More Related Content
Similar to Vasculitis nrrheum.2014.67 (20)
More from Elsa von Licy (20)
Vasculitis nrrheum.2014.67
- 1. 502 | AUGUST 2014 | VOLUME 10 www.nature.com/nrrheum
Introduction
Vasculitides encompass large, medium and
small-vessel vasculitis, including a number
of rare diseases with multisystem presenta-
tions.1
Other than those with an infectious
aetiology, most vasculitides are thought to
be autoimmune in origin and are treated
by inducing immunosuppression.2
How
ever, immunosuppressant therapies have
been associated with infection, leukopenia
and certain types of malignancy, whilst
corticosteroid use is associated with several
complications including infection, weight
gain, diabetes mellitus and osteoporosis.3,4
A need exists not only to define effective
therapies and evaluate new therapeutics for
vasculitis, but also to refine existing treat
ments to minimize the exposure of patients
to excessive immunosuppression. Several
examples are available of successful clini-
cal trial execution in vasculitis, especially
in antineutrophil cytoplasmic antibody
(ANCA)-associated vasculitis (AAV), and
these examples have formed the evidence
base for our current management protocols.
In large-vessel vasculitis (LVV), the clini-
cal trial evidence for management is weaker
than trial data for AAV; however, the field
is moving forward with the establishment
of multicentre collaborations, initiatives to
standardize diagnostic criteria, and valida-
tion of noninvasive imaging modalities and
outcome measures. The commencement of
a large multicentre randomized controlled
trial (RCT) of tocilizumab in giant-cell
arteritis (GCA; GiACTA)5,6
will, it is hoped,
demonstrate the feasibility of such studies
in LVV and facilitate further advances.
RCTs performed for AAV and LVV to date,
issues in trial design and challenges for the
future are discussed in this Opinion article.
Prerequisites for trials
Box 1 lists the prerequisites for RCTs in vas-
culitis. We have chosen to focus on AAV and
LVV because these are the most common
forms of vasculitis in adults, for which most
data are available, but these diseases illus-
trate the issues in clinical trial design for all
forms of vasculitis.
Multicentre collaborations
Rare diseases often require multicentre
trials to have sufficient statistical power to
answer important therapeutic questions;
such trials might need organization and
collaboration across national borders,
and might necessitate longer recruitment
periods than trials in more common dis-
eases. International conferences, the internet
and the drive of medical leaders to spear-
head clinical trials have had an important
positive effect. Disease registries enabling
rapid identification of eligible patients
are also beneficial, as are disease interest
groups that bring together specialists with
a common interest in improving thera-
pies. Broad consensus and support for the
protocols are required in order for recruit-
ment at multiple sites to be successful. This
consensus can be difficult to achieve as
local variations in management protocols
exist, especially when the evidence base is
limited. In particular, differences of opinion
on the appropriate dosing, rate of tapering
or discontinuation of corticosteroids can
be an issue in vasculitis trials. Funders and
stakeholders (including local investigators)
need to have a vested interest in the success
of clinical trials because of a genuine inter-
est in the results and recognition of their
individual input in publication reports. The
development of new biologic agents has
helped to foster collaborations between the
pharmaceutical industry and academia to
address unmet needs in rare diseases. How
ever, the rapid recruitment targets some-
times required by industry have, in our
experience, also led to difficulties in some
clinical trials in vasculitis because of slow
patient recruitment.
Efficient trial design
Limitations on available patients and
resources mean that it is important to define
the most pressing questions to address and
to predict how relevant the answer will be
at the end of the trial, which can be up to
5 years from inception. In some circum-
stances, more than one question can be
addressed at once. For example, factorial
design of the PEXIVAS trial will hopefully
answer two questions, namely the roles of
plasma exchange and of glucocorticoid
dosing in AAV.7,8
Newer methods for clini-
cal trial design (including computerized
algorithms to avoid bias) are important,
and the development of electronic case
report forms and adverse-event reporting
has streamlined the processes. Traditional
trial designs, with fixed protocols in which
data are analysed at the termination of
the experiment, are mainly required for
licensing new medicines. However, there is
increasing interest in adaptive trial design in
early-phase experimental medicine studies
using Bayesian statistics to enable interim
OPINION
Issues in trial design for ANCA-associated
and large-vessel vasculitis
Ruth M.Tarzi, Justin C. Mason and Charles D. Pusey
Abstract | Randomized clinical trials (RCTs) have informed the management of
antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis, although challenges
still exist. The evidence base for treating large-vessel vasculitis (LVV) is weaker, but
initiatives to standardize diagnostic criteria and outcome measures, and to validate
biomarkers in LVV, together with newly initiated RCTs should start to address this
need. In this Perspectives, we discuss the prerequisites for RCTs in vasculitis, existing
trial evidence, continuing unmet needs, potential therapeutic avenues to explore and
considerations in the design of future trials.
Tarzi, R. M. et al. Nat. Rev. Rheumatol. 10, 502–510 (2014); published online 6 May 2014;
doi:10.1038/nrrheum.2014.67
Competing interests
C.D.P. has received a research grant from
GlaxoSmithKline. R.M.T. and J.C.M. declare no
competing interests.
PERSPECTIVES
© 2014 Macmillan Publishers Limited. All rights reserved
- 2. NATURE REVIEWS | RHEUMATOLOGY VOLUME 10 | AUGUST 2014 | 503
analyses and the use of information gained
during the trial to modify the study proto-
col.9
In this way, more information can be
gained from a smaller pool of patients. This
approach has been taken with the CLEAR
study, assessing a C5a receptor antagonist
in AAV.10
Inclusion criteria
Inclusion criteria for any trial need to
be well defined. In vasculitis, however,
evidence-based diagnostic criteria do not
exist. Notably, the ACR classification cri-
teria do not include specific criteria for
microscopic polyangiitis11
and the Chapel
Hill Consensus Conference definitions1
are often used, although they are formed
by consensus rather than being evidence-
based and do not include classification cri-
teria. The DCVAS study (Diagnostic and
Classification Criteria in Vasculitis Study)
is an observational cohort study with the
aim of developing evidence-based diagnos-
tic criteria for vasculitic conditions; results
are awaited.12
The need for multiple sites
in trials means that the inclusion criteria
must be well defined, and ideally include
‘hard’ criteria such as laboratory data or
histological confirmation. When present,
a positive ANCA test is a useful diagnos-
tic marker for AAV, but specific serologi-
cal biomarkers for LVV are not available.13
Whereas a biopsy is usually performed to
confirm diagnosis in suspected AAV, histo-
logical confirmation is not always obtained
in the setting of characteristic features and
a positive ANCA test, particularly in the
setting of life-threatening disease. In LVV,
arterial specimens are only collected from
patients with Takayasu arteritis undergoing
surgery; notably, insistence on histological
confirmation by temporal artery biopsy in
a GCA trial hindered recruitment.14
When
biopsy-obtained tissue is available, central
review of histological specimens is impor-
tant to standardize assessments and confirm
the diagnosis, and to stratify responses to
therapy on the basis of histological stage.
A histological categorization system has
been developed that separates patients
with glomerulonephritis owing to AAV
into crescentic, focal, sclerotic or mixed
groups according to analysis of renal biopsy
samples.15
This scoring system is being
validated to determine whether the histo-
logical subgroups correlate with outcome.
The ability to stratify disease is important
to define more-homogeneous populations
who might need to be managed differently.
In AAV, the approach taken has been to
stratify patients on the basis of the severity
of their clinical presentation, and perform
separate trials of management of severe,
generalized and early systemic AAV.
Outcome measures and end points
Clinically meaningful outcome measures for
vasculitis trials need to be validated, to act as
end points that will be recognized by regu
latory agencies. The Outcome Measures
in Rheumatology group (OMERACT) has
developed guidelines for the assessment of
potential outcome measures in rheumatic
diseases, based on three principles: truth,
discrimination and feasibility. In evaluat-
ing renal end points, hard composite end
points (of death or end-stage renal disease)
or doubling of serum creatinine level have
been used. However, when multisystem
disease manifestations are being studied,
these outcomes are not sufficient. For AAV,
OMERACT has provided an analysis of the
available outcome measures and their valid-
ity based on its three principles.16
Poten
tial outcome measures for LVV are being
evaluated by OMERACT.17
Robust means to monitor disease activ-
ity and damage across multiple organ sites
and systems are required for vasculitis
trials. These tools require standardized
definitions of disease activity and damage,
and they should be sensitive to change and
detect clinically relevant differences that
would signal a modification in therapy.
The Birmingham Vasculitis Activity Index
(BVAS)18
and subsequent iterations (includ-
ing the BVAS 3 and BVAS/WG) have been
endorsed by OMERACT for AAV. The Dis
ease Extent Index19
is another disease activ-
ity index that has been used in AAV trials.
BVAS was originally designed as a univer-
sal vasculitis activity index, but the utility
of BVAS for vasculitides other than AAV
has not been well established. A Paediatric
Vasculitis Activity Index has now been
developed,20
and is currently undergoing
validation. The Vasculitis Damage Index
and the Combined Damage Assessment
Index (CDA) are used to assess damage
in AAV across multiple organ systems,21,22
although one study found that the Vasculi
tis Damage Index was less time-consuming
to complete than the CDA and captured
similar information.22
For induction trials, remission rates
are commonly used as an end point, and
in maintenance trials, time to relapse or
relapse event rates are often used. However,
definitions of remission and relapse vary.
For example, in the RAVE trial comparing
rituximab to cyclophosphamide for remis-
sion induction, remission was based on the
absence of clinical features and no gluco
corticoid use, whereas in the RITUXVAS
trial, examining the same question, treat-
ment was not part of the end point.23,24
Vari
ations in end points between trials can make
comparisons between trials difficult, hence
the importance of agreement and standard-
ization in analysis and reporting of trials.
Surrogate end points using biomarkers, such
as C‑reactive protein (CRP) or erythrocyte
sedimentation rate (ESR) levels, proteinu-
ria and haematuria are sometimes used in
proof-of-concept studies. For definitive
studies, there is a need to demonstrate that
the biomarker in use is predictive of the
clinical outcomes of interest.
Cost-effectiveness
Cost-effectiveness is an important aspect to
consider when designing clinical trials, par-
ticularly with expensive interventions such
as biologic therapies. Cost-effectiveness
analysis is based on the cost per quality-
adjusted life-year gained by the treatment,
compared with conventional therapy. It is
therefore mandatory to include assessments
of quality of life as one of the outcomes of
clinical trials. The patient-reported out-
comes form Short-Form 36 is widely used;
interestingly, a patient-reported outcome
measure that is specific for vasculitis is
under development.16
Populations studied
In clinical trials, the question always arises
of whether the patients recruited truly
mirror the population being studied. The
AAV and LVV populations include large
numbers of elderly patients with comorbidi-
ties, who can sometimes be excluded from
Box 1 | Vasculitis clinical trial prerequisites
■■ Robust multicentre collaborations
■■ Funding from government, charities
or industry
■■ Address clinically important questions
■■ Achievable recruitment targets
■■ Protocols agreed by consensus,
comparing to standard best practice
■■ Clear diagnostic criteria
■■ Inclusion criteria clearly defined
■■ Stratification for severity of disease
and/or disease manifestations possible
■■ Activity and damage indices and quality
of life measures designed and validated
■■ Validated outcome measures and/or
end points
■■ Stakeholders, including investigators
and funders, motivated and engaged
FOCUS ON VASCULITIS
© 2014 Macmillan Publishers Limited. All rights reserved
- 3. 504 | AUGUST 2014 | VOLUME 10 www.nature.com/nrrheum
clinical trials for these reasons alone.25
It is
therefore important to bear this in mind
and for the trials to be as inclusive as pos-
sible to enable them to assess the true clini-
cal importance of the therapies being tested.
A move towards greater transparency in
access to patient-level clinical trial data,
both in the academic and pharmaceutical
sector, is gaining momentum.26,27
When
trial results are negative, publication can
sometimes be more difficult, but negative
results can have important implications in
avoiding ineffective therapies. As patients
enter clinical trials altruistically, consid-
eration of the ethics dictate that the data
generated should be fully utilized.
Trials of therapy in AAV
The introduction of cyclophosphamide in
the 1970s changed AAV from a disease with
a high mortality to a relapsing–remitting
chronic condition.28
However, the high
incidence of adverse effects associated with
large cumulative doses of cyclophospha-
mide provided the impetus for clinical trials
to establish less toxic, but nevertheless effec-
tive, treatments.29,30
A number of organiza-
tions, including national and international
vasculitis societies in Europe and the USA
have driven a number of successful multi-
centre RCTs in AAV over the past 20 years.
In particular, several trials have been organ-
ized by the European Vasculitis Society,
whose premise has been to subgroup vas-
culitis according to severity, give high-
intensity treatment to induce remission
and low-intensity immunosuppression to
prevent relapse, to agree a standard regimen
by consensus, to test against the best alter-
native by RCT and to use standardized
scoring systems.
Table 1 lists the multicentre RCTs for
induction and remission maintenance ther
apy that have been completed in AAV and
summarizes their outcomes; Supplemen
tary Table 1 online lists multicentre RCTs
in AAV that are ongoing or just completed
and not yet published.
Successes
RCTs in AAV have been successful in pro-
viding an evidence base for the current
management protocols, which is a major
achievement in these rare diseases. The
results of the trials have reduced exposure
of patients with AAV to cyclophosphamide,
which has helped to improve long-term
outcomes, as evidenced by the reduced
incidence of late-onset malignancy in
current patients with AAV when compared
with historical cohorts.4,30
The success of
early trials has proven to funders that large
multicentre RCTs in rare vasculitic diseases
are possible, and facilitated funding of the
current generation of clinical trials in vas-
culitis. Although the individual trials were
not able to capture events such as mortal-
ity, long-term malignancy risk and chronic
damage, later analysis and pooling of results
from a number of trials have enabled these
questions to be addressed.3,4,31
The RAVE and RITUXVAS trials have
established that rituximab is noninferior
to cyclophosphamide for induction of
remission in AAV,23,24
adding an alternative
option for patients in whom cyclophospha-
mide avoidance is desirable. Even larger
global collaborations are now occurring, in
terms of the number of centres and patients
involved in current RCTs; for example, the
PEXIVAS trial7,8
and the RITAZAREM
trial.32
Academic and industry collabora-
tions have also been helpful for funding the
use of expensive biologic therapies in RCTs
and the vasculitis trials have also enabled
the collection of serum, plasma, DNA and
cellular samples from well-characterized
cohorts of patients, which is an invaluable
tool for biomarker research.
Issues to consider
Owing to the rarity of AAV, most of the
trials to date have included patients with
both granulomatosis with polyangi
itis (GPA) and microscopic polyangiitis
(MPA). Although some of the clinical fea-
tures overlap, there are notable differences.
For example, granulomatous manifesta-
tions do not occur in MPA, and the patho
genesis of granulomatous disease and time
course of response to treatment probably
differs from ‘pure’ vasculitis.33
In addition,
GPA is substantially more prone to relapse
than MPA.34
GPA and MPA have been con-
firmed as different diseases with different
MHC susceptibilities in a genome-wide
association study published in 2012.35
The
study also demonstrated that the genetic
associations were more robust for the bio
markers myeloperoxidase (MPO)-ANCA
and proteinase 3 (PR3)-ANCA rather than
the clinical phenotypes of MPA and GPA.
In view of this finding, and the fact that
none of the clinical algorithms currently in
use reliably distinguishes MPA from GPA,
it has been proposed that ANCA status be
used to stratify patients rather than the
clinical phenotypes.36
In future trials, it will
be important to assess outcomes of MPA
and GPA, or MPO-ANCA and PR3-ANCA
disease, separately, particularly in trials
of remission maintenance; it might also
be time to consider whether trials should be
designed to address whether GPA and MPA
should be treated differently.
Because of their short follow-up, results
of initial RCTs in AAV have varied to some
extent from those of long-term follow-up
studies. However, caution should be exer-
cised in interpreting the results of long-term
follow-up data that have been collected
retrospectively after the end of the trials,
as these data are weaker and should not be
used to contest the primary end point of the
properly controlled RCT. In the CYCLOPS
study in AAV, no difference was obser
ved in the rate of remission between the
intravenous and oral cyclophosphamide
groups.37
However, the long-term analysis
(average follow-up 4.3 years) subsequently
demonstrated a higher relapse rate in
the intravenous cyclophosphamide group,
although there was no notable difference
in survival or renal function at long-term
follow-up.38
The MEPEX trial was designed
to assess dialysis independence at 3 months
in patients with AAV and serum creatinine
level 500 μmol/l. Although benefit from
plasma exchange in terms of this end point
was achieved and maintained to 12 months,
follow-up for a median of 3.95 years dem-
onstrated no difference in mortality.39,40
This uncertainty has led to the design
of the PEXIVAS trial, recruiting a larger
number of patients (n = 500), and hopefully
this study will definitively answer the ques-
tion of when plasma exchange is indicated
in AAV with glomerulonephritis.7
The
REMAIN trial—a remission maintenance
trial addressing the length of maintenance
therapy in GPA—was instigated in 2003,
but the answers have been substantially
delayed, as recruitment, follow-up and
reporting has taken 10 years.41
This delay
challenges the motivation of investigators,
and the need to demonstrate outcomes to
employers and funders.
Future directions
Several trials in AAV are ongoing or not
yet published (Supplementary Table 1).
Priorities that we feel need to be addressed
in current and future clinical trials in AAV
are listed in Box 2. For example, infections
continue to be the most common cause of
mortality in patients within the first year
after diagnosis of AAV,42
and no reduction
in infections was seen in the rituximab-
treated groups versus the cyclophosphamide
arms in the RAVE or RITUXVAS trials.23,24
PERSPECTIVES
© 2014 Macmillan Publishers Limited. All rights reserved
- 4. NATURE REVIEWS | RHEUMATOLOGY VOLUME 10 | AUGUST 2014 | 505
Table 1 | Published multicentre RCTs in AAV
Trials Indication Trial design* Primary end point Brief results
Induction trials
NORAM64,65
Newly diagnosed GPA
or MPA, with early
systemic involvement
Induction: trial, oral methotrexate 15–25 mg
per week + tapering Pred (n =51); control,
oral cyclophosphamide 2 mg/kg per day*
(tapering to 1.5 mg per day once remission
attained) + tapering Pred (n = 49)
All treatment discontinued by 12 months
Remission at
6 months
Methotrexate noninferior
to oral cyclophosphamide
in inducing remission
at 6 months, but
relapse rate higher in
methotrexate group at
18 months
CYCLOPS37,38
GPA or MPA with renal
involvement, but serum
creatinine 500 μmol/l
Induction: trial, IV cyclophosphamide 15 mg/kg
for 2–3 weeks + tapering Pred (n = 76);
control, oral cyclophosphamide 2 mg/kg per
day* + tapering Pred (n = 73)
Maintenance: azathioprine 2 mg/kg per
day + Pred
Time to remission IV cyclophosphamide
noninferior to oral
cyclophosphamide with
lower cumulative dose
Less leukopenia in
IV group
MEPEX39,40
Severe renal GPA or MPA
with serum creatinine
500 μmol/l
Induction: trial, PLEX + oral cyclophosphamide
2.5 mg/kg per day reducing to 1.5 mg/kg per day
at 3 months + Pred (n = 70); control IV methyl
Pred 1 g daily for 3 days + oral cyclophosphamide
2.5 mg/kg per day reducing to 1.5 mg/kg per day
at 3 months + Pred (n = 67)
Maintenance: azathioprine 2 mg/kg + Pred
Dialysis independence
at 3 months
Renal survival better with
PLEX than IV methyl Pred
No difference in safety
or mortality
RITUXVAS24
Newly diagnosed GPA or MPA
with renal involvement
Induction: trial, rituximab 375 mg/m2
per week for
4 weeks + Pred + IV cyclophosphamide 15 mg/kg
(weeks 0 and 2) (n = 33); control, IV
cyclophosphamide 15 mg/kg + Pred (n = 11)
Maintenance: Pred alone (rituximab group) or
azathioprine + Pred (cyclophosphamide group)
Sustained remission
at 12 months and
adverse event rates
Rituximab noninferior to
IV cyclophosphamide;
no difference in adverse
event rate
RAVE23,66
New or relapsing GPA or MPA
(excluding serum creatinine
4.0 mg/dl [equivalent to
~354 μmol/l], or pulmonary
haemorrhage)
Induction: trial, rituximab 375 mg/m2
per week for
4 weeks + Pred (n = 99); control, oral
cyclophosphamide 2 mg/kg + Pred (n = 98)
Maintenance: Nil (rituximab group) or azathioprine
2 mg/kg (IV cyclophosphamide group)
Remission without
Pred at 6 months
Rituximab noninferior to
oral cyclophosphamide
Rituximab more effective
than cyclophosphamide in
relapsing patients
Maintenance trials
CYCAZAREM67
GPA or MPA, new or relapse
with renal or multiorgan
involvement
Induction: cyclophosphamide 2 mg/kg per
day + tapering Pred
Maintenance: trial, azathioprine 2 mg/kg per day
+ 10 mg Pred (n = 71); control, oral
cyclophosphamide 1.5 mg/kg once daily + 10 mg
Pred (n = 73)
Relapse rate No difference in relapse
rate
IMPROVE68
Newly diagnosed GPA or MPA Induction: oral or IV cyclophosphamide (as per
CYCLOPS above) + Pred
Maintenance: trial, MMF 2 g per day + tapering
Pred (n = 76); control, azathioprine 2 mg/kg per
day + tapering pred (n = 80)
Relapse-free survival MMF less effective than
azathioprine in
maintaining remission
No difference in adverse
events
WEGENT69
GPA or MPA with renal or
multi-organ involvement
Induction: IV cyclophosphamide 15 mg/kg every
2–3 weeks + tapering Pred
Maintenance: trial, methotrexate (up to 25 mg
per week) + tapering Pred (n = 63); control,
azathioprine 2 mg/kg per day + tapering Pred
(n = 63)
Adverse event causing
treatment cessation
or death
No difference between
azathioprine and
methrotrexate in adverse
events or relapse
WGET70
GPA and BVAS 3 Induction: oral cyclophosphamide 2 mg/kg or
methotrexate 0.25 mg/kg per week, up to 25 mg
per week + Pred
Maintenance: trial, methotrexate up to 25 mg per
week + etanercept 25 mg subcutaneously twice a
week (n = 89); control, methotrexate up to 25 mg
per week (n = 92)
Remission for
6 months
Addition of etanercept
failed to improve
remission rates
German Network
of Rheumatic
Diseases study71
GPA and serum creatinine
level 1.3 mg/dl (equivalent
to ~115 μmol/l)
Induction: oral cyclophosphamide 2 mg/kg per
day + Pred
Maintenance: trial, leflunomide 30 mg per
day + Pred (n = 26); control, methotrexate
7.5–20 mg per week + Pred (n = 28)
Relapse Leflunomide more
effective than
methotrexate in
maintaining remission,
but with more adverse
events
*Cyclophosphamide doses adjusted for age and renal function in all of the trials. Abbreviations: AAV, antineutrophil cytoplasmic antibody-associated vasculitis; BVAS, Birmingham Vasculitis
Activity Score; GPA, granulomatosis with polyangiitis; IV, intravenous; MMF, mycophenolate mofetil; MPA, microscopic polyangiitis; Pred, prednisolone or prednisone; PLEX, plasma exchange;
RCT, randomized controlled trial.
FOCUS ON VASCULITIS
© 2014 Macmillan Publishers Limited. All rights reserved
- 5. 506 | AUGUST 2014 | VOLUME 10 www.nature.com/nrrheum
A reduction in corticosteroid exposure
might be an avenue to explore in this regard.
The PEXIVAS and CLEAR studies are both
investigating whether reductions in steroid
exposure are possible in AAV induction
therapy. Another issue to address is the man-
agement of frequent relapse, which is espe-
cially common in those with granulomatous
upper airway disease, who can often be
exposed to several courses of induction
treatment during their lifetime, with atten-
dant treatment-related comorbidity and the
potential for cumulative disease-induced
damage. The RITAZAREM trial is examin-
ing whether repeated dosing of rituximab
will have an effect on relapse rates in AAV
compared with azathioprine.32
A number of
other biologic agents targeting pathways
of importance in the pathogenesis of AAV
are available, some of which are currently
under evaluation (Figure 1). Ultimately, a
means to restore immunological tolerance
in AAV is required.
Trials in eosinophilic granulomatosis with
polyangiitis (EGPA) are scarce, owing to its
rarity when compared with GPA and MPA.43
Glucocorticoids are effective for nonsevere
presentations, but patients with cardiac,
neurological or renal involvement with a
five-factor score of ≥1 have been shown to
benefit from the addition of cyclophospha-
mide to the steroid-containing regimen.44
Reports of successful treatment of EGPA
with rituximab are available, but no RCT at
present.45,46
A trial of the anti-IL‑5 mono
clonal antibody mepolizumab in EGPA is
now recruiting.47
Clinical trials in LVV
LVV is characterized by granulomatous
inflammation in the aorta and its major
branches.48
The two main forms of LVV are
GCA, which is reasonably common, with
an incidence of 7–29 per 100,000 in white
Europeans 50 years old, and Takayasu
arteritis, which is rare, with an incidence of
3 per 1 million population, and presents
predominantly in women 40 years of
age.48,49
Clinical trials including therapies
other than corticosteroids in LVV com-
pleted to date and their major findings are
listed in Table 2; trials in progress are listed
in Supplementary Table 2.
Issues to consider
Imaging
The gold standard for diagnosis of GCA is
evidence of arteritis in a temporal artery
biopsy sample. The TABUL trial is cur-
rently evaluating whether colour Doppler
ultrasonography is sensitive and specific
for this condition, and whether it might,
in due course, represent a less-invasive
diagnostic technique.50
A study suggests
that this benefit might indeed be the case,
which will help standardize clinical trial
recruitment.51
Moreover, advances, avail-
ability and understanding of the role of
other noninvasive imaging modalities,
including contrast-enhanced MRI, CT
Box 2 | Priorities for future clinical trials in vasculitis
AAV
■■ Development of biomarkers for the identification of patients with AAV at risk of relapse
■■ Corticosteroid minimization protocols to reduce steroid-induced adverse-effect burden
■■ Refinements to reduce the toxicity of induction therapy for elderly patients
■■ Therapeutics with faster speed of onset of action for induction therapy
■■ Therapies with faster speed of onset in granulomatous disease
■■ Trials addressing the management of the maintenance phase of PR3-ANCA and MPO-ANCA
disease as separate entities
■■ More-effective maintenance strategies for relapsing patients
■■ Therapies to re-establish immunological tolerance
LVV
■■ Clear definition of outcome measures and the role of imaging in clinical trials
■■ Development of biomarkers to enable patient stratification in GCA at diagnosis
■■ Development of biomarkers for the identification of patients with LVV at risk of relapse
■■ Corticosteroid minimization protocols to reduce steroid adverse-effect burden
■■ Trials to address the role of adjunctive immunosuppressive therapy in GCA and Takayasu
arteritis (e.g. methotrexate as a steroid-sparing drug)
■■ Development of international clinical trial networks for LVV including patients from Asia,
Europe and the Americas
Abbreviations: AAV, ANCA-associated vasculitis; ANCA, antineutrophil cytoplasmic antibody; GCA, giant-cell
arteritis; LVV, large-vessel vasculitis; MPO, myeloperoxidase; PR3, proteinase 3.
C5a
Myofibroblast
Vascular DC
C5a–C5aR
Eculizumab
CCX168
BAFF–APRIL
Belimumab
Atacicept
Veltuzumab
Ocrelizumab
Ofatumumab
Rituximab*
CD20
Epratuzumab
CD22
Everolimus
Sirolimus
mTOR
Belatacept
Abatacept
CTLA-4
TH
17
cell
TH
1
cell
IL-6–IL-6R
Tocilizumab
IL-1–IL-1R
Anakinra
Canakinumab
Macrophage
ANCA
Neutrophil
SYK
Fostamatinib
Ustekinumab
Briakinumab
IL-12/IL-23
Belatacept
Abatacept
CTLA-4
Brodalumab
Ixekizumab
Secukinumab
IL-17
AAV targets
TH
17 response
B cells
Auto-antibody production
Co-stimulation
Inflammatory cells
Complement
Fcγ receptors
Cytokines
LVV targets
TH
1 response
Vascular DC activation
Cytokines
Inflammatory cells
Myofibroblast proliferation
Reactive oxygen species
Neovascularization
B cell
IFN-γ
Fontolizumab
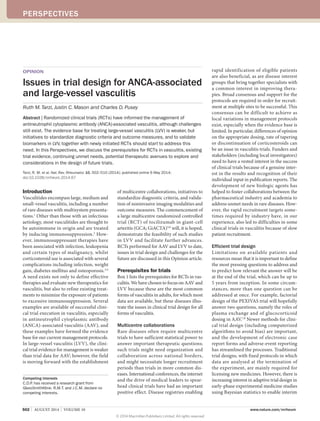
Figure 1 | Potential therapeutic targets in AAV and LVV. Schematic diagram showing potential
therapeutic targets in AAV and LVV, including examples of biologic therapies and small-molecule
inhibitors targeting these pathways. *Of these agents, only rituximab is licensed for the
treatment of AAV, whereas several of the other agents are under evaluation. Abbreviations: AAV,
ANCA-associated vasculitis; ANCA, antineutrophil cytoplasmic antibody; APRIL, a proliferation-
inducing ligand (also known as TNF ligand superfamily member 13); BAFF, B-cell activating factor
of the TNF family (also known as TNF ligand superfamily member 13B); CTLA-4, cytotoxic
T-lymphocyte protein 4; DC, dendritic cell; LVV, large-vessel vasculitis; mTOR, mammalian target
of rapamycin; SYK, spleen tyrosine kinase; TH
(cell), helper T (cell).
PERSPECTIVES
© 2014 Macmillan Publishers Limited. All rights reserved
- 6. NATURE REVIEWS | RHEUMATOLOGY VOLUME 10 | AUGUST 2014 | 507
angiography and 18
FDG-CT-PET might
also facilitate trials in LVV, particularly if
they can be shown to correlate with disease
activity or damage and be incorporated into
appropriate disease-scoring systems.49
Outcome measures
Disease activity indices for LVV are less
developed than for AAV, which has made
clinical trial implementation difficult.
A particular problem has been the identi-
fication of valid biomarkers to distinguish
active disease from damage. An initiative to
develop a core set of outcome measures for
use in clinical trials of LVV was launched
by the international OMERACT Vasculitis
Working Group in 2009.17
In addition, The
Indian Takayasu Clinical Activity Score
(ITAS2010) was published in 2013 and
validated in 300 patients with Takayasu
arteritis.52
Multiple different end points
have been used in clinical studies of LVV;
the main categories used in clinical trials
for GCA relate to clinical outcomes (time
to remission, time to relapse, relapse rates),
laboratory measures and glucocorticoid-
sparing effects. However, some of the clini
cal outcomes are rather vague and subjective
(fatigue, headache, arthralgia), whereas
other manifestations can be asymptomatic
until later stages when they are irreversible
(for example, sudden-onset visual loss).
Steroid tapering
Standard treatment of GCA with cortico
steroids is highly effective in inducing
remission,48
but relapses on steroid taper-
ing are common, and the need to avoid the
adverse effects of prolonged steroid courses
in elderly patients has provided an impetus
to develop steroid-sparing regimens. Trials
of adalimumab and etanercept in GCA have
proven negative.14,53,54
Trials using metho-
trexate as a steroid-sparing agent in GCA
have given conflicting results. Mahr et al.55
performed a meta-analysis of three placebo-
controlled trials (comprising a total of 161
patients across the three trials) of patients
with new-onset GCA who were randomly
assigned to either corticosteroids alone or
with the addition of methotrexate or placebo.
Despite the mean dose of methotrexate over
the total period of intake being lower than
the recommended dose at only 11.1 mg per
week, a steroid-sparing effect in GCA was
found.55
However, further analysis of these
trials, and indeed many vasculitis studies,
raises the important and unresolved issue
of optimal corticosteroid-tapering schemes.
In all vasculitis trials, decisions regard-
ing steroid-tapering protocols are challeng-
ing. A balance needs to be drawn between
the desire to optimise the chance of dem
onstrating a beneficial effect of adjunctive
therapy, and too rapid a reduction in the
corticosteroid dose with the associated risk
of disease flare and complications. Likewise,
too cautious tapering might mask the bene
ficial effect of a new therapeutic approach.
The three trials designed to assess the role
of methotrexate in the treatment of GCA
illustrate this problem.56–58
These trials
used different steroid-reduction regimens,
all of which were more rapid than many
practitioners would use in clinical practice.
Relapse rates were fairly high, with 61%
and 29% of patients experiencing a first and
second relapse, respectively.55
In particular,
a switch to alternate-day prednisone dosing
seemed to lead to a high incidence of vision
loss.56
Ideally, steroid-tapering regimens
for future studies should be consistent.
Two possible approaches might be consid-
ered. The first would be to adopt a standard
Table 2 | Published RCTs of therapeutics in LVV, excluding trials of steroid dosing alone
Trials Indication Trial design Primary end point Brief results
Induction trials
Jover et al.
(2001)57
Biopsy-proven
new-onset GCA
Induction: trial, 10 mg methotrexate weekly plus
Pred (tapering) (n = 21); control, placebo plus
Pred (tapering) (n = 21)
Number of disease
relapses and
cumulative
corticosteroid dose
Substantial reduction in relapses
and reduced corticosteroid dose
in methotrexate group at
24 months
Speira et al.
(2001)58
Biopsy-proven
new-onset GCA or ESR
50 mm/h and clinical
features
Induction: trial, methotrexate 7.5–20 mg per
week plus Pred (n = 12); control, placebo plus
Pred (n = 9)
Cumulative
corticosteroid dose
No statistically significant
difference in corticosteroid
dosage between the groups at
12 months
Only one major relapse occurred
Hoffman et al.
(2002)56
Patients 50 years old
with diagnosis of GPA
within 6 months of
entry by biopsy or
clinical features and
raised ESR level
Induction: trial, methotrexate median dose
15 mg per week plus Pred (tapered off by
6 months) (n = 51); control, placebo plus Pred
(tapered off by 6 months) (n = 47)
First relapse and
treatment failure rates
No notable difference in treatment
failures between the groups
Seror et al.
(2013)14
Patients 50 years old
with new-onset GCA
Induction: trial, adalimumab (40 mg every
2 weeks) for 10 weeks + tapering Pred (n = 34);
control, placebo plus tapering Pred (n = 36)
Remission on 0.1 mg/
kg Pred at week 26
Adjunctive adalimumab did not
increase the proportion of
patients achieving the end point
Maintenance trials
Infliximab-GCA
study group
(2007)53
Newly diagnosed GCA
with ESR 40 mm/h
and clinical criteria for
GCA in corticosteroid-
induced remission
Induction: Pred
Maintenance: trial, infliximab 5 mg/kg IV
(week 0, 2, 6 then every 8 weeks) + Pred
tapering over 24 weeks (n = 28); control,
placebo + Pred tapering over 24 weeks (n = 16)
Number of patients
relapse free at week 22
and adverse events
No benefit of infliximab in reducing
relapse rates
Etanercept trial
in GCA (2008)54
Biopsy-proven GCA in
remission with
corticosteroid-induced
adverse effects
Induction: Pred
Maintenance: trial, etanercept 25 mg
subcutaneous twice a week plus Pred
(tapering; n = 9); control, placebo plus
Pred (tapering; n = 8)
Rates of steroid
discontinuation with
controlled disease at
12 months
No statistically significant
difference in percentage of
patients steroid-free at 12 months
(50% vs 22%), but small patient
numbers
Abbreviations: ESR, erythrocyte sedimentation rate; GCA, giant cell arteritis; IV, intravenous; LLV, large-vessel vasculitis; Pred, prednisone or prednisolone; RCT, randomized controlled trial.
FOCUS ON VASCULITIS
© 2014 Macmillan Publishers Limited. All rights reserved
- 7. 508 | AUGUST 2014 | VOLUME 10 www.nature.com/nrrheum
protocol described in guidelines such as
those proposed by the British Society for
Rheumatology.59
Second, the GiACTA trial
will compare two clearly defined prednisone
tapering regimens, the first a rapid reduction
from 60 mg to withdrawal over 26 weeks,
and the second, which is more representa-
tive of clinical practice, with tapering from
60 mg to 1 mg over 52 weeks.5
Recruitment
A trial of adjunctive adalimumab in GCA
published in 201314
illustrates some of the
problems in recruiting to clinical trials. Initi
ally, the trial required histological confirma-
tion of GCA with temporal artery biopsy, but
this criterion was dropped during the trial
because of slow recruitment of participants.
Statistical power calculations suggested that
100 patients were required, but due to slow
recruitment the trial was terminated after
recruiting 70, 10 of whom had not received
their allocated therapy. This difficulty in
recruitment reduced the power of the study
to 72%, although it is questionable whether
it affected the outcome.14
Trials in progress
The GiACTA trial, an RCT of the anti-IL‑6
receptor antibody tocilizumab in GCA, has
started recruiting; it is the largest RCT in
GCA to date, aiming to recruit 250 patients
over 100 centres worldwide (Supplemen
tary Table 2).5,6
In this trial, the entry cri
teria include either positive temporal artery
biopsy, or evidence of LVV by noninvasive
imaging with magnetic resonance angio
graphy, CT angiography or CT‑PET. These
criteria represent an important change for
GCA trials and should improve the homo-
geneity of the study population, compared
with reliance on clinical criteria, as positive
biopsies are often not obtained. The trial will
use the absence of GCA symptoms, together
with normal levels of ESR and CRP, as the
primary efficacy end point at 52 weeks; how
ever, it is important to note that the effect
of IL‑6 inhibition on the synthesis of acute-
phase reactants, including potent suppres-
sion of CRP, might not necessarily reflect
control of inflammation in the arterial
wall. A second trial currently recruiting is
the ABVAS trial, evaluating the efficacy of
abatacept in treating GCA and preventing
disease relapse (Supplementary Table 2).60
In Takayasu arteritis, no RCTs have been
completed to date, which reflects the rarity
of the disease, the lack of suitable activity
and damage indices, and difficulty sur
rounding selection of suitable end points.
The ABVAS trial is underway and aims to
evaluate abatacept in treating both GCA
and Takayasu arteritis.60
Hopefully, if this
trial is successful, it will enable trials of other
potential therapies, such as TNF inhibitors
and tocilizumab to be formally evaluated
in Takayasu arteritis. Evidence from small
open-label studies of the latter biologic
agents in patients with refractory Takayasu
arteritis are encouraging and reveal pro-
longed efficacy.61–63
However, important
caveats remain surrounding biologic thera-
pies in Takayasu arteritis, including whether
tocilizumab attenuates arterial wall inflam-
mation, in addition to suppressing the acute-
phase response. Multinational RCTs are now
required to generate convincing evidence of
efficacy for both anti-TNF and anti-IL-6
receptor therapies.
Future directions
The paucity of clinical trials in LVV and the
lack of progress when compared with AAV,
although in urgent need of redress, empha-
sises the considerable challenge in planning
effective trials in LVV. A key factor is the
use of high-dose corticosteroids as the main
stay of treatment in LVV, and the tendency in
GCA for overtreatment with steroids owing
to concern regarding the risk of blindness.
A second critical factor is the need to define,
agree and validate outcome measures for
LVV trials. Many queries remain and these
include whether end points can be agreed
that are the same for GCA and Takayasu
arteritis, so that patients with either condi-
tion can be included in a single trial. The
role of imaging must also be determined.
Although noninvasive imaging can detect
arterial damage, its role in assessing disease
activity in the arterial wall as increased wall
thickness, oedema or wall enhancement
has yet to be established. These questions
are being addressed by OMERACT, and
OMERACT 10 has initiated an international
expert Delphi exercise, the results of which
are awaited.17
Results of trials of methotrexate therapy
in LVV have produced conflicting results.55
However, we would argue that this conflict
could reflect underpowered clinical trials,
inadequate doses of the immunosuppressive
drug and the lack of reliable outcome meas-
ures. When considering future clinical trials,
there is a strong case for a large, adequately
powered placebo-controlled trial of metho-
trexate as an adjunct to corticosteroids. This
trial should be of sufficient duration (ideally
2-year follow-up) and investigate a steroid-
sparing effect and improved maintenance of
remission in GCA and Takayasu arteritis. In
a reasonably common disease such as GCA,
and a rare disease such as Takayasu arteri-
tis that affects patients in countries where
access to biologic agents is limited, there
is a strong case for studying a fairly cheap
and widely used drug such as methotrexate.
The well-designed, large and comprehensive
GiACTA trial will hopefully set a benchmark
for the study of biologic therapies and a suc-
cessful outcome would be a huge stimulus to
this field and lead to further pharmaceutical
company interest.
Improved understanding of the patho-
genesis of GCA and the identification of a
persistent relatively corticosteroid-resistant
type 1 helper T‑cell response in the arterial
wall has helped identify novel therapeutic
targets (Figure 1).48
Consideration must
also be given to combination therapy that
is not restricted to control of inflammation;
thus, vascular dendritic cell activation, myo
fibroblast proliferation, generation of reac-
tive oxygen species and neovascularisation
of the arterial wall all contribute to patho-
genesis in LVV and should be considered in
future trials. The antiproliferative actions of
the mammalian target of rapamycin (mTOR)
antagonists sirolimus and everolimus, which
can suppress myofibroblast proliferation,
might well have a part to play, particularly
in patients developing arterial stenoses.48,49
Conclusions
In conclusion, the future of clinical trials in
vasculitis is looking brighter, due to the for-
mation of networks of individuals with the
motivation to improve the evidence base for
the management of vasculitis. A number of
new potential therapies are on the horizon.
In AAV, more evidence is required for indi-
vidualizing therapy for PR3-ANCA and
MPO-ANCA disease (or GPA and MPA),
and for therapy for EGPA, and steroid-
sparing protocols are required. Biomarkers
to identify those patients most likely to
relapse and more effective means to maintain
remission in relapsing patients are required.
In LVV, not enough data is available yet to
validate the end points and outcome meas-
ures that are in use, but that situation should
change after the current generation of
RCTs in LVV are completed. Studies of new
imaging modalities in LVV are also under-
way and these might well provide important
biomarkers for future clinical trials if they
can be validated. Large studies will always
require consortia with established leaders,
and large-scale governmental, charitable
or industry funding. However, there is still
PERSPECTIVES
© 2014 Macmillan Publishers Limited. All rights reserved
- 8. NATURE REVIEWS | RHEUMATOLOGY VOLUME 10 | AUGUST 2014 | 509
a place for experimental medicine studies
that can be performed with smaller groups
of intensively studied patients. These studies
can be followed up by larger trials in which
the protocol in use shows promise. Although
there is no doubt that biologic therapies will
have an important effect on the manage-
ment of vasculitis in the coming years, one
should bear in mind that many advances
have been achieved by simple refinements
to existing therapies, such as a reduction in
cyclophosphamide exposure in AAV.
Renal and Vascular Inflammation Section,
Department of Medicine (R.M.T., C.D.P.),
Vascular Sciences Unit, National Heart and
Lung Institute (J.C.M.), Hammersmith Hospital
Campus, Imperial College London, Du Cane
Road, London W12 0NN, UK.
Correspondence to: R.M.T.
r.tarzi@imperial.ac.uk
1. Jennette, J. C. et al. 2012 revised international
Chapel Hill consensus conference
nomenclature of vasculitides. Arthritis Rheum.
65, 1–11 (2013).
2. Hamour, S., Salama, A. D. Pusey, C. D.
Management of ANCA-associated vasculitis:
current trends and future prospects. Ther. Clin.
Risk Manag. 6, 253–264 (2010).
3. Robson, J. et al. Damage in the ANCA-
associated vasculitides: long-term data
from the European Vasculitis Study group
(EUVAS) therapeutic trials. Ann. Rheum. Dis.
http://dx.doi.org/10.1136/annrheumdis-
2013-203927.
4. Heijl, C. et al. Incidence of malignancy in
patients treated for antineutrophil cytoplasm
antibody-associated vasculitis: follow-up data
from European Vasculitis Study Group clinical
trials. Ann. Rheum. Dis. 70, 1415–1421
(2011).
5. Unizony, S. H. et al. Design of the tocilizumab in
giant cell arteritis trial. Int. J. Rheumatol. 2013,
912562 (2013).
6. US National Library of Medicine. Clinical trials.gov
[online], http://www.clinicaltrials.gov/ct2/show/
NCT01791153?term=NCT01791153rank=1
(2013).
7. Walsh, M. et al. Plasma exchange and
glucocorticoid dosing in the treatment of anti-
neutrophil cytoplasm antibody associated
vasculitis (PEXIVAS): protocol for a randomized
controlled trial. Trials 14, 73 (2013).
8. US National Library of Medicine. ClinicalTrials.gov
[online], http://www.clinicaltrials.gov/ct2/show/
NCT00987389?term=NCT00987389rank=1
(2013).
9. Berry, D. A. Bayesian clinical trials. Nat. Rev.
Drug Discov. 5, 27–36 (2006).
10. US National Library of Medicine. ClinicalTrials.gov
[online], http://www.clinicaltrials.gov/ct2/show/
NCT01363388?term=NCT01363388rank=1
(2013).
11. Basu, N. et al. EULAR points to consider in the
development of classification and diagnostic
criteria in systemic vasculitis. Ann. Rheum. Dis.
69, 1744–1750 (2010).
12. Craven, A. et al. ACR/EULAR-endorsed study to
develop Diagnostic and Classification Criteria
for Vasculitis (DCVAS). Clin. Exp. Nephrol. 17,
619–621 (2013).
13. Tervaert, J. W. et al. Association between active
Wegener’s granulomatosis and anticytoplasmic
antibodies. Arch. Intern. Med. 149, 2461–2465
(1989).
14. Seror, R. et al. Adalimumab for steroid sparing
in patients with giant-cell arteritis: results of a
multicentre randomised controlled trial. Ann.
Rheum. Dis. http://dx.doi.org/10.1136/
annrheumdis-2013-203586.
15. Berden, A. E. et al. Histopathologic classification
of ANCA-associated glomerulonephritis. J.Am.
Soc. Nephrol. 21, 1628–1636 (2010).
16. Merkel, P. A. et al. The OMERACT core set of
outcome measures for use in clinical trials of
ANCA-associated vasculitis. J. Rheumatol. 38,
1480–1486 (2011).
17. Direskeneli, H. et al. Development of outcome
measures for large-vessel vasculitis for use in
clinical trials: opportunities, challenges, and
research agenda. J. Rheumatol. 38,
1471–1479 (2011).
18. Luqmani, R. A. et al. Birmingham Vasculitis
Activity Score (BVAS) in systemic necrotizing
vasculitis. QJM 87, 671–678 (1994).
19. de Groot, K., Gross, W. L., Herlyn, K.
Reinhold-Keller, E. Development and validation
of a disease extent index for Wegener’s
granulomatosis. Clin. Nephrol. 55, 31–38
(2001).
20. Dolezalova, P. et al. Disease activity
assessment in childhood vasculitis:
development and preliminary validation of
the Paediatric Vasculitis Activity Score (PVAS).
Ann. Rheum. Dis. 72, 1628–1633 (2013).
21. Exley, A. R. et al. Development and initial
validation of the Vasculitis Damage Index for
the standardized clinical assessment of
damage in the systemic vasculitides. Arthritis
Rheum. 40, 371–380 (1997).
22. Suppiah, R. et al. Measurement of damage in
systemic vasculitis: a comparison of the
Vasculitis Damage Index with the Combined
Damage Assessment Index. Ann. Rheum. Dis.
70, 80–85 (2011).
23. Stone, J. H. et al. Rituximab versus
cyclophosphamide for ANCA-associated
vasculitis. N. Engl. J. Med. 363, 221–232
(2010).
24. Jones, R. B. et al. Rituximab versus
cyclophosphamide in ANCA-associated renal
vasculitis. N. Engl. J. Med. 363, 211–220
(2010).
25. Tarzi, R. M. Pusey, C. D. Vasculitis: Risks
and rewards of treating elderly patients with
vasculitis. Nat. Rev. Nephrol. 7, 253–255 (2011).
26. Mello, M. M. et al. Preparing for responsible
sharing of clinical trial data. N. Engl. J. Med.
369, 1651–1658 (2013).
27. Nisen, P. Rockhold, F. Access to patient-level
data from GlaxoSmithKline clinical trials.
N. Engl. J. Med. 369, 475–478 (2013).
28. Fauci, A. S., Katz, P., Haynes, B. F. Wolff, S. M.
Cyclophosphamide therapy of severe systemic
necrotizing vasculitis. N. Engl. J. Med. 301,
235–238 (1979).
29. Faurschou, M. et al. Malignancies in Wegener’s
granulomatosis: incidence and relation to
cyclophosphamide therapy in a cohort of 293
patients. J. Rheumatol. 35, 100–105 (2008).
30. Holle, J. U. et al. Improved outcome in 445
patients with Wegener’s granulomatosis in a
German vasculitis center over four decades.
Arthritis Rheum. 63, 257–266 (2011).
31. Flossmann, O. et al. Long-term patient survival
in ANCA-associated vasculitis. Ann. Rheum. Dis.
70, 488–494 (2011).
32. US National Library of Medicine. ClinicalTrials.gov
[online], http://www.clinicaltrials.gov/ct2/show/
NCT01697267?term=NCT01697267rank=1
(2012).
33. Jennette, J. C., Falk, R. J., Hu, P. Xiao, H.
Pathogenesis of antineutrophil cytoplasmic
autoantibody-associated small-vessel
vasculitis. Annu. Rev. Pathol. 8, 139–160
(2013).
34. Hogan, S. L. et al. Predictors of relapse and
treatment resistance in antineutrophil
cytoplasmic antibody-associated small-vessel
vasculitis. Ann. Intern. Med. 143, 621–631
(2005).
35. Lyons, P. A. et al. Genetically distinct subsets
within ANCA-associated vasculitis. N. Engl. J.
Med. 367, 214–223 (2012).
36. Falk, R. J. Jennette, J. C. ANCA disease:
where is this field heading? J.Am. Soc. Nephrol.
21, 745–752 (2010).
37. de Groot, K. et al. Pulse versus daily oral
cyclophosphamide for induction of remission in
antineutrophil cytoplasmic antibody-associated
vasculitis: a randomized trial. Ann. Intern. Med.
150, 670–680 (2009).
38. Harper, L. et al. Pulse versus daily oral
cyclophosphamide for induction of remission
in ANCA-associated vasculitis: long-term
follow-up. Ann. Rheum. Dis. 71, 955–960
(2012).
39. Jayne, D. R. et al. Randomized trial of plasma
exchange or high-dosage methylprednisolone
as adjunctive therapy for severe renal
vasculitis. J.Am. Soc. Nephrol. 18, 2180–2188
(2007).
40. Walsh, M. et al. Long-term follow-up of patients
with severe ANCA-associated vasculitis
comparing plasma exchange to intravenous
methylprednisolone treatment is unclear.
Kidney Int. 84, 397–402 (2013).
41. US National Library of Medicine. ClinicalTrials.gov
[online], http://www.clinicaltrials.gov/ct2/show/
NCT00128895?term=NCT00128895rank=1
(2005).
42. Little, M. A. et al. Early mortality in systemic
vasculitis: relative contribution of adverse
events and active vasculitis. Ann. Rheum. Dis.
69, 1036–1043 (2010).
43. Watts, R. A., Lane, S. E., Bentham, G.
Scott, D. G. Epidemiology of systemic
vasculitis: a ten-year study in the United
Kingdom. Arthritis Rheum. 43, 414–419
(2000).
44. Cohen, P. et al. Churg–Strauss syndrome with
poor-prognosis factors: A prospective
multicenter trial comparing glucocorticoids and
six or twelve cyclophosphamide pulses in forty-
eight patients. Arthritis Rheum. 57, 686–693
(2007).
45. Cartin-Ceba, R., Fervenza, F. C. Specks, U.
Treatment of antineutrophil cytoplasmic
antibody-associated vasculitis with rituximab.
Curr. Opin. Rheumatol. 24, 15–23 (2012).
46. Pepper, R. J. et al. Rituximab is effective in the
treatment of refractory Churg–Strauss
syndrome and is associated with diminished
T‑cell interleukin‑5 production. Rheumatology
(Oxford) 47, 1104–1105 (2008).
47. US National Library of Medicine. ClinicalTrials.gov
[online], http://www.clinicaltrials.gov/ct2/show/
NCT02020889?term=NCT02020889rank=1
(2013).
48. Weyand, C. M., Liao, Y. J. Goronzy, J. J.
The immunopathology of giant cell arteritis:
diagnostic and therapeutic implications.
J. Neuroophthalmol. 32, 259–265 (2012).
49. Mason, J. C. Takayasu arteritis—advances
in diagnosis and management. Nat. Rev.
Rheumatol. 6, 406–415 (2010).
50. US National Library of Medicine. ClinicalTrials.gov
[online]. http://www.clinicaltrials.gov/ct2/show/
NCT00974883?term=tabulrank=1 (2009).
FOCUS ON VASCULITIS
© 2014 Macmillan Publishers Limited. All rights reserved
- 9. 510 | AUGUST 2014 | VOLUME 10 www.nature.com/nrrheum
51. Diamantopoulos, A. P. et al. Diagnostic value of
color Doppler ultrasonography of temporal
arteries and large vessels in giant cell arteritis:
a consecutive case series. Arthritis Care Res.
(Hoboken) 66, 113–119 (2014).
52. Misra, R. et al. Development and initial
validation of the Indian Takayasu Clinical
Activity Score (ITAS2010). Rheumatology
(Oxford) 52, 1795–1801 (2013).
53. Hoffman, G. S. et al. Infliximab for maintenance
of glucocorticosteroid-induced remission of
giant cell arteritis: a randomized trial. Ann.
Intern. Med. 146, 621–630 (2007).
54. Martinez-Taboada, V. M. et al. A double-blind
placebo controlled trial of etanercept in
patients with giant cell arteritis and
corticosteroid side effects. Ann. Rheum. Dis.
67, 625–630 (2008).
55. Mahr, A. D. et al. Adjunctive methotrexate for
treatment of giant cell arteritis: an individual
patient data meta-analysis. Arthritis Rheum.
56, 2789–2797 (2007).
56. Hoffman, G. S. et al. A multicenter, randomized,
double-blind, placebo-controlled trial of
adjuvant methotrexate treatment for giant cell
arteritis. Arthritis Rheum. 46, 1309–1318
(2002).
57. Jover, J. A. et al. Combined treatment of giant-
cell arteritis with methotrexate and prednisone.
A randomized, double-blind, placebo-controlled
trial. Ann. Intern. Med. 134, 106–114 (2001).
58. Spiera, R. F. et al. A prospective, double-blind,
randomized, placebo controlled trial of
methotrexate in the treatment of giant cell
arteritis (GCA). Clin. Exp. Rheumatol. 19,
495–501 (2001).
59. Dasgupta, B. et al. BSR and BHPR guidelines
for the management of giant cell arteritis.
Rheumatology (Oxford) 49, 1594–1597
(2010).
60. US National Library of Medicine. ClinicalTrials.gov
[online], http://www.clinicaltrials.gov/ct2/show/
NCT00556439?term=NCT00556439rank=1
(2013).
61. Comarmond, C. et al. Anti TNF-α in refractory
Takayasu’s arteritis: cases series and review of
the literature. Autoimmun. Rev. 11, 678–684
(2012).
62. Abisror, N. et al. Tocilizumab in refractory
Takayasu arteritis: a case series and updated
literature review. Autoimmun. Rev. 12,
1143–1149 (2013).
63. Youngstein, T. et al. Serial analysis of clinical
and imaging indices reveals prolonged efficacy
of TNF-α and IL‑6 receptor targeted therapies in
refractory Takayasu arteritis. Clin. Exp.
Rheumatol. CER6558 (2013).
64. De Groot, K. et al. Randomized trial of
cyclophosphamide versus methotrexate for
induction of remission in early systemic
antineutrophil cytoplasmic antibody-associated
vasculitis. Arthritis Rheum. 52, 2461–2469
(2005).
65. Faurschou, M. et al. Brief report: long-term
outcome of a randomized clinical trial comparing
methotrexate to cyclophosphamide for remission
induction in early systemic antineutrophil
cytoplasmic antibody-associated vasculitis.
Arthritis Rheum. 64, 3472–3477 (2012).
66. Specks, U. et al. Efficacy of remission-induction
regimens for ANCA-associated vasculitis.
N. Engl. J. Med. 369, 417–427 (2013).
67. Jayne, D. et al. A randomized trial of
maintenance therapy for vasculitis associated
with antineutrophil cytoplasmic autoantibodies.
N. Engl. J. Med. 349, 36–44 (2003).
68. Hiemstra, T. F. et al. Mycophenolate mofetil vs
azathioprine for remission maintenance in
antineutrophil cytoplasmic antibody-associated
vasculitis: a randomized controlled trial. JAMA
304, 2381–2388 (2010).
69. Pagnoux, C. et al. Azathioprine or methotrexate
maintenance for ANCA-associated vasculitis.
N. Engl. J. Med. 359, 2790–2803 (2008).
70. The Wegener’s granulomatosis Etanercept
Trial (WGET) Research Group. Etanercept plus
standard therapy for Wegener’s granulomatosis.
N. Engl. J. Med. 352, 351–361 (2005).
71. Metzler, C. et al. Elevated relapse rate under
oral methotrexate versus leflunomide for
maintenance of remission in Wegener’s
granulomatosis. Rheumatology (Oxford) 46,
1087–1091 (2007).
Acknowledgements
R.M.T. gratefully acknowledges salary support from
an Arthritis Research UK Clinician Scientist
Fellowship. The authors acknowledge support from
the Imperial NIHR Biomedical Research Centre.
Author contributions
R.M.T. and J.C.M. researched data for and wrote
the article. All authors made equal contributions to
discussion of content and reviewing/editing the
manuscript before submission.
Supplementary information is linked to the online
version of the paper at www.nature.com/nrrheum.
PERSPECTIVES
© 2014 Macmillan Publishers Limited. All rights reserved