Belgium Country Report: Struggling to break free from the past
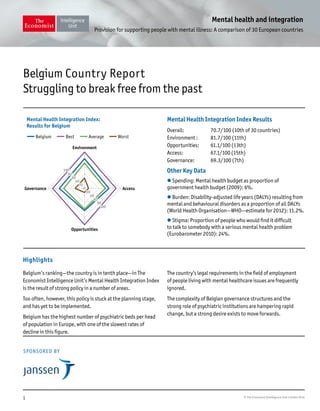
- 1. 1 © The Economist Intelligence Unit Limited 2014 Mental health and integration Provision for supporting people with mental illness: A comparison of 30 European countries Belgium’s ranking—the country is in tenth place—in The Economist Intelligence Unit’s Mental Health Integration Index is the result of strong policy in a number of areas. Too often, however, this policy is stuck at the planning stage, and has yet to be implemented. Belgium has the highest number of psychiatric beds per head of population in Europe, with one of the slowest rates of decline in this figure. The country’s legal requirements in the field of employment of people living with mental healthcare issues are frequently ignored. The complexity of Belgian governance structures and the strong role of psychiatric institutions are hampering rapid change, but a strong desire exists to move forwards. Mental Health Integration Index Results Overall: 70.7/100 (10th of 30 countries) Environment : 81.7/100 (11th) Opportunities: 61.1/100 (13th) Access: 67.1/100 (15th) Governance: 69.3/100 (7th) Other Key Data l Spending: Mental health budget as proportion of government health budget (2009): 6%. l Burden: Disability-adjusted life years (DALYs) resulting from mental and behavioural disorders as a proportion of all DALYs (World Health Organisation—WHO—estimate for 2012): 11.2%. l Stigma: Proportion of people who would find it difficult to talk to somebody with a serious mental health problem (Eurobarometer 2010): 24%. SPONSORED BY Belgium Country Report Struggling to break free from the past Highlights Environment Opportunities AccessGovernance Mental Health Integration Index: Results for Belgium Belgium Best Average Worst 100 100 80 80 60 60 40 40 20 20 0
- 2. 2 © The Economist Intelligence Unit Limited 2014 Mental health and integration Provision for supporting people with mental illness: A comparison of 30 European countries Community care in Belgium for people living with mental illness dates back around 600 years—or at least in does in one town. In the Middle Ages, in the town of Geel a shrine to St Dymphna, patron saint of those with mental illness, attracted numerous pilgrims seeking to be healed. By the 15th century, the pilgrims were housed in a local infirmary at night, but spent the day in the community. As the designated accommodation became too small, the practice of housing individuals with moderate or, in some cases, serious mental illness in local homes as permanent boarders slowly began. It continues to this day: although the number has declined in recent years, several hundred still live with families in the town. Ironically, given this legacy, Belgium’s results in the Mental Health Integration Index have very little to do with current practice in the field of mental health, let alone innovation on the ground. The Index is heavily policy based, because of difficulties in collecting any meaningful data on mental health that are comparable across all countries under study. Accordingly, impressive policy aspirations help Belgium to achieve tenth place overall, and to place as high as seventh in the “Governance” category, which covers a range of issues. However, a closer examination of how well these policy have been implemented yields another picture. Red flags for Belgium include the second-highest suicide rate in Europe and a high and growing rate of involuntary commitment to psychiatric hospitals.1 As Piet Bracke, president of the European Society of Health and Medical Sociology, notes, “if you start to talk about mental healthcare as an integrated system with a focus on community integration and recovery, the [Index] result comes as a surprise. Belgium is really lagging behind.” A system largely mired in the past (I) Hospital-dominated provision. The most striking feature of mental health provision in Belgium is how small an impact, compared with other European countries, the psychiatric reform process has had. The country ranks 18th overall in the “Deinstitutionalisation” category, but, as elsewhere, an official policy of seeking to reduce hospital bed numbers saves it from a worse score than one based on performance alone. Belgium’s “mental health policy is very hospital-centred,” says Dr Tom Declercq, lecturer in the Department of General Practice and Primary Health Care at Ghent University. The country’s 175 psychiatric hospital beds per 100,000 inhabitants in 2011( the latest year available) is the highest figure for any European country and well over twice the average for countries in the Index. This, Dr Declercq adds, “is not a good sign of integration”. Worse still, although the number of beds is decreasing, it is doing so much more slowly than elsewhere. Over the two decades before 2011, the rate of hospital beds per head fell by a total of 12%—one of the smallest declines in that period of any country in the Index and, as far as data is available, roughly one-third of the average. Just as telling, since official efforts to reduce these bed numbers began in 1990, not a single psychiatric hospital has closed. In addition to hospitals themselves, the country has 42 specialist psychiatric nursing homes that provide accommodation for those with a mental illness who are in a stable condition. The result of early attempts to reduce psychiatric hospital bed numbers and provide a stepping stone toward the community, these institutions nevertheless resemble the hospitals that they are supposed to replace. 1 Belgian Health Care Knowledge Centre, Performance of the Belgian Health System Report 2012, 2013.
- 3. 3 © The Economist Intelligence Unit Limited 2014 Mental health and integration Provision for supporting people with mental illness: A comparison of 30 European countries Residents are overseen by a psychiatrist, for example, and on average the facilities have slightly over 80 beds, making them much larger than group homes. By comparison, the average number of beds in psychiatric hospitals in the capital, Brussels, is 68 (although it stands at over 200 in the rest of the country). The ambiguity is such that, for a decade, Belgium included these homes when calculating its figure for total psychiatric hospitals beds, a practice that stopped in 2006. (II) A bio-psychosocial-focused, psychiatrist-centred system. The high number of hospital beds reflects a system that remains, says Mr Bracke, “very organised from a biomedical [rather than bio-psychosocial] perspective, with psychiatrists and a diagnosis-and-treatment logic at the core”. Dr Declercq adds that, until very recently, psychiatrists have not typically been involved in structures that require co-operation with other professionals in primary care. Index data illustrate the nature of the system very well. With Belgium’s relatively low spending on mental health—just 6% of total healthcare expenditure—the country predictably has a relatively small number of people involved in the field, ranking 22nd out of 30 in the mental health workforce category. Digging deeper, however, Belgium has a slightly above-average number of psychiatrists—17 per 100,000, placing it 13th in the Index— but comes 25th for the number of specialist social workers, 29th for psychologists, and last for mental health nurses. This is no accident. A recently-passed law means that, for the first time, psychotherapy is to be recognised as a medical profession—however it will not come into force until 2016. Previously, the field was entirely unregulated and most health insurance paid for psychotherapy only if conducted by a psychiatrist. Dr Declercq says that “psychotherapy is now a real job that is respected, well-defined, and secure”. He hopes this will also lead to greater willingness by insurers to cover associated fees. This is not to say that community-based care and service facilities are completely lacking. Belgium has a wide variety of these for people living with mental illness paid for by either national or regional authorities. In the Index it receives full points for the existence of home care, family support, and assertive outreach teams. The country also has community mental health centres with multi-disciplinary teams providing a range of assistance, along with other specialist social service teams and sheltered housing. The problem, notes Mr Bracke, “is that compared with residential centres linked to psychiatry, these other efforts are minor”. In some ways, provision is shrinking: consolidation cut the number of mental health centres in the Flanders region by three-quarters, so that there are now only 83 in the country—about two-thirds the combined number of hospitals and nursing homes. More tellingly, when looking at the number of mental outpatient facilities per head, Belgium placed just 22nd (out of the 25 countries for which the Index was able to gather data). An important result of this paucity of facilities, says Dr Declercq, “is a far greater demand for help for people with psychiatric problems in the community than we are able to meet.” Extensive waiting lists exist for community care teams as well as for sheltered accommodation and even psychiatric nursing homes. This drives people inappropriately into hospital care in the first place, keeps people in because of a lack of other options and, with poor care continuity, creates the conditions for a return to hospital. Making matters worse, primary-care physicians are often unaware of psychiatric resources available outside hospitals, or refer patients incorrectly. (III) A workplace culture uninterested in implementing mental health regulation. Employment is another area of Belgian mental health where
- 4. 4 © The Economist Intelligence Unit Limited 2014 Mental health and integration Provision for supporting people with mental illness: A comparison of 30 European countries practice fails to live up to government policy. The country comes in a solid 13th in the “Opportunities” category, with a range of potentially helpful regulations and programmes. For example, employers need to conduct psycho-social risk evaluations; doctors specialising in occupational medicine are supposed to help those who develop a mental illness on their road to returning to work; and health insurers have a legal obligation to help sick workers return to employment. However beneficial these might be, the OECD reports that such regulation is far more likely to be breached than observed. It notes, for example, that employers rarely have ask their in-house health services to help with employee retention or reintegration. Moreover, few “see the benefit of the legally required psychosocial risk assessments, and sanctions for non- compliance with the law are too low to motivate employers”. Similarly, occupational doctors, rather than helping on the journey to recovery, are allowed simply to declare an individual disabled, which is sufficient grounds for that person’s immediate dismissal. Finally, health insurers are, like the rest of the health system, focused on the sickness status of those they cover and “remain quite passive ... despite their legal obligation to assist workers in their return to work”. The barriers to change in a complex landscape Belgium’s problems are well known. One politician anonymously told a researcher in 2009 that “After 20 years of initiatives, the WHO always comes back with the same remarks on the way to organise the mental health system in Belgium.”2 Nor is anyone in the country under any illusions about the need for change. According to Mr Bracke, “the more informed policy makers in the various governments and staff surrounding the cabinets really understand the problem and a lot of people who made their careers in mental health have their fingers on the pulse at the government level. Everyone understands the need for transformation with community integration at the core, but in Belgium things evolve very slowly.” This slow pace of change is partly a function of Belgium’s notoriously complex governing structure. With a federal, three regional, and three language group governments, each with its own delineated powers, any given government can rarely accomplish much on its own. Mental health is no exception. Elements of it are the responsibility of two separate federal and six regional ministers. Moreover, governmental priorities also differ significantly, making concerted action less likely. Flanders has a comprehensive regional mental health action plan for 2010-14 focused on suicide reduction and improving front-line mental healthcare by general practitioners (GPs) and psychiatrists. The French-speaking Walloon government has a declaration stating that it will co-operate in this field with the national government. The latter, meanwhile, lacks an overarching policy plan, but is active in specific projects.3 Within this context, efforts to change course go back several decades. A 1989 report commissioned by the Ministry of Social Affairs called for stable long-term, patients then in psychiatric hospitals to be re-socialised in their own living environments.4 The following year, the federal government issued two royal decrees aimed at “de-hospitalisation”, if not necessarily deinstitutionalisation, by creating legal structures for establishing psychiatric nursing homes and sheltered accommodation. Although now important parts of mental health provision in the country, neither did much to accelerate the slow decline in numbers of psychiatric hospitals beds nor to change the ethos of care away from an institutional base. In 1999, in order to try to speed change, the national government 2 Didier Vrancken et al, “Reconfigurations of the Belgian health sector. An experimentation: The therapeutic projects”, KNOWandPOL Working Paper 10, 2009. 3 Marc Hermanns et al, “The State of Psychiatry in Belgium”, International Review of Psychiatry, 2012. 4 L Groot and J Breda, “Evaluation de la programmation hospitalière. Deuxième partie: soins hospitaliers psychiatriques”, 1989.
- 5. 5 © The Economist Intelligence Unit Limited 2014 Mental health and integration Provision for supporting people with mental illness: A comparison of 30 European countries increased the number of both nursing home and sheltered beds and encouraged greater co-operation between hospital and other care providers. Hospital bed numbers actually increased instead. The federal government could accomplish little more on its own. Early in the last decade, though, the various responsible federal, regional, and community ministers began meeting in the Inter-ministerial Conference for Public Health, which also discusses, among other things, issues of mental health policy. In 2004 it issued a joint declaration calling for the reform of mental healthcare around care circuits and stakeholder networks. This led, from 2005 onwards, to a programme for the establishment of dialogue platforms to bring together all relevant stakeholders in given regions to be able to discuss mental health provision. It also led to a programme of pilot projects to create multi-provider, patient-centred care programmes in this field. These projects began in 2007 and after the first year roughly half (41 of 78) had reached their minimum case load needed to achieve refunding. None, though, have since been scaled up. More recently, Article 107 of the Hospital Act of 2008 changed funding regulations to allow psychiatric hospitals to experiment with the creation of care circuits—groups of shareholder bodies that would work together on projects for the promotion of mental health and prevention of illness; intensive treatment of chronic physical ailments for those also living with mental illness; rehabilitation and social integration; community outreach teams for acute and chronic mental healthcare; and provision of residential facilities that allow an increased level of home-based care. The result was another call for pilot projects, 20 of which are under way. Based on the project proposals, the government hopes to reduce the number of psychiatric hospital beds by 11%. The desired outcome is laudable, but this initiative illustrates another difficulty of bringing about change in Belgian mental healthcare. Along with a panoply of state actors at various levels, the psychiatric hospitals themselves—roughly 85% of which are privately run by non-governmental organisations (NGOs), most related to the Catholic Church—have their own interests. Mr Bracke notes that “these organisations control mental healthcare; it is as simple as that. You cannot understand the structure and institutional components of mental healthcare in Belgium if you see it as under the control of government. It is not. Governments have to negotiate with these organisations.” He adds that these institutions typically deliver high-quality care and are run by very motivated, dedicated people. Nevertheless, “although they are all looking to set up measures to innovate their sector, psychiatric hospitals use their power to channel deinstitutionalisation in ways that do not hurt their own interests”. Rather than challenging this power, Article 107 entrenches it. Funding for any proposed care network comes via a hospital’s voluntary decision to dip into its own budget; the hospital employs and pays for the network co-ordinator; new community outreach teams created are considered part of its service; and the hospital is central to choosing its partners in the local network. A recent academic analysis concluded that “either the influence of psychiatric hospitals over community services will grow within centralised patterns of relations ... [or] mental health service networks will be at risk of dissolving whilst trying to maintain a shared model of governance”5 . 5 Pablo Nicaise et al, “Mental healthcare delivery system reform in Belgium: The challenge of achieving deinstitutionalisation whilst addressing fragmentation of care at the same time”, Health Policy, 2014.
- 6. 6 © The Economist Intelligence Unit Limited 2014 Mental health and integration Provision for supporting people with mental illness: A comparison of 30 European countries The various Article 107 projects were only launched in 2011, so it is too early for any formal evaluation of their success (or lack thereof). Mr Bracke reports that, from what he has heard anecdotally from colleagues and students involved, “there are huge regional variations in the smoothness of the implementation. So far, the work is still about co-ordination. There are a lot of meetings, but at ground-level, at this stage, there has not been much effect.” The Belgian way forward? Looking to the future, it would be all too easy to be pessimistic. Policy by pilot project rarely yields rapid change, especially when the institutions that are supposed to be disrupted are in charge of the process and political power is too diffuse to exert a strong will. Considering the overall picture, however, the cumulative effect of initiatives over the years and the widespread realisation that change is needed allow for some hope. Mr Bracke is positive about the future. “People are ready for reform”, he says. “When I talk to people at various levels, there is a consensus that things are going in the right direction, but only the first steps have been taken.” This, he adds, is consistent with his country’s way of doing things: “Belgium is never the first to jump on a radical transformation. We lag behind a few years and learn from what we see. This can be a good thing.”
- 7. 7 © The Economist Intelligence Unit Limited 2014 Mental health and integration Provision for supporting people with mental illness: A comparison of 30 European countries This study, one of a dozen country-specific articles on the degree of integration of those with mental illness into society and mainstream medical care, draws on The Economist Intelligence Unit’s Mental Health Integration Index, which compares policies and conditions in 30 European states. Further insights are provided by two interviews—with Piet Bracke, president of the European Society of Health and Medical Sociology, and Dr Tom Declercq, a lecturer in the Department of General Practice and Primary Health Care at Ghent University—along with extensive desk research. The work was sponsored by Janssen. The research and conclusions are entirely the responsibility of The Economist Intelligence Unit. About the research
