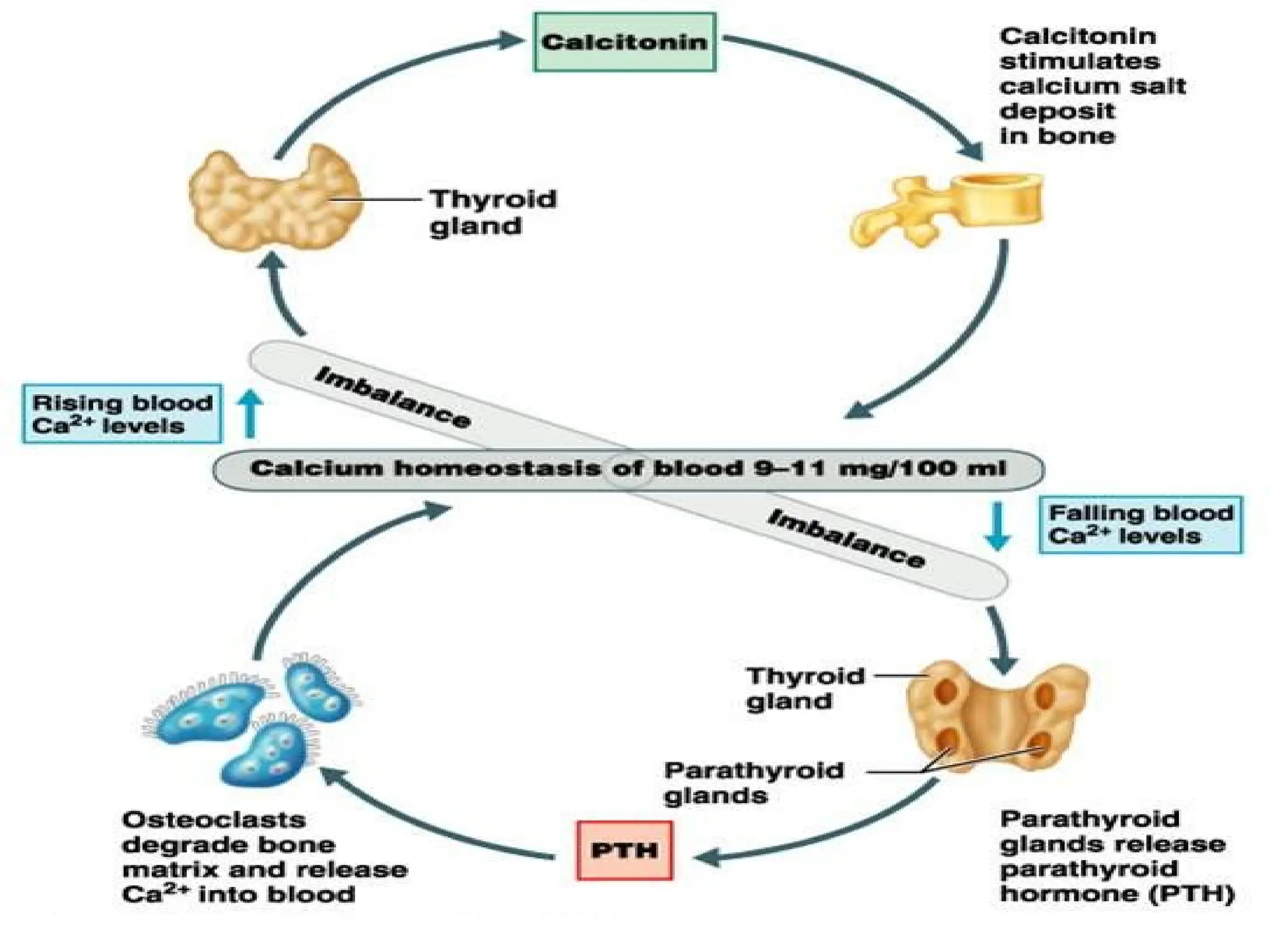
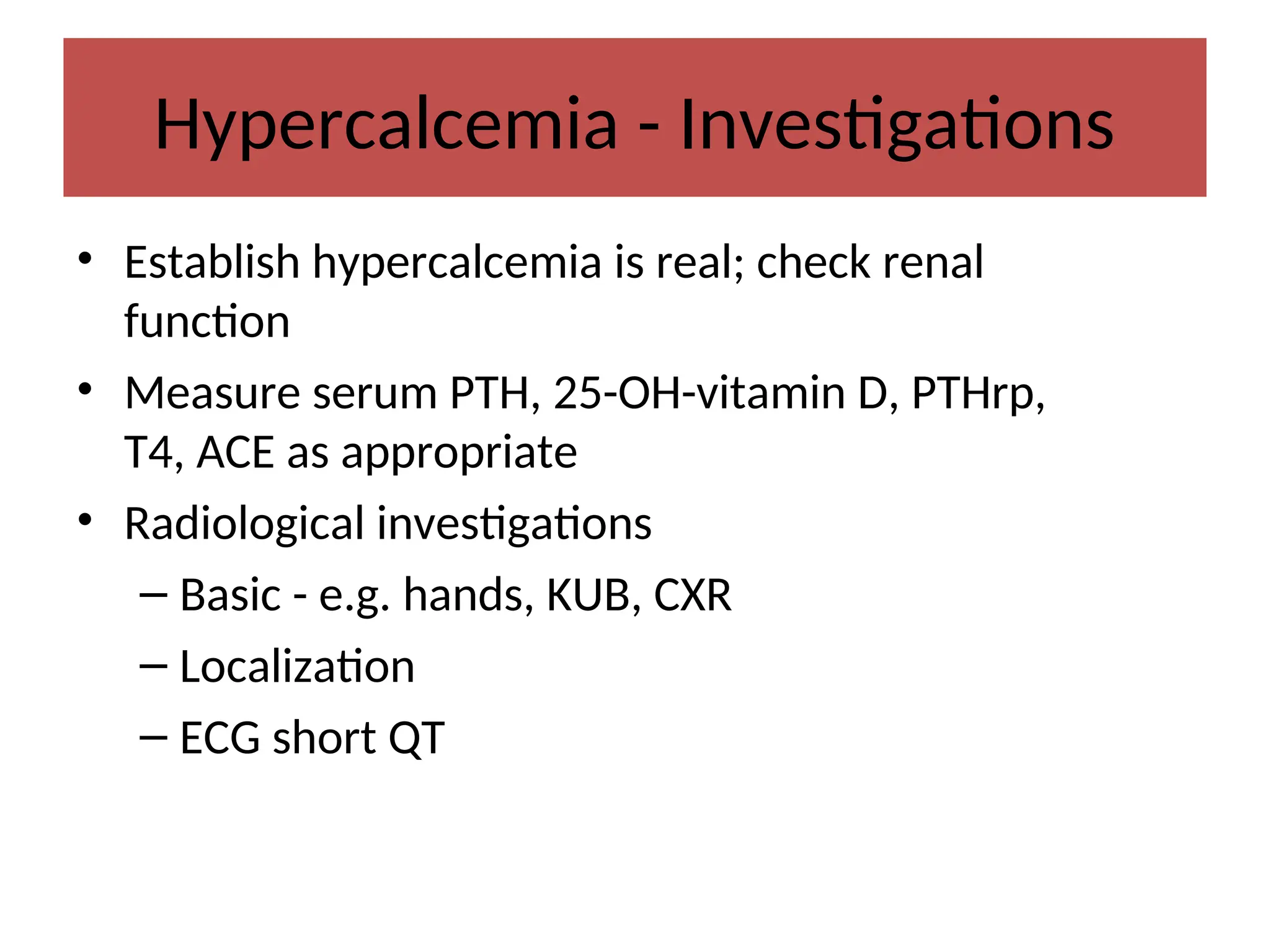
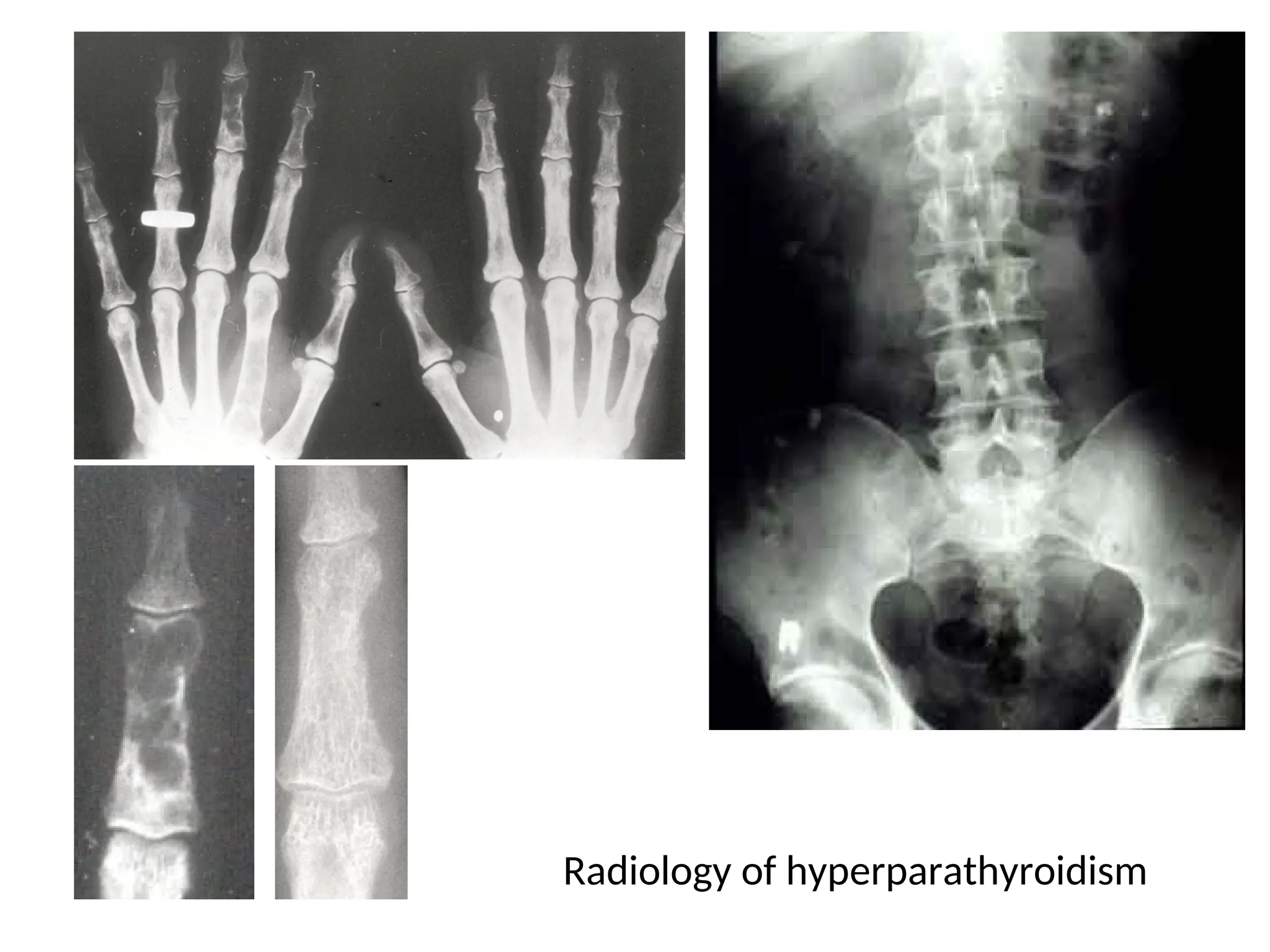
The document details calcium metabolism and its disorders, emphasizing the roles of calcium in bone health, cardiovascular function, and blood clotting. It discusses the regulation of calcium levels in the body, the impact of vitamin D and parathyroid hormone, and conditions related to calcium imbalance, such as hypercalcemia and hypocalcemia. The document also outlines dietary requirements and the physiological functions of calcium in various forms.





![Different Forms of Calcium
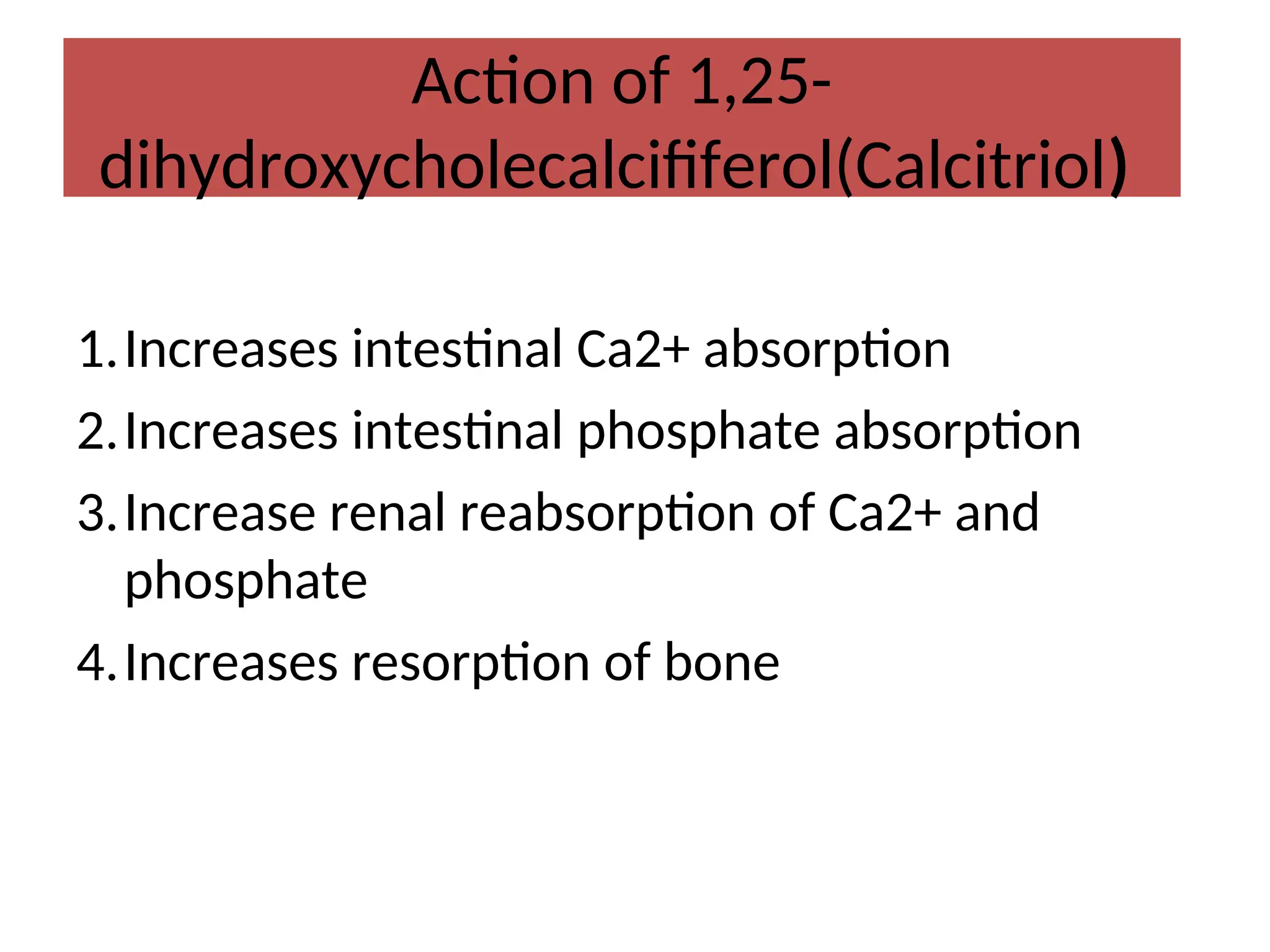
At any one time, most of the calcium in the body exists as the
mineral hydroxyapatite, Ca10(PO4)6(OH)2.
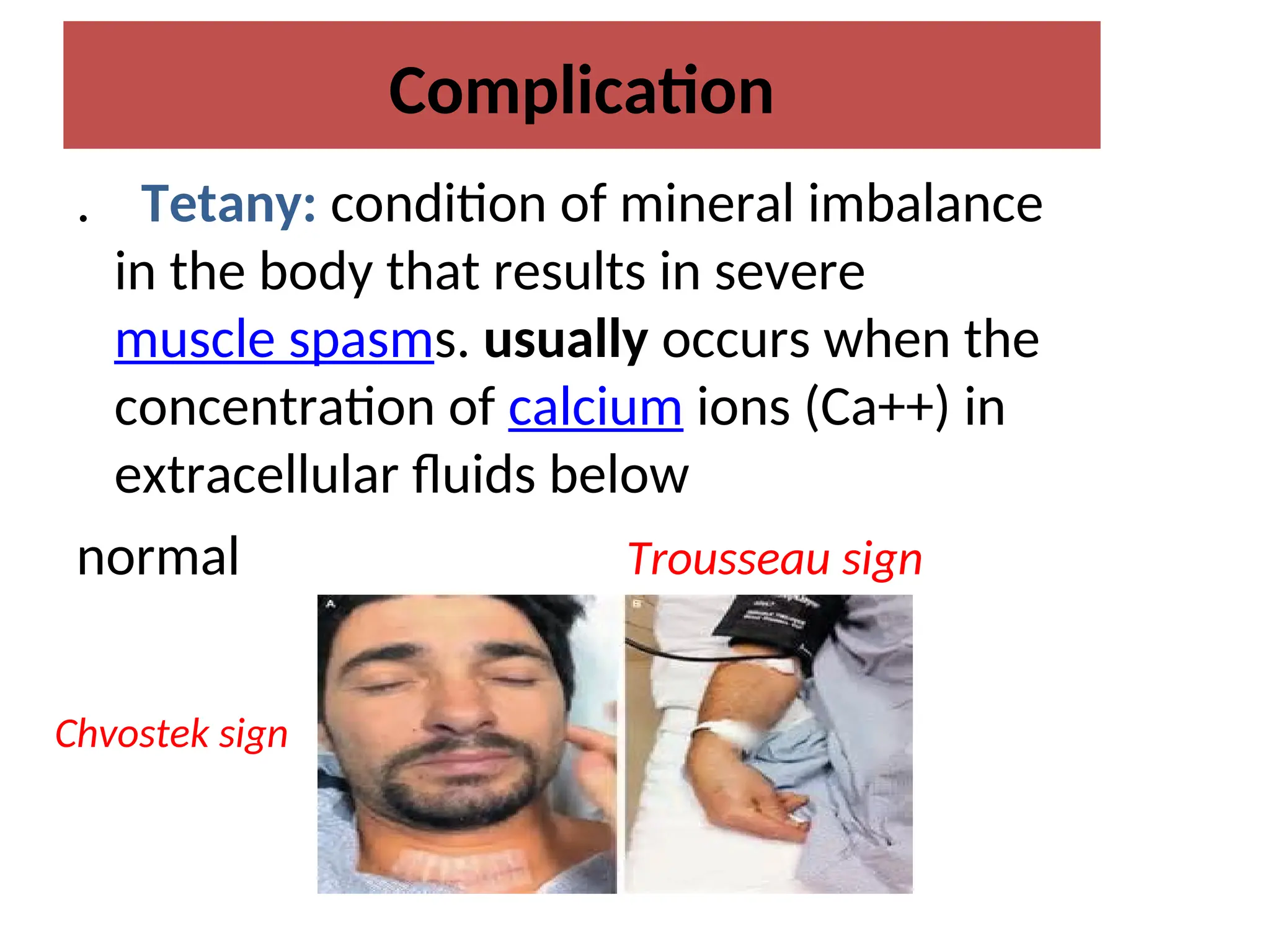
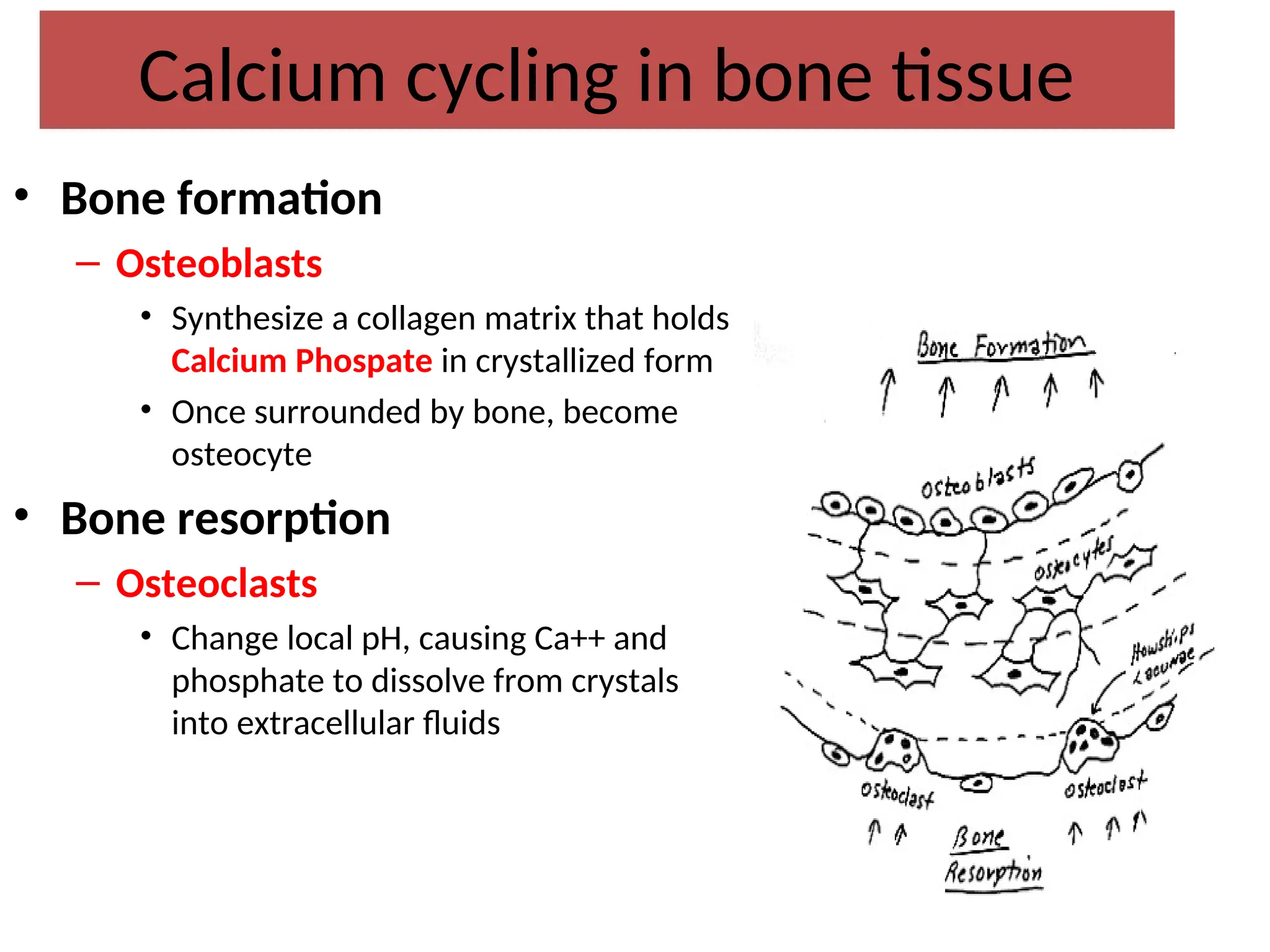
Calcium in the plasma:
45% in ionized form (the physiologically active form)
45% bound to proteins (predominantly albumin)
10% complexed with anions (citrate, sulfate, phosphate)
To estimate the physiologic levels of ionized calcium in states of
hypoalbuminemia:
[Ca+2
]Corrected = [Ca+2
]Measured + [ 0.8 (4 – Albumin) ]](https://image.slidesharecdn.com/1-calciummetabolismdisorders-241120140752-73c83a35/75/1-Calcium-metabolism-disorders-for-students-ppt-7-2048.jpg)


![Regulation of PTH
• Low serum [Ca+2
] Increased PTH
secretion
• High serum [Ca+2
] Decreased PTH
secretion](https://image.slidesharecdn.com/1-calciummetabolismdisorders-241120140752-73c83a35/75/1-Calcium-metabolism-disorders-for-students-ppt-12-2048.jpg)







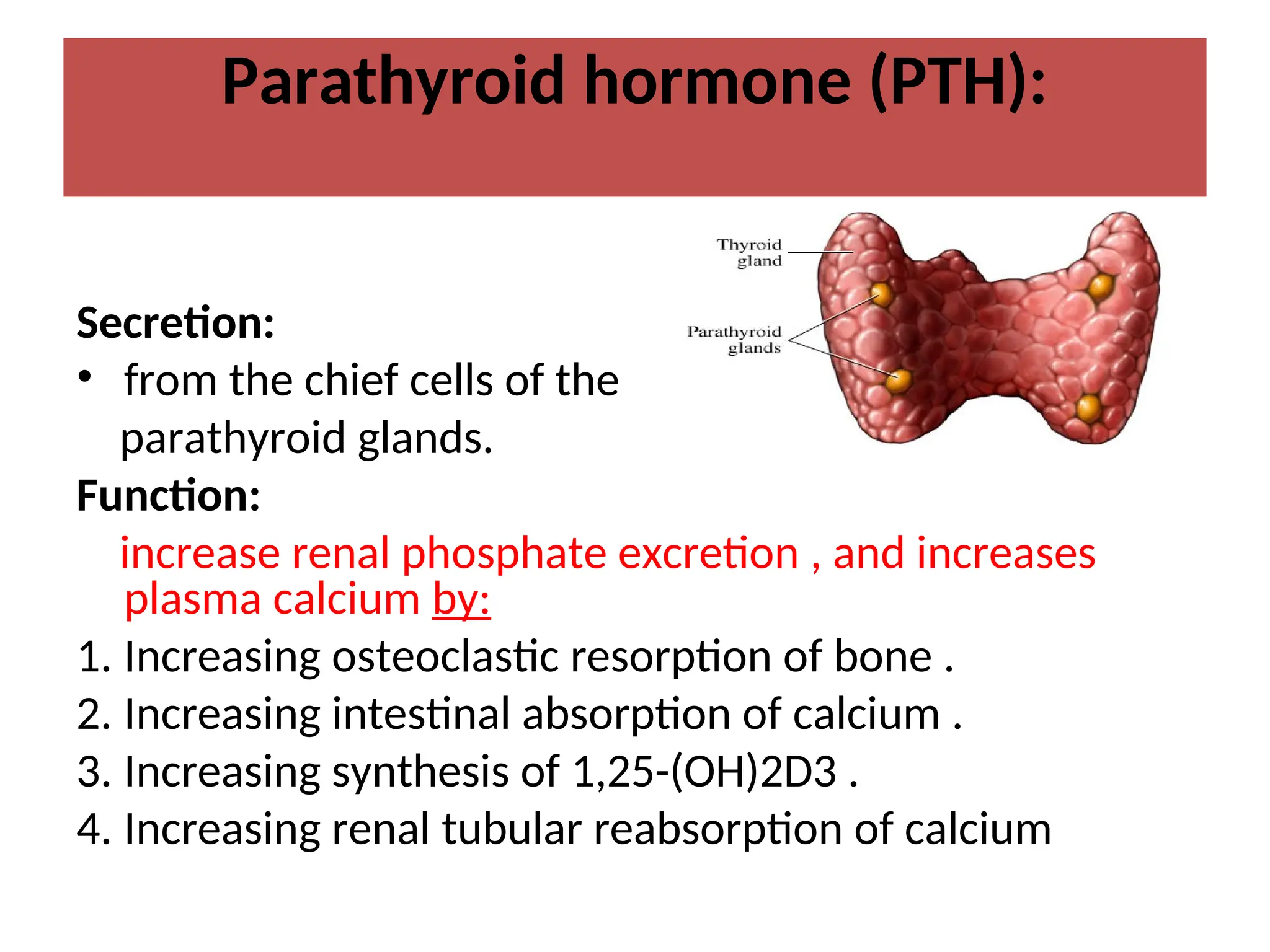
![• Mild hypercalcemia — Patients with asymptomatic or
mildly symptomatic hypercalcemia (calcium <12 mg/dL
[3 mmol/L]) do not require immediate treatment.
• Moderate hypercalcemia — (calcium between 12 and 14
mg/dL [3 to 3.5 mmol/L]) may not require immediate
therapy
• In these patients, we typically treat with saline hydration
and bisphosphonates,
• Severe hypercalcemia — Patients with calcium >14
mg/dL (3.5 mmol/L) require more aggressive therapy.](https://image.slidesharecdn.com/1-calciummetabolismdisorders-241120140752-73c83a35/75/1-Calcium-metabolism-disorders-for-students-ppt-25-2048.jpg)