https://userupload.net/ys137mbkcpak
Workplace health programs are a coordinated and comprehensive set of health promotion and protection strategies implemented at the worksite that includes programs, policies, benefits, environmental supports, and links to the surrounding community designed to encourage the health and safety of all employees.
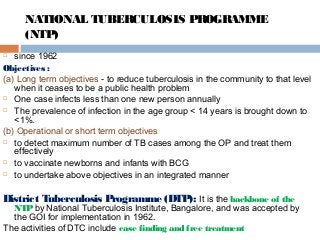
National Health Programmes
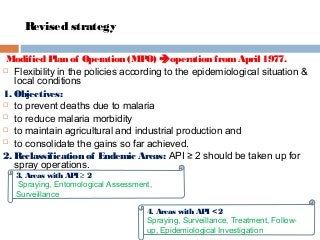
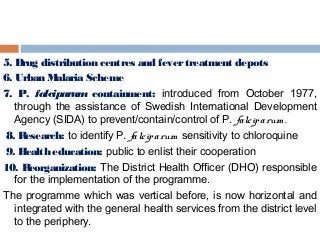
Communicable diseases.
Intellectual Disability related schemes.
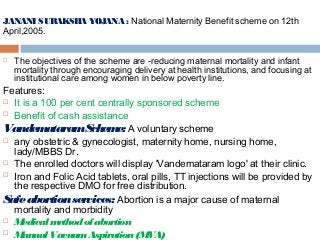
Janani Suraksha Yojana.
Janani Shishu Suraksha Karyakaram.
Mission Indhradhanush.
Pradhan Mantri Swasthya Suraksha Yojana (PMSSY)
National Ayush Mission (NAM)
National Viral Hepatitis Surveillance Programme.






























































![Evaluation
ICDS phase-III
Implementation Completion Report of World Bankassisted ICDS-III/WCDProject Borrower’s
[Government of India] Evaluation Report December2006](https://image.slidesharecdn.com/005-190131061705/85/National-health-programs-of-India-89-320.jpg?cb=1548915602)