Oral cavity malignancy.pptx
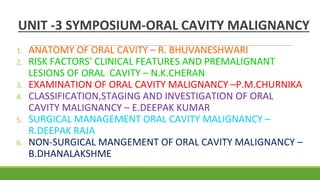
- 1. UNIT -3 SYMPOSIUM-ORAL CAVITY MALIGNANCY 1. ANATOMY OF ORAL CAVITY – R. BHUVANESHWARI 2. RISK FACTORS’ CLINICAL FEATURES AND PREMALIGNANT LESIONS OF ORAL CAVITY – N.K.CHERAN 3. EXAMINATION OF ORAL CAVITY MALIGNANCY –P.M.CHURNIKA 4. CLASSIFICATION,STAGING AND INVESTIGATION OF ORAL CAVITY MALIGNANCY – E.DEEPAK KUMAR 5. SURGICAL MANAGEMENT ORAL CAVITY MALIGNANCY – R.DEEPAK RAJA 6. NON-SURGICAL MANGEMENT OF ORAL CAVITY MALIGNANCY – B.DHANALAKSHME
- 2. ANATOMY OF ORAL CAVITY HOD MAM: DR.BANUREKHA M.S.,D.G.O R.BHUVANESHWARI 3rd UNIT
- 3. ORAL CAVITY It extends from the lips to the oropharyngeal isthmus i.e upto the level of anterior pillar of tonsil. DIVISIONS - Outer part,vestibule - Inner part,oral cavity proper
- 4. VESTIBULE ● Narrow space bounded externally by lips and cheeks, and internally by the teeth and gums. ● It communicates - With the exterior through the oral fissure - With the mouth open , it communicates with oral cavity proper.
- 6. ORAL CAVITY PROPER It is bounded ● anterolaterally : teeth , gums and alveolar arches of the jaws ● Floor : tongue ● Posterior:communicates with pharynx through Oropharyngeal isthmus
- 8. EMBRYOLOGY
- 15. LIPS Lip is composed of ● Skin ● Superficial fascia ● Orbicularis oris muscle ● Submucosa ● Mucous membrane Frenulum of lips : mucous membrane forms median folds that pass from lips to gums. Philtrum:median vertical groove on outer surface of upper lip.
- 18. CHEEKS ( BUCCAE )
- 19. Each cheek is composed of ● Skin ● Superficial fascia ● Buccinator covered by buccopharyngeal fascia ● Submucosa ● Mucous membrane Parotid duct : opens on the inner surface of the cheeks opposite to the crown of the upper second molor tooth. Buccal pad of fat:lies on the buccinator
- 20. ● The cheeks are supplied by buccal branches of the maxillary artery. ● Innervated by buccal branches of the mandibular nerve. ● The lymphatics of the cheek drain chiefly into submandibular and preauricular lymph nodes and partly into buccal and mandibular nodes.
- 21. GUMS ( GINGIVAE ) ● The gums are the soft tissues which envelop the alveolar processes of the upper and lower jaws and surround the necks of the teeth. ● These are dense fibrous tissue covered by startified squamous epithelium. ● Each gum has two parts : - Free part - Attached part
- 23. NERVE SUPPLY OF GUMS UPPER GUMS ● Labial side ● Lingual side LOWER GUMS ● Labial side ● Lingual side Posterior, middle and anterior superior alveolar nerves. Anterior palatine and nasopalatine nerves. Buccal branch of mandibular and incisive branch of mental nerve. Lingual nerve
- 24. LYMPHATIC DRAINAGE OF GUMS ● Upper gums drains into submandibular nodes. ● Anterior part of lower gums drains into the submental nodes. ● Posterior part of lower gums drains into the submandibular nodes.
- 25. RETROMOLAR TRIGONE Triangular area overlying anterior ramus of mandible. Apex: maxillary tuberosity Base: posterior most Molar.
- 26. HARD PALATE Forms roof of the oral cavity. ● Anterolateral margins : continuous with the alveolar arches and gums. ● Posterior margin: gives attachment to soft palate. ● Superior surface : forms floor of the nose. ● Inferior surface : forms roof of the oral cavity.
- 27. SOFT PALATE ● It is a movable, muscular fold, suspended from the posterior border of the hard palate. ● It separtes nasopharynx from the oropharynx. ● The soft palate has two surface - anterior surface - posterior surface
- 28. ● Two borders: - Superior border - inferior border ● Muscles of soft palate
- 30. TONGUE Parts
- 31. Dorsum of the tongue It is divided into ● Oral part ● Pharyngeal part
- 32. Papillae of the tongue
- 33. Inferior surface of the tongue
- 34. Extrinsic muscles of tongue
- 35. Extrinsic muscles Actions ● Genioglossus ● Hyoglossus ● Styloglossus ● Palatoglossus Protrudes the tongue. Depresses the tongue. Retracts the tongue. Elevates the tongue.
- 36. Intrinsic muscles of the tongue
- 37. Intrinsic muscles Actions ● Superior longitudinal ● Inferior longitudinal ● Transverse ● Vertical ● Shortens the tongue makes its dorsum concave. ● Shortens the tongue makes its dorsum convex. ● Makes the tongue narrow and elongated. ● Makes the tongue broad and flattened
- 41. Taste buds The bud is formed by two kinds of cells - supporting cells ( form an outer envelope for the bud ) - Gustatory cells which are chemoreceptors occupy central portion of the bud. The taste receptors are located around the papillae found on upper surface of the tongue. These structures are involved in taste perception.
- 43. MINOR SALIVARY GLANDS Around 450 minor salivary glands in the oral cavity. They contribute 10% of the salivary volume. Sites : Cheek Palate Floor of the mouth Lips Retromolar area Upper aerodigestive tract . oropharynx . Larynx . Trachea . Sinuses
- 44. OROPHARYNX Anterior : oral cavity Above : nasopharynx Below: Hypopharynx Extent: soft palate to upper border of epiglottis.
- 45. Subsites ● Palatine tonsil ● soft palate ● Base of tongue
- 48. HOD MAM: DR.BANUREKHA M.S, DGO Risk factors , Clinical features, Premalignant lesions of oral cavity N.K.Cheran 3rd unit
- 49. HOD MAM: DR.BANUREKHA M.S, DGO Risk factors , Clinical features, Premalignant lesions of oral cavity N.K.Cheran 3rd unit
- 50. Risk factors. ••increase in age •Tobacco •smoking •alcohol •areca nut /pan masala •Epstein Barr Virus •Human papilloma virus •Plummer Vinson syndrome •poor nutrition
- 51. ● AGE: M/c in old age - due to low immunity ● SEX: males affected twice than females ( Due to smoking & tobacco use ) ● SMOKING: cigarettes contain nicotine - carcinogenic ● OCCUPATION: persons who work under uv exposure ⬇️ Lip cancer ● Poor oral hygiene – leads to oral lesions Risk factors of oral lesions
- 52. ALCOHOL: dehydrating effect ⬇️ on oral mucosa ⬇️ increases permeability,DNA damage ⬇️ Allowes carcinogens easily ⬇️ Precancerous to cancerous lesion formation
- 53. ARECA NUT / PAN MASALA: 3 Alkaloids -Arecoline,arecaidine,Guvacaine ⬇️ Increased collagen synthesis,fibroblast formation ⬇️ oral submucosal fibrosis
- 55. TOBACCO - indigenous- smoking or snuff - bidi ,hookah etc Oral chewable form - betel quid ⬇️ Polycyclic aromatic hydrocarbon , nitrosamine,etc ⬇️ Carcinogenic effect ,Chronic irritation ⬇️ Inflammation - cytokines release + activation of TGF growth factor-beta ⬇️. Cancerous lesion formation
- 57. NUTRITION: ● Vitamin c - blocks the conversion of nitrites to nitrosamine which has carcinogenic effect. ● Vitamin A,B Complex , antioxidants,Cu ,Zn- have protective effect on cancer ● Red chillies,spices - causes chronic irritation and results in lesion formation
- 58. HUMAN PAPILLOMA VIRUS: HPV 16,HPV 18,HPV 31,HPV 45 ⬇️ Abnormal alteration & growth lining the infected mucosa in the oral cavity ⬇️ Dysplasia - leads to cancer formation
- 59. EPSTEIN BARR VIRUS : In Immunocompromised individuals it causes oral hairy leukoplakia
- 61. Premalignant lesions of oral cavity High risk ● Erythroplakia ● Speckled erythroplakia ● Chronic hyperplastic candidasis Medium risk ● Oral submucosal fibrosis ● Syphilitic glossitis ● Sideropenic dysphagia Low risk ● Oral lichen planus ● Discoid lupus erythematous ● Discoid keratosis congenita
- 62. Premalignant lesions of oral mucosa & oropharyngeal mucosa present as….. ● Leukoplakia ● Speckled leukoplakia ● Erythroplakia
- 63. Premalignant lesion: ● It is defined as morphologically altered tissue in which cancer is more likely to develop than its apparently normal counter part. ● Premalignant condition: It is a generalised state assosiated with a significantly incresed risk of cancer.
- 64. Premalignant lesions premalignant conditions Leukoplakia Erythroplakia Leukokeratosis nicotina palatinae Candidiasis Carcinoma in situ Oral submucosal fibrosis Oral lichen planus Actinic keratosis Syphilis Discoid lupus erythematosis Sideropenic dysphagia
- 65. Leukoplakia ● A White patch / plaque that cannot be characterized clinically or pathologically. ● Varies from small well circumscribed to an extensive lesion. 3 - types ↙️ ⬇️️ ↘️ Homogeneous nodular speckled Uniform white Fine nodules arises from an Patches. on surface erythematous base
- 67. Predisposing factors .. 7S •syphilis -Sharp tooth •smoking -Sunlight •spirit -UV radiation •sepsis •spices
- 68. 5 stages .. Stage 1 - mild thickening of the surface with hypertropy of the papillae & hyperkeratosis Stage 2 - Tongue is covered with smooth paint. Stage 3 - surface becomes irregular like dried paint Stage 4 - warty projections appears with cracks& fissures( precancerous) Stage 5 - desquamation leads to red glazed tongue ( progress to carcinoma )
- 69. Clinical features … Gross morphology ● Occurs anywhere in oral cavity ( buccal mucosa ,floor of mouth , ventral surface of tongue ,palate ,gingiva). ● Solitary / multiple patches ● ● Thickening,smooth /wrinkled/ fissured. ● Palpation - induration -suggestive of malignant change.
- 70. Investigation… ● Biopsy and histological examination is the key to define the nature and relative risk of leukoplakia. ● Molecular,biological and immunohistochemical techniques(p53 antigen,HPV 16,18,33)are important for detection of leukoplakia with high risk of malignant transformation.
- 71. Differential diagnosis… ● Lichen planus ● Discoid lupus erythematous ● Candidiasis ● Hairy leukoplakia ● Uremic stomatitis
- 72. Histopathology.. ● Hyperkeratosis ● Mild Dysplasia - nuclear hyperchromasia , Increased nuclear to cytoplasmic ratio ● Severe dysplasia - nuclear & cellular pleiomorphism ,numerous mitotic figures
- 73. Treatment: ● Stop pan masala & smoking –homogenous leukoplakia without epithelial dysplasia may disappear or diminish in size with in 2- 3months after cessation of habit. ● Surgical excision ( skin graft if required) ● In wide spread or multiple leukoplakia oral administration of 13- cis retinoic acid (1mg/kg of body weight daily for 2- 3months)maybe used with limited success. ● Topical application of retinoic acid has been used in the treatment of selective cases. ● Co2 laser excision
- 74. Erythroplakia (erythroplasia of queyrat) ● Bright red plaque,which cannot be characterized clinically or patholologically as any other recognisable condition. ● More malignant . ● Can be Homogenous Speckled Erythroleukoplakia
- 75. Clinical features .. Gross morphology ● More common in lower alveolar mucosa ,gingivobuccal sulcus,floor of mouth, tongue & vestibule ● Bright red plaque ● Slightly depressed than surrounding mucosa. ● Surface - nodules ● Red color - decreased keratin ↙️ ↘️ Shining vasodilation + subepithelial Inflammatory reaction
- 76. Investigation: Differential diagnosis 1.Speckled leukoplakia 2.Erythematous candidiasis 3.Early squamous cell carcinoma 4.Local irritation 5.Drug reaction. History and examination. Biopsy-exfoliative cytology Fluorescence staining Toluidine staining
- 77. Histopathology ● Lack of keratin ● Subepithelial Inflammatory reaction ● Vasodilation
- 78. Treatment : 1. Surgical excision 2.Interventional laser surgery is an alternative treatment for oral erythroplakia. 3.Topical 5% imiquimod cream and 5-aminolevulinic acid has been used with for success of treatment.
- 79. Potential risk of malignant transformation… Increases with …… ● Increase with age of the patient ● Increase with age of the lesion ● Higher in smokers ● Increase with alcohol consumption ● Depends on anatomical site of Premalignant lesion ● Higher for leukoplakia in floor of mouth ,ventral surface of tongue, particularly in younger women.
- 80. Chronic hyperplastic candidasis ● Dense plaques of leukoplakia. ● Caused by Candida albicans.
- 81. Immunocompromised individuals ⬇️ Easily acquires fungal infection- Candida albicans ⬇️ Produces oral lesion -chronic hyperplastic candidasis high risk for malignant transformation ⬇️ Dense plaques of leukoplakia ⬇️ M/C -around commissures of mouth ⬇️ Can extend to vermilion & facial skin Chronic hyperplastic candidiasis
- 82. Clinical features: ● White patches over buccal mucosa ,commisures of mouth , Vermilion border ,facial skin . ● Painless ● Lesions are adherent to the surface Investigation Biopsy
- 83. Histopathology Invasion of candidia in epithelium Elongation of epithelial ridges Inflammatory infiltrate
- 84. Treatment: Medical Topical antifungals 6 weeks Systemic antifungals 2 weeks Surgical ● Surgical excision ● Laser vaporization
- 85. Oral submucosal fibrosis: Fibrous bands beneath the oral mucosa ⬇️ Scarring ⬇️ Contracture Progressive disease
- 86. Causes.. ● Prolonged irritation by chillies, tobacco ,areca nut ● Dietary causes - vit A,B complex,iron - deficiency ● Localised collagen disorder ● Common in indian & Asian population - middle age M/c - soft palate ,faucial pillars,buccal mucosa
- 87. Clinical features: ● Trismus - limited mouth opening ● Difficulty in protruding the tongue ● Soreness & burning in mouth during food
- 88. Histopathology Hyperplasia of overlying epithelium Atrophied epithelium replaced with fibroblasts
- 89. Treatment.. Medical ● Avoid precipitating factors- chillies , tobacco, areca. ● Maintain orall hygiene. ● Restricted mouth opening - intralesional steroid (Local injection- dexamethasone 4 mg with Hyalase 1500 units) biweekly for 10 days ● Vitamin and iron deficiency- treat with supplements. Surgical Surgical excision+ skin graft
- 90. Sideropenic dysphagia ● As known as Plummer Vincent / Patterson Kelly syndrome Triad ↙️ ⬇️ ↘️ Iron deficiency. Beefy. Oesophageal web Red tongue
- 91. Iron deficiency ⬇️ Epithelial atrophy of oral mucosa ⬇️ Oral mucosa vulnerable to carcinogens ⬇️ Development of oral cancer
- 92. Treatment.. Iron supplements- correct iron deficiency Reduces atrophy of epithelium & Risk of malignant transformation
- 93. Thank you ! !
- 94. HISTORY AND EXAMINATION OF ORAL CAVITY MALIGNANCY HOD MAM- DR.BANUREKHA M.S.,D.G.O. BY, P.M.Churnika, 3rd unit.
- 95. HISTORY OF PRESENTING ILLNESS: H/O pain, referred to ear H/O Halitosis, foul smelling discharge from mouth H/O dysphagia H/O ulcer H/O excessive salivation H/O alteration in voice, difficulty in speech, difficulty in swallowing H/O difficulty in opening mouth H/O swelling in upper part of neck H/O fever H/O loss of weight, loss of appetite H/O trauma H/O recent falling of tooth H/O hemoptysis, pleuritic chest pain
- 96. HISTORY: AGE AND SEX- cleft lip, cleft palate-birth mucous retention cyst, stomatitis-any age carcinoma lip and tongue-Males above 50 yrs. OCCUPATION: Outdoor activities-countryman’s lip RESIDENCE: White causians in Australia-more susceptible negroes –less susceptible INCIDENCE- MC in India- CARCINOMA GINGIVOBUCCAL SULCUS MC in west – CARCINOMA TONGUE.
- 97. SWELLING/ULCER: mucous retention cyst –inner side of lip or cheek, very slow growth, long time cancer of lip, tongue-short history though slow growing
- 98. PAIN: Site of pain: dental ulcer --side of tongue late Carcinoma tongue –referred to ear of affected side(lingual, auriculotemporal nerve) PAINFUL PAINLESS Aphthous ulcer Carcinoma Dental ulcer Syphilitic ulcer Tb ulcer Systemic diseases Smoker’s ulcer Monilial ulcer Herpetic ulcer Leucoplakia Ictal ulcer Mucous retention cyst
- 99. SPECIFIC COMPLAINTS: o excessive salivation-carcinoma tongue o inability to protrude tongue –tongue tie, late stage of carcinoma tongue o difficulty in speech-cleft lip, cleft palate, carcinoma tongue o deviation of tongue tip to side of lesion –carcinoma tongue. o alteration of voice-1st symp of carcinoma posterior 1/3 tongue
- 100. PAST HISTORY: H/O DM,TB,AIDS,any immunocompromised state H/O ill fitting dentures H/O tooth removal with delayed healing of socket H/O sexually transmitted diseases
- 101. PERSONAL HISTORY: smoking, alcohol leucoplakia Tobacco ,spicy food Clay pipe smoking- carcinoma Tongue Exposure to sunlight- carcinoma lip betel nut ,Pan chewing- carcinoma cheek Supari/khaini Eg: betel quid kept in inner aspect of left cheek for 30 mins each time and spits it out. Uses it 6times/day. Reverse smoking- carcinoma hard palate Diet – vit A, (Iron Deficiency Anemia-squamous cell carcinoma of oral cavity, hypopharynx)
- 102. GENERAL EXAMINATION: Cancer-anemia, cachexia, tb ulcer-primary focus in lungs gummatous-syphilitic lesions EXAMINATION OF ORAL CAVITY: LIPS HARD AND SOFT PALATE BUCCAL MUCOSA(CHEEK) RETROMOLAR TRIGONE TONGUE FLOOR OF MOUTH GUMS/ALVEOLUS
- 103. PHYSICAL EXAMINATION INSPECTION: 1.Lips, 2.cheek-retract outwards 3.Gums, 4.floor of mouth, 5.Posterior 1/3rd OF TONGUE -push tongue to one side 6.Anterior 2/3rd Tongue-mouth opened fully, protrusion of tongue 7.Fauces,tonsil,beginning of pharynx-depress tongue with spatula 8.Dental formula :2123 2123 2123 2123
- 104. INSPECTION 1.LIPS: Cleft lip Cleft palate Facial cleft Pigmentation of lip and buccal mucosa-Addison’s disease Small bluish black spots-Peutz jegher’s syndrome Chancre of lip-painless ulcer, dull red Cracked lips-midline of lower lip(cold weather) Ectopic salivary neoplasm-upper lip, slow growing,lobulated
- 105. CA lip-erosion in early stage red granular appearance with whitish flecks, Yellowish crusting in middle of erosion ulcerated centre, everted margin skin –red, vascular Macrocheilia-thickening (upper lip)
- 106. 2.TONGUE: Volume Macroglossia--lymphangioma,hemangioma, neurofibroma,muscular macroglossia(cretins) Colour white – leucoplakia(chronic superficial glossitis) Red glazed tongue-desquamated leucoplakia, Blue-venous hemangioma Black,hairy-antibiotics,hyperkeratosis in smokers (aspergillus Niger) Crack/fissure Syphilitic-longitudinal
- 107. INCIDENCE SITE of carcinoma in tongue 25% ANTERIOR 1/3RD LATERAL *2 (ON EACH=50%) 10% TIP 10% UNDER SURFACE 5% DORSUM 25% POSTERIOR 1/3RD
- 108. Swelling/ulcer: Dental ulcer-lateral margin of tongue Traumatic ulcer Aphthous ulcer-small, multiple Tb ulcer -tips and sides Gummatous ulcer-midline ant2/3rd dorsum of tongue, Carcinomatous ulcer-scc MC SITE:MIDDLE 3RD OF LATERAL MARGIN OF TONGUE Angioma like swelling –lingual thyroid (at foramen caecum) Mobility of tongue: Inability to protrude completely-ankyloglossia Deviate(impaired nerve supply)- advanced CA tongue Impaired speech ,not protrude-tongue tie
- 109. 3.PALATE: Congenital cleft Perforation of hard palate-syphilis ulcer- Most Common-MINOR SALIVARY GLAND TUMORS
- 110. 4.GUMS: Healthy gums-bright pink Pyorrhoea alveolaris-deep red line along free edge of gum Vincent stomatitis-ulcer,pseudomembrane,bad smell. Cancrum oris-painful, purple red papule on molar/premolar area Dental abscess-swollen gums Lead-blue line
- 111. 5.FLOOROF MOUTH: ranula-unilateral, bluish translucent cyst Sublingual dermoid-opaque, midline, submental region Plunging ranula-cervical prolongation to submandibular region Wharton’s duct opening Leucoplakia of floor of mouth and ventral surface of tongue: high incidence of malignant change .
- 112. 6.CHEEK: Pigmented patches-Addison’s disease, Peutz jegher’s syndrome Mucous cyst-buccal mucosa of cheek at bite of teeth Stenson’s duct opening Cyst Salivary tumour Ulcer
- 114. PALPATION: 1.LIP: Benign-firm, lobulated carcinoma lip-stony hard, always fixed Hunterian chancre-rubbery hard Mucous retention cysts-inner surface of lower lip Fluctuation, transillumination –positive in large cysts Squamous cell carcinoma most common in lower lip
- 115. 2.TONGUE: ULCER TB SYPHILITIC APHTHOUS ULCER TRAUMATI C MALIGNANT Pain PAINFUL Painless Painful Marked Painless--- painful,iceberg like Shape Oval/circular Round Any shape Irregular Number Multiple Single Single/multi Single Single Edge Undermine d Punched out - Edematous Everted, rolled out Floor Pale granulation tissue Wash leather slough White floor,yellowish border, Slough Necrotic debris,dirty grey Discharg e Thin ,watery Greyish white - Purulent BLEED ON TOUCH, Thick,purulent,offensiv e Induratio n - Slight - slight Marked
- 116. 3.PALATE: Alveolar abscess-tender, fluctuating swelling Gumma-soft, swelling in middle of hard palate Mixed tumour of ectopic salivary gland. 4.GUMS: Scurvy-bleed, swollen, tender Uremia-bleed Epulis-swelling of alveolar margin of gum
- 117. 5.FLOOROF THE MOUTH: Ranula-fluctuating ,brilliantly transilluminant. Sublingual dermoid-not translucent,tense fluctuant in midline. Carcinoma of floor of mouth-fixed, indurated base
- 119. 6.CHEEK: Mucous cyst-smooth surface, mobile ,fluctuate Papilloma-solid tumor,irregular surface,mobile Carcinoma-fixed, indurated Most common carcinoma IN CHEEK- SQUAMOUS CELL CARCINOMA
- 120. Examination of soft palate
- 121. EXAMINATION OF JAW: Upper jaw(maxilla) Swelling/ulcer-epulis Tenderness in maxillary antrum without distension-empyema TEETH-count, dental cyst, dentigerous cyst
- 122. Lower jaw(mandible):(carcinoma tongue, floor of mouth, lip) thickening /irregularity, alveolar abscess Fracture of mandible(mostly at the region of canine tooth) Body, angle, inferior part of ramus of mandible-accessible For temporomandibular joint: Ask patient to open and close his mouth-trismus, ankylosis Place fingers over temporomandibular joint just below and in front of tragus – crepitus(osteoarthritis)/clicking jaw(loose meniscus/disarticulated articular cartilage) Little finger inserted into external ear with pulp directed forwards-dislocation
- 123. EXAMINATION OF CERVICAL LYMPH NODES LEVEL PRIMARY CANCER SITES 1 Anterior tongue,floor of mouth,anterior alveolar ridge,lip,salivary gland 2 Oral cavity,oropharynx,nasopharynx,salivary gland,larynx 3 Oral cavity, lateral tongue, oropharynx,hypopharynx,thyroid, larynx 4 Oral cavity,hypopharynx,larynx, thyroid, cervical esophagus 5 Git,lungs,testis,scalp,external ear, 6 Thyroid 7 CARCINOMA TONGUE- SKIP METASTASIS
- 125. OTHER SYSTEM EXAMINATION: Head and neck Cranial nerves-7,8,9,10,11,12 Ear,nose,throat. Thyroid Central nervous system Cardiovascular system Respiratory system Abdomen
- 126. COMMON MODES OF PRESENTATION: Anterior 2/3rd of tongue-ulcer Posterior 1/3rd of tongue-pain, dysphagia, dysarthria Dentate patient-swelling of gums, tooth extraction which fails to heal Numbness over distribution of mental nerve Pathological fracture of mandible
- 127. THANK YOU
- 128. CLASSIFICATION,STAGING AND INVESTIGATIONS OF ORAL CAVITY MALIGNANCIES - E.DEEPAK KUMAR - UNIT 3 HOD MAM: DR.BANUREKHA M.S.,D.G.O.
- 129. SPREAD OF SQUAMOUS CELL CARCINOMA • Local infiltration ◦ Invasion of local soft tissues ◦ Invasion of perineural space ◦ Invasion of vessels ◦ Invasion of bone • Lymphatic spread • Hematogeneous spread (distant metastasis)
- 130. NECK NODE LEVELS • IA- Submental nodes • IB- Submandibular nodes • II - Upper jugular nodes • III- Middle jugular nodes • IV- Lower jugular nodes • VA &VB- Posterior triangle nodes • VI- Anterior compartment nodes • VII- Upper mediastinal nodes
- 131. CARCINOMA OF LIP Most common location of oral cancer. 90% on lower lip,common in old age. 90% 5-year survival if <2 cm 90% squamous cell carcinoma (Rules of 90's) Basal cell carcinoma is more common on upper lip 2-15% regional metastasis (for all stages)
- 132. CLINICAL FEATURES • Non-healing progressive ulcer, painless to begin with • Everted edge with indurations • Growth moves with the lip • Fungation, bleeding, halitosis is present Red granular appearance with whitish flecks. Yellowish crusting in the middle of erosion The centre becomes ulcerated and margin becomes everted
- 133. SPREAD OF CARCINOMA LIP • Lower lip has bilateral and ipsilateral lymphatic drainage into level I-Ill nodal groups • Upper lip has ipsilateral lymphatic drainage into level I-Ill nodal groups (no contralateral drainage due to embryological fusion plates).
- 134. CARCINOMA TONGUE GROSS 1. Papillary. 2. Ulcerative or ulceroproliferative 60%. 3. Fissure with induration. 4. Lobulated, indurated mass—frozen tongue.
- 135. CLINICAL FEATURES Painless ulcers/ swelling in tongue. Excessive salivation ( often blood stained) Dysphagia Inability to articulate Ankyloglossia Halitosis Bronchopneumonia SITES OF CARCINOMA 1.Lateral margin (47-50%) 2.Posterior third (20%) 3.Dorsum (6.5%) 4.Ventral surface (9%) 5.Tip (10%)
- 136. SPREAD OF CARCINOMA TONGUE LOCAL SPREAD: • In case of anterior two-thirds of tongue, the spread occurs to genioglossus muscle, floor of the mouth, opposite side and mandible. • In case of posterior third of tongue it spreads locally to tonsil, side of pharynx, soft palate, epiglottis, larynx and cervical spine.
- 137. Lymphatic spread: • From tip of tongue it spreads to submental nodes. • From lateral margin it spreads to submandibular lymph nodes and later to deep cervical lymph nodes. • From posterior third it spreads to pharyngeal nodes and upper deep cervical lymph nodes. • All oral cavity malignancies spread to level I and II sometimes level III • Tongue malignancy follows skip metastasis and spread to level III and IV
- 138. CARCINOMA CHEEK/BUCCAL MUCOSA Clinically, there are three distinct types: exophytic, ulcerative, and verrucous. The patient may present with pain or bleeding, trismus,halitosis. Posterior extension may result in involvement of the lingual or dental nerves, which may cause ear pain. Extension behind the pterygomandibular raphe into the pterygoid muscles or into the buccinator and masseter muscles may cause trismus. Involvement of retromolar trigone indicates an advanced disease. Death usually occurs as a result of poor nutrition and general debilitation
- 139. SPREAD OF CARCINOMA BUCCAL MUCOSA LYMPHATIC SPREAD The submandibular lymph nodes are most frequently involved; involvement of the upper cervical and the parotid lymph nodes is less common. LOCAL SPREAD Infiltrating lesions of the buccal mucosa can invade the buccinator muscle, extend to the buccal fat pad, and invade the subcutaneous tissue. Carcinomas of the buccal mucosa frequently spread by direct invasion into the gingivobuccal sulcus, the upper and lower alveolar ridges, the hard palate, the maxilla, and the mandible.
- 140. OTHER CARCINOMAS CARCINOMA OF HARD PALATE: • Minor salivary gland tumours(adenoid cystic) are more common in palate. • Malignant tumours may spread to periosteum, bone, maxilla,sinus, or nose. • Upper deep cervical nodes are involved in 25% of patients. CARCINOMA OF ALVEOLUS • It is squamous cell carcinoma arising from gums • There will be invariable bone involvement by direct extension • Nodal spread is also common
- 141. As posterior third tongue has got abundant lymphatics which cross communicates on either side, lymph node spread is common (70%). Bilateral nodal spread is common. Remains asymptomatic for long time —> Early symptoms mimic sore throat —> Late symptoms dysphagia and change in voice. Infiltration into the tongue muscles like genioglossus, epiglottis, pre- epiglottic space, tonsillar pillars and hypopharynx are common. Hematological spread is common,carry poor prognosis. CARCINOMA FLOOR OF MOUTH
- 142. SECONDARIES WITH UNKNOWN PRIMARY Primary may be very small to be detected clinically in places like fossa of Rosenmuller, pyriform fossa, nasopharynx, posterior third tongue but present clinically as hard lymph node secondaries in neck called as secondaries with unknown primary. Hard secondaries in neck confirmed by FNAC but all investigations including blind biopsies, CT head and neck region and endoscopies could not identify primary lesion creates a situation called as secondaries in neck nodes with an occult primary (30%).
- 143. QUIZ A 58-year-old man presents with discomfort in his mouth. He denies any trauma to his oral mucosa. He has smoked cigarettes daily for the past 38 years. He drinks 2 beer daily. His heart rate is 94 beats/minute, blood pressure is 142/74 mmHg, and temperature is 37°C (98.6°F). On physical examination, the physician notices a plaque in the oral mucosa. Which of the following findings would most likely indicate the plaque is a premalignant lesion? a) A white deposit on the tongue that can be easily scraped off b) A white, rough patch on the lateral tongue c) A white plaque that cannot be scraped off d) A clear base surrounded by erythema
- 144. INVESTIGATIONS
- 145. CLINICAL FEATURES OF ORAL CANCER THAT WARRENT INVESTIGATION Persistent oral swelling for >3 weeks Mouth ulceration for >3 weeks Sore tongue Difficulty swallowing Jaw or facial swelling Painless neck lump Unexplained tooth mobility Trismus
- 146. BIOPSY When a clinical diagnosis of oral cancer is suspected,a tissue diagnosis, typically by way of incisional biopsy(edge biopsy), is essential. The biopsy must include the most suspicious area of the lesion, as well as normal adjacent tissue.
- 147. Biopsy has to be taken from the edge as it contains active cells; not from the centre as it is the area of necrosis. Malignant squamous cells with epithelial pearls (Keratin pearls) are the histological features.
- 148. MAGNETIC RESONANCE IMAGING- Staging It provides excellent visualisation of soft tissue infiltration of the tumour. Ideally it should be performed before diagnostic biopsy as biopsy frequently distorts the image of the primary tumour. It can detect the cervical node metastasis
- 149. COMPUTED TOMOGRAPHY- Staging CECT Head and neck is useful when bony invasion is suspected. CT of the thorax and abdomen is now indicated for all patients and not just those with proven cervical lymph node metastasis and large-volume disease. CT is much more widely available than MRI but its utility may be restricted by artifact degredation of images by dental restorative materials.
- 150. ULTRASOUND It is useful in evaluation of undiagnosed neck lumps or presumed cervical metastasis. Used alongside fine-needle aspiration cytology (FNAC), ultrasound is capable of delineating and sampling cervical lymphadenopathy and both thyroid and salivary gland lesions/masses.
- 151. abnormal nodes include shape (round), absent hilus, intranodal necrosis, reticulation, calcification, matting, soft-tissue edema,low or mixed echogenecity and peripheral vascularity. sonograms of patients with metastatic nodes. Image of 70-year- old man with carcinoma of tongue and with bilateral metastatic upper cervical lymph nodes shows one of metastatic upper cervical nodes is hypoechoic, round, and without echogenic hilus (arrows). Lymph node also shows multiple areas of intranodal cystic necrosis (arrowheads).
- 152. FINE NEEDLE ASPIRATION CYTOLOGY FNAC is useful for the assessment and pathological diagnosis of enlarged cervical lymph nodes. It involves the use of a fine-needle puncture into the mass and immediate aspiration for cytological examination. It has few complications and there is no evidence of tumour seeding along needle tracts. It requires no specialist equipment other than a 21G or 23G needle and a 10 mL syringe.
- 153. POSITRON EMISSION TOMOGRAPHY COMBINED WITH CT • Positron esmission tomography combined with CT (PET-CT) of the whole body uses the anatomical capability of CT scanning in concert with radiolabelled tracers capable of localising to specific tissues. • The most widely used tracer is 18 fluoro-dexoyglrucose (FDG), which is transported and trapped within hypermetabolic tissues (typically cancerous or inflammed tissues, or those that are predictably physiologically active).
- 154. ORTHOPANTOMOGRAM To access the state of dentition and potential gross mandibular invasion.
- 155. OTHER INVESTIGATIONS Direct and Indirect laryngoscopy Endoscopy Dentist opinion Complete blood count Blood grouping Liver function tests Hiv/HbsAg Chest x-ray ROUTINE BLOOD INVESTIGATIONS
- 156. TNM STAGING OF ORAL CAVITY CANCER By American Joint Committe on Cancer (8th edition,2018)
- 157. T- STAGING Tx- Primary tumour cannot be assessed Tis- Carcinoma in situ T1- Tumour ≤2cm with depth of invasion ≤5mm • T2- Tumour ≤2cm with depth of invasion >5mm and ≤10mm OR Tumour >2cm and <4cm with depth of invasion ≤10mm
- 158. T3- Tumour 2cm-4cm with depth of invasion >10mm OR Tumour >4cm with depth of invasion ≤10mm • T4- Tumour moderately advanced local disease or very advanced local disease
- 159. T-STAGING OF LIP CARCINOMA
- 160. T-STAGING OF CARCINOMA OF TONGUE
- 161. T4a (lip) - Invading through cortical bone, inferior alveolar nerve, floor of mouth or skin of face(chin or nose). T4a (Oral cavity) - Invading adjacent structures eg, cortical bone, deep extrinsic muscle of tongue, maxillary sinus or skin of face. T4b - Invading masticator space, pterygoid plates, skull base or encases Internal carotid artery (Superficial erosion alone of bone/ tooth socket by gingival primary is not T4)
- 162. N- Nodal spread Nx - Nodes cannot be assessed. NO - No regional lymph node spread. N1 - Regional single node <3 cm with no Extranodal extension N2 - N2a: Single ipsilateral node <3 cm with Extranodal extension OR single ipsilateral node 3-6 cm with no Extranodal extension
- 164. • N2b: Multiple ipsilateral nodes <6 cm in size and no Extranodal extension • N2c: Bilateral or contralateral nodes <6 cm with no Extranodal extension N3 - N3a: Single ipsilateral node >6 cm with no Extranodal extension N3b: single ipsilateral node >3 cm with Extranodal extension OR multiple ipsilateral or contralateral or bilateral any sized nodes with Extranodal extension OR single contralateral node of any size with Extranodal extension
- 165. M- DISTANT METASTASIS cM0- Distant metastasis not present cM1- Distant metastasis present pM1- Distant metastasis,microscopically confirmed
- 166. STAGING GROUPS
- 168. STAGING GROUPS Stage 0 - TIS NO MO Stage I - T1 NO MO Stage II - T2 NO MO Stage III - T3 NO MO; T1, T2, T3 N1 MO Stage IV - IVA: T4a NO/N1 MO; T1, T2,T3, T4a N2 MO. IVB: Any T N3 MO; T4b any N MO. IVC: Any T Any N M1
- 170. Surgery for Oral Cavity Malignany HOD MAM : Dr.BANUREKHA.MS.,DGO -By R.Deepak Raja IIIrd UNIT
- 171. Management Treatment of oral cancer is based on staging of cancer *STAGE 1&2:- -Early stage oral Cancer [Single Modality Treatment]-(Surgery or RT) *STAGE 3&4a:- -Locally advanced & Operable cancers [Combined Modality Treatment] *STAGE4b&4c:- -palliative [RT or CT] or Symptomatic Treatment
- 172. Criteria for Inoperability Fixed Neck Nodal Adenopathy Recent onset of trismus (Gross Infratemporal Fossa Invasion) Base skull involvement Extensive Soft Tissue Invovement Distant Metastasis
- 173. Neck Dissection Incision-Modified Schoebinger Incision Modified Radical Neck Dissection[MRND] Level I-V lymph nodes are Removed + At least One of the 3 Extra Lymphatic structures are saved (*Spinal Accessory Nerve *Sternocleidomastoid *Internal Jugular Vein)
- 174. MRND Classification MRND 1-Spinal accessory Nerve is saved MRND 2-Spinal accessory Nerve and Internal jugular Vein is saved MRND 3-All 3 are saved (Functional neck Dissection)
- 175. Other Methods Radical Neck Dissection(Crile’s Operation) Level I-V Lymph Nodes are Removed+ All 3 extra Lymphatic Structures are Removed Selective Neck Dissection: 1.Central neck dissection(CND)-Level VI lymph nodes are removed 2.SupraOmohyoid Neck Dissection(SOHND)-levels I,II,III are removed 3.Extended SOHND-Levels I-IV are removed
- 176. Principles Of Management of NECK
- 177. Primary Reconstructive Options In Oral Cancers Anatomical Site Primary Reconstructive Options Alternative Reconstruction Floor of mouth Buccal Mucosa Tongue Base Lateral Tongue Radial forearm free flap For Tongue : PMMC Flap Total Tongue AnteroLateralThigh OR Rectus Abdominis flap PMMC flap Maxillary Tumors Iliac crest graft** is the method of choice for Maxillary Reconstruction Fibula
- 178. Survival and Prognosis Stage I & II Disease have Better Prognosis (5 Years survival 31-100%) • Stage III & IV Disease-Advanced have Poor Prognosis (5 Years survival 7-41%)
- 179. Content I. LIP CANCER II. TONGUE CANCER III. BUCCAL MUCOSA CANCER IV.FLOOR OF MOUTH V. RETROMOLAR PAD VI.HARD PALATE
- 180. I. Lip Cancer It usually arises as an ulcer on the vermilion border. ⮚ 95% - On the lower lip, ⮚15% -On central one-third and commissures. ⮚Squamous cell carcinoma- M/C in lower lip, ⮚Basal cell carcinoma- M/ C in upper lip
- 181. •Initially starts as *Occasionally it occurs at the angle of mouth a red granular dry lesion ulcerated ulcero-proliferative lesion.
- 182. A.Small Tumors ⮚Small tumours (<2 cm) of the lip -either a V- or W-shaped excision under local or general anaesthesia. ⮚The defect, (which should be no larger than one-third of the total lip size), is closed in three layers – mucosa, muscle and skin – with particular attention paid to the correct alignment of the vermilion border Skin markings for wedge excision of the lower lip. Primary closure.
- 183. B.Intermediate tumours ⮚Larger tumours, (defects of between one-third and two-thirds the size of the lower lip)-require local flaps for reconstruction. ⮚V or W excision —>microstomia. ⮚Large central defects can be managed using local flaps —the Johansen step technique. ⮚This allows closure of the defect by symmetrical advancement of soft-tissue flaps, utilising the excess skin in the labiomental grooves. ⮚Alternative techniques include the Bernard or the Karapandzic advancement flaps. Skin markings for Johansen step reconstruction. Closure of lip and labiomental steps.
- 184. C.Total lip reconstruction ▪Extensive tumours of the lower lip, which invade adjacent tissues (T4), have a high incidence of neck node metastasis. ▪Patients with such advanced disease require surgery, which may include - unilateral or bilateral selective neck dissection, - total excision of the lower lip and chin, - with or without adjacent mandibular resection (rim or segmental mandibulectomy ). Skin markings for total excision of the lower lip,chin and left selective neck dissection
- 185. ▪The lower lip soft-tissue defect can be reconstructed with a variety of free flaps including the - radial forearm flap potentially suspended with palmaris longus tendon (or) - perforator flaps such as the anterolateral thigh(ALT) flap (or) - The medial sural artery perforator (MSAP) free flap. *the scapula free flap provides exceptional flexibility and tissue variability. Postoperative view of the reconstructed lower lip using a radial artery forearm flap.
- 186. Methods of Reconstruction 1. Abbe-Estlander's rotation flap used for either upper or lower lip lesions (of less than ½ of lip) located at the angle based on labial artery.
- 187. 2. Fries' modified Bernard facial flap -reconstruction using lateral facial flaps. - It is used when defect is more than ½ of lip and midline.
- 188. II. Tongue Cancer ▪ The tumors may present as ulcerations or as exophytic masses. ▪ The regional lymphatics of the oral cavity are to the submandibular space and the upper cervical lymph nodes. ▪ The lingual nerve and the hypoglossal nerve may be directly invaded by locally extensive tumor ▪ Involvement can result in - ipsilateral paresthesias, -deviation of the tongue on protrusion with fasciculations & eventual atrophy. Ulcerative squamous cell carcinoma of the right lateral border of the tongue.
- 189. •Tumors on the tongue may occur on any surface, but are most commonly seen on the lateral and ventral surfaces. •Primary tumors of the mesenchymal components of the tongue include -leiomyomas, -leiomyosarcomas, -rhabdomyosarcomas & -neurofibromas.
- 190. Access Access for oral cancer -allow accurate assessment -clear visualisation to enable tumour clearance to be achieved. Access techniques include: ❖Transoral – small –moderate sized anterior oral tumours; ❖Lip-split technique and paramedian or median mandibulotomy. ❖Visor incision with or without drop down. Skin markings for lip split and mandibulotomy in continuity with neck dissection Visor approach to the anterior mandible/floor of the mouth and tongue.
- 191. Surgery • Tumour less than 1 cm in size or in carcinoma insitu -Wide excision with 1 cm clearance in margin and depth is done in Laser (CO2/diode) can be used. • Tumour between 1-2 cm in size -partial glossectomy is done with 2 cm clearance from the margin with removal of 1/3rd of anterior two-thirds of the tongue. • Tumour larger than 2 cm, -Hemiglossectomy is done with removal of anterior 2/3rd of tongue on one side up to sulcus terminalis
- 192. •Wide excision - growth is in the tip of the tongue. Same side palpable, mobile lymph nodes - radical neck block dissection. Bilateral mobile lymph nodes - One side radical block & Other side modified radical block dissection with essentially retaining internal jugular vein (on opposite side) to maintain the cerebral venous blood flow. ( Other option is doing same side radical neck dissection and on opposite side Supra Omohyoid block dissection.) • Posterior third growth - lip split and mandible resection, so as to have total glossectomy- Kocher's approach ( When mandible is involved hemimandibulectomy is done.)
- 193. Reconstruction ▪ Small defects of the lateral tongue -primary closure or be allowed to heal by secondary intention with little or no functional impariment. ▪ Larger defects (e.g.T2, T3 and T4 resections) require formal reconstruction to encourage good speech and swallowing. [Free tissue transfer of suitable tissue (e.g. a radial forearm flap, or ALT), utilising microvascular anastomosis in most instances,gives a good functional result] ▪ Large-volume defects, including total glossectomy, may require more bulky flaps such as the rectus abdominus free flap or ALT depending on patient body habitus.. Radial artery forearm flap raised before division of a vascular pedicle and cephalic vein
- 194. Carcinoma Of Posterior One-Third Of Tongue •Carcinoma posterior third of the tongue is often poorly differentiated and so caries poor prognosis. •T1, T2, N0 and N1 diseases surgical wide excision or often by total glossectomy +midline mandibulotomy incision (mandible split) +neck dissection on both sides (MRND one side).
- 195. III.Carcinoma Of Buccal Mucosa • Squamous cell carcinoma is the most common type of carcinoma of the cheek. • Occasionally it can be adenocarcinoma arising from the minor salivary glands or mucous glands. Rarely it can also be melanoma. • Carcinoma is common in posterior half of cheek than anterior. • It spreads outwards to involve the skin causing fungation, ulceration, orocutaneous fistula formation. Exophytic squamous cell carcinoma of the right buccal mucosa.
- 196. Indication for Surgery Early tumour Tumour spreading to mandible bone/alveolus Fungation, haemorrhage due to erosion Recurrence of tumour after RT Multiple sites Soft tissue spread Locally advanced but amenable to surgical resection
- 197. Surgery 1.Wide excision -wide excision with 1-2 cm clearance. -Often, the approach to the tumour is by raising the cheek flap (outside). -After the wide excision, the flap is placed back-Patterson operation 2. Hemimandibulectomy 3.Neck lymph nodes block dissection.
- 198. •SCC of the buccal mucosa should be excised widely, including the underlying buccinator muscle. •Access for buccal carcinoma can be achieved either -Transorally for smaller lesions (T1, T2) or -Lip-splitting technique for larger lesions (T3, T4). •Reconstruction of the buccal mucosa prevents scarring and trismus. •Options include the radial artery forearm flap or a temporalis muscle flap. -Raw temporalis muscle inset into the buccal mucosal defect will epithelialize spontaneously over several weeks.
- 199. •Growth with mandible involvement: wide excision of the primary tumour+ hemimandibulectomy or segmental resection of the mandible or marginal mandibulectomy (using rotary electric saw) is done. •Operable growth with mandible involvement and mobile lymph nodes on the same side (confirmed by FNAC): wide excision of the primary tumor +Hemimandibulectomy +radical neck lymph node dissection is done (like commando operation). -It is called as composite resection.
- 201. IV.Floor of Mouth • Surgical excision may include a Partial Anterior Glossectomy and Anterior mandibular resection. • Only very small tumours of the floor of the mouth can be managed by simple excision. • Management of the adjacent mandible/mandibular rim may be necessary where the tumour abuts the mandible. • this may be by way of a rim resection or segmental mandibulectomy.
- 202. Reconstruction After Surgery •Reconstruction will depend on the defect size (and its constituents) and ranges from healing by secondary intention to use of the - thin, pilable radial forearm free flap for small defects, - to ALT and composite flaps for larger resections. •If a patient is unfit for microvascular free-flap surgery or the facilities are limited, -bilateral nasolabial flaps tunnelled into the mouth and interdigitated provide an acceptable alternative
- 203. V. Retromolar Pad •Tumours occurs at this site frequently, but not always, invade the ascending ramus of the mandible. •They also spread medially into the soft palate and the tonsillar fossa. •Access for excision may necessitate additional access (e.g. a lip split and mandibulotomy).
- 204. •Small defects are managed ideally with a microvascular free flap, such as -a radial artery forearm flap -with a temporalis muscle flap ( where pedicled options are preferred) •Abundant soft tissue capable of modification and flexible at inset, to suit larger defects.
- 205. VI.Carcinoma of hard palate •Squamous cell carcinoma is ulcerative with raised and everted edge. •Upper deep cervical lymph nodes are involved in 25% of patients. •wide excision with removal of the underlying palatal bone. •Often Partial or Total maxillectomy ( Weber-Ferguson incision) may be required.
- 206. •Myocutaneous flap with dental prosthesis is essential to reconstruct after surgery. •Postoperative radiotherapy and neck block dissection are often required.
- 208. NON- SURGICAL MANAGEMENT OF ORAL CAVITY MALIGNANCY -B.Dhanalakshme 3rd unit
- 210. RADIOTHERAPY CHEMOTHERAPY LASER SURGERY CRYOTHERAPY COBLATION RECENT ADVANCES IN TREATMENT OF MALIGNANCY
- 211. RADIOTHERAPY Cellular death Free radical reaction Apoptosis Cell cycle arrest • Curative • Palliative MODALITIES OF APPLICATION:
- 212. INDICATIONS: early growth no bone involvement patients who refuse surgery inoperable/ advanced cases METHODS OF APPLICATION: external beam radiotherapy brachytherapy
- 213. TYPES OF RADIOTHERAPY Conventional Three dimensional conformal radiation therapy Intensity modulated radiation therapy Image guided radiation therapy Streotactic body radiation therapy Adaptive
- 214. TREATMENT MACHINES Cobalt 60 – emits gamma rays Linear accelerator Proton beam radiotherapy-deep seated tumours [bragg peak effect] Gamma knife Cyberknife Tomotherapy
- 215. Low / linear energy transfer- X-rays, gamma rays High energy transfer- electron, protons, neutrons PRINCIPLES: Penetrated into deep seated tumour Building of radiation under skin of the tumour to reduce skin reactions Precise targeting towards tumour Efficacy of the radiation therapy depends on the patient ‘s health condition, tumour grading, lymphatic invasion
- 217. PREOPERATIVE RADIOTHERAPY ADVANTAGES: Downstage the tumour and reduce the tumour bulk Vascularity is not affected Blockage of lymphatics Decreases microscopic spread Allows time for supportive therapy for subsquent surgery{cariac , nutrition, pulmonaryn DISADVANTAGES: Impaired healing process Delays definitive surgery Flap necrosis Fistula formation , Carotid blow out
- 218. POSTOPERATIVE RADIOTHERAPY Resected tumour margin is positive Extracapsular nodal spread Multiple lymph nodes DISADVANTAGES: Pathologically cure cannot be assessed Flap necrosis, dehiscence
- 219. CARCINOMA OF CHEEK SCC- radiosensitive Early tumour Fixed primary tumour/ advanced secondary Nart
- 220. ADVANTAGES No anasthesia complications No surgical mutilation Surgery is avoided Cosmetically acceptable preservation of organ and its function 80to90 % cure
- 221. DISADVANTAGES Infection Hypothyroidism Soft tissue fibrosis Dryness , xerostomia Skin excoriation , hair loss Osteoradionecrosis
- 223. CARCINOMA OF TONGUE ADVANTAGES: Pre- operative , post operative Posterior one third of tongue DISADVANTAGES: Loss of taste sensation Trismus, ankyloglossia Dermatitis, sepsis Pharyngeal oedema
- 224. CARCINOMA OF LIP Size [<2cm],- curative Postoperative – large tumour/ fixed lymph nodes CARCINOMA OF HARD PALATE: postoperative radiotherapy SECONDARY METASTASIS WITH UNKNOWN PRIMARY Definitive radiotherapy is given Surgery and post operative radiotherapy [advanced disease] Biopsy of the node and radiation of all suspected areas
- 225. RADIOSENSITIZERS Hyperbaric oxygen , nicotinamide, carbogen Nimorazole and tirapamazine Chemotherapeutic agents[concomitant radiotherapy] • Antioxidants • Lipoic acid • cysteine RADIOPROTECTORS
- 226. DOSAGE: Definitive- Daily dosage of 180-200cGy/ day- 5 days /week 6 to7 weeks Postoperative therapy – 6000cGy{ for 6 weeks} daily- 5 days / week T3,T4 TUMOURS N2,N3 NODES MULTIPLE NODES PALLIATIVE:
- 227. FRACTIONATION Hyperfractionation: smaller doses{110-120cGY}, given in multiple doses Better locoregional control , delayed side effects Accelerated fractionation:180-200cGY , dose is steadily increased, Duration of treatment is shortened , side effects are more Hypofractionation:600-800cGY, fraction delivered several days apart duration of treatment is shortened, low total radiation
- 228. CARE OF THE PATIENT DURING RADIOTHERAPY Skin: avoid exposure to sun, chemical irritants , lotion/ ointments{ don’t rub/ scratch skin Oral cavity and dentition: gargle several times [salt , bicarbonate] mild antiseptic lotion, fluoride gel Preirradiation extraction of loose teeth Infection: antibiotic Thyroid profile
- 229. Nutrition : High protein diet with vitamins and minerals Blended/ semisolid diet Ryle tube/ percutaneous gastrotomy Psychological support Severe Complications –hospitalization CT scan and MRI SCAN – for evaluation and follow up 18-FDG-PET Scan
- 230. BRACHYTHERAPY •Sealed radiaton inside or close to the tumour, delivered via catheters, implants •Gold[198],pallidium[103],caesium[13], iridium[197] •Radiation material placed in the cavity- intracavity radiotherapy •Radiation material inserted into the tissue- interstitial radiotherapy •Combined with external beam radiotherapy
- 231. •Implants can be kept either temporarily or permanently •Low dose brachytherapy - 40-200cGY /hr •High dose brachytherapy - 1200cGY/hr
- 232. Advantages: Localised , deeper, less side effects, adjacent tissues are spared avoiding surgeries High dose rate with short duration Curative and effective Disadvantages: Non availability of the facility Technically difficult local : displacement , erosion
- 233. CHEMOTHERAPY Neoadjuvant chemotherapy:Anterior[induction] High response rate, less toxicity, provides prognostic information Delays locoregional treatment, Adjuvant chemotherapy:Posterior No delay in locoregional treatment Cannot be tolerated, effect of chemotherapy on the disease cannot be assessed Palliative concurrent
- 234. EVALUATION BEFORE CHEMOTHERAPY History and clinical examination Hematological Liver and renal function test X-ray chest ECG PET CT Scan Audiogram
- 235. DRUGS DOSAGE SIDE EFFECTS FOLLOW UP METHOTREXATE 40mg/m2, i.v weekly Bone marrow suppression, hepatotoxic , nephrotoxic Liver function test before use 5- FLUOROURACIL 10-15mg/kg , i.v. daily Myelo suppression, Mucositis, Skin changes Not gven in poorly nourished CYCLOPHOSPHAMIDE 60-90mg/m2, i.v. daily Heamorrhagic cystitis, Neutropenia, alopecia Adequate hydration BLEOMYCIN 10-20/m2 twice weekly, i.v, Pulmonary fibrosis, Anaphylaxis alopecia X-ray chest
- 236. ADRIAMYCIN 60-90mg/m2, iv every 30weeks Cardiotoxic, Alopecia Neutropenia, styomatitis ECG evaluation Red coloured urine CISPLATIN 80-120mg/m2, i.v. infusion every 3 weeks Nausea , vomiting, Peripheral neuropathy, Hematologic, nephrotoxic Renal function test, Adequate hydration VINCRISTINE 1.5mg/m2 , i.v. twice monthly, Neurotoxic, constipation hydration PACLITAXEL 135-150mg/m2, as3h infusion every 3 weeks Neutropenia, infection , peripheral neuritis Correcting neutropenia
- 238. CHEMORADIOTHERAPY Increased locoregional control Decreased risk of metastasis Improved survival Commonly used regimen: Cisplatin and 5- fluorouracil on day 1 and day22 of radiotherapy paclitaxel , docetaxel, ifosamide
- 239. CONCOMITANT CHEMOTHERAPY Single agent chemotherapy+ continuous course radiotherapy Combination chemotherapy +split course radiotherapy Alternating chemotherapy and radiotherapy Amelioration of side effects: Amifostine - free radical scavenging mechanism pilocarpine
- 240. LASER SURGERY Given via flexible endoscopes, straight or curved tubes.
- 241. Preferred in oropharyngeal and premalignant conditions of oral cavity, carcinoma of tongue{CO2 LASER}
- 242. Precise hemostasis Minimal post operative pain Rapid ablation of tissues High cost Special precautions Requires trained personnel ADVANTAGES DISADVANTAGES
- 243. PRECAUTIONS Display “lasers in use” No entry or exit permitted Protective glasses Wet saline pads on eyes Wet soaked towels to cover the exposed areas Endotracheal tubes should be covered Evacuation of smoke
- 244. CRYOSURGERY •Open method •Closed method •Dehydration •Denaturation •Thermal shock •Vascular stasis •Cryoimmunization
- 245. Anasthesia is not required Used for premalignant lesions Bleeding disorders/ coagulopathy Minimal postoperative pain and scarring Op procedure Multiple cancers, palliation of secondary cancers No tissue is available for biopsy No control on depth of freezing Skin changes and destruction of hair follicles Not possible to assess the margins of tumour Advantages: Disadvantages: Benign vascular tumours Premalignant lesions Malignant lesions
- 246. COBLATION Controlled or cold ablation Radiofrequency energy passed through saline Ionisation of high energy ions Create plasma field energy Breaks molecular bonds soft tisssue Tissue dissolution at low temperatures