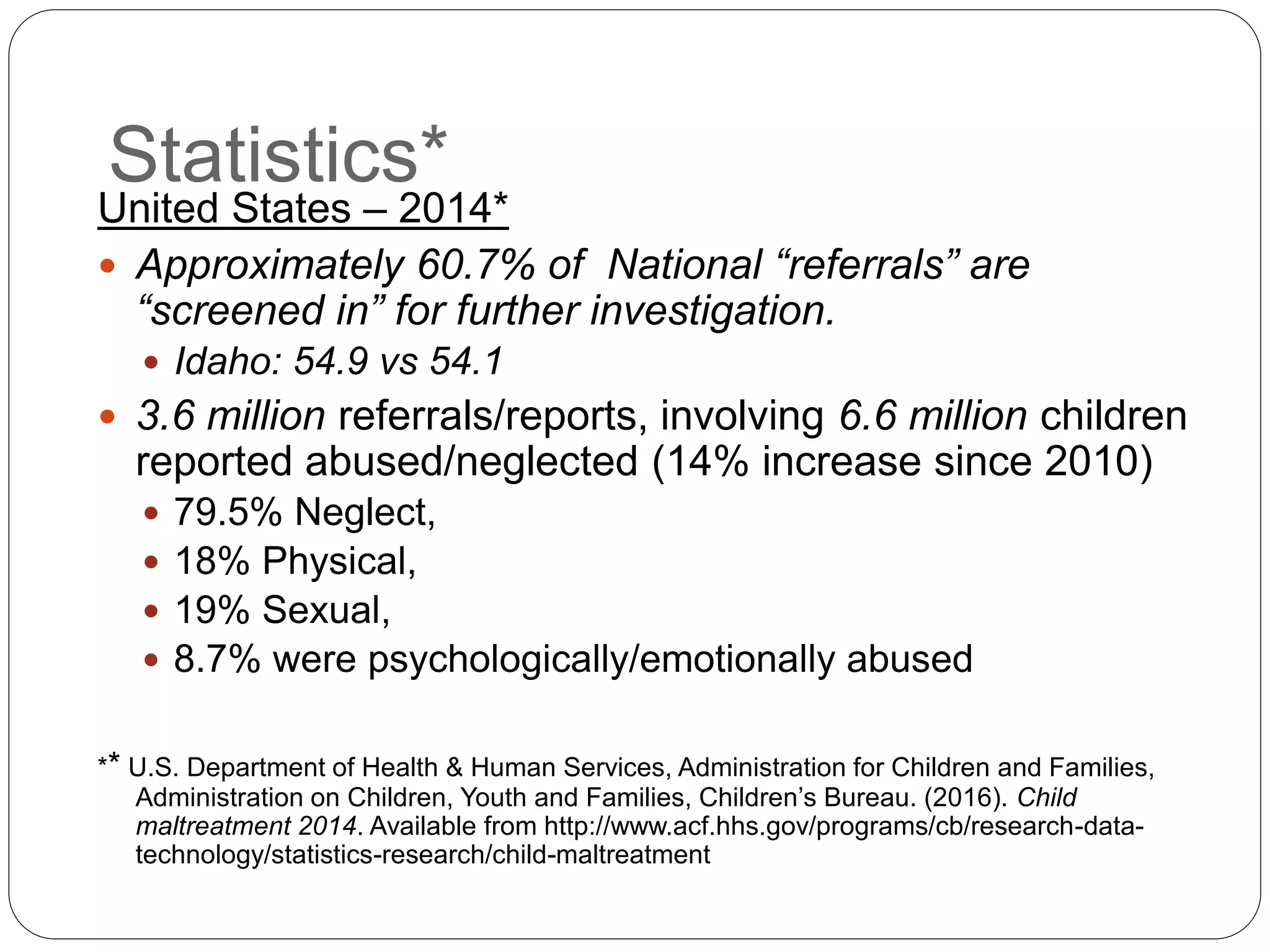
This document discusses child abuse and the role of EMS providers. It begins with definitions of child abuse and outlines the four main categories: neglect, physical abuse, sexual abuse, and emotional abuse. Statistics on child abuse in the US, Idaho, Oregon, and Washington are provided. Risk factors for victims and perpetrators are described. Common injuries associated with different types of abuse are illustrated and explained. The document stresses that all EMS providers are mandatory reporters of suspected child abuse in their states and outlines reporting procedures and protections for reporters. The goal is to help EMS providers recognize and appropriately respond to suspected abuse.