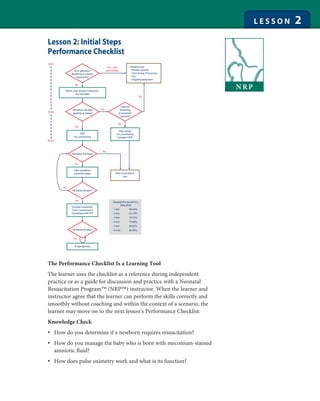
This document provides guidance on performing initial steps of newborn resuscitation. It includes:
1) A performance checklist that guides assessment and intervention based on factors like breathing, heart rate, and tone.
2) Target oxygen saturation levels by age to guide use of supplemental oxygen.
3) Sample scenarios walking through assessing an infant at birth and performing appropriate initial steps or resuscitation based on conditions. The document is intended to help learners practice newborn resuscitation skills.
![Initial Steps of Resuscitation
66
Learning Objectives
Identify the newborn who requires initial steps of resuscitation.
Demonstrate correct technique for performing initial steps,
including decision making for a baby born with meconium-stained
amniotic fluid.
Demonstrate correct placement of oximeter probe and
interpretation of pulse oximetry.
“You are called to attend a cesarean birth due to breech presentation.
How would you prepare for the birth of this baby? As you work, say
your thoughts and actions aloud so your assistant and I will know
what you are thinking and doing.”
Instructor should check boxes as the learner responds correctly.
Participant Name:
Obtains relevant perinatal
history
Gestational age? Fluid clear? How many babies? Other
risk factors?
Performs equipment check
If obstetric provider indicates
that meconium is present in
amniotic fluid, prepares for
intubation and meconium
aspiration
Warmer on and towels to dry, Clear airway (bulb
syringe, wall suction set at 80-100 mm Hg, meconium
aspirator), Auscultate (stethoscope), Oxygenate (checks
oxygen, blender, pulse oximeter and probe), Ventilate
(checks positive-pressure ventilation [PPV] device),
Intubate (laryngoscope and blades, endotracheal tubes,
stylets, end-tidal CO2 detector), Medicate (code cart
accessible), Thermoregulate
Option 1: Meconium-stained amniotic fluid, vigorous newborn.
“The baby has been born.”
Sample Vital
Signs Performance Steps Details
Appears term
Respiratory rate
(RR)-crying
Tone-flexed
Completes initial assessment
when baby is born.
Learner asks 3 questions:
• Term?
• Breathing or crying?
• Good tone?
Initial assessment determines whether or not baby will
receive initial steps of resuscitation at the radiant warmer.
Allows baby to stay with his
mother for routine care:
Warm, clear airway if
necessary, dry, stimulate if
necessary, continue
evaluation
“Vigorous” meconium-stained baby is defined by
• Strong respiratory efforts
• Good muscle tone
• Heart rate (HR) 100 beats per minute (bpm)
Assume that a crying baby with good tone has
HR 100 bpm.](https://image.slidesharecdn.com/02pc-140928202202-phpapp02/85/NRP-Lesson-2-2-320.jpg)


