4th Annual Early Age Onset Colorectal Cancer Summit: Transforming Family Health History Ascertainment and Colorectal Cancer Preventive Services in Primary Care An Update from the NCCRT Family History Early Age Onset Task Group.
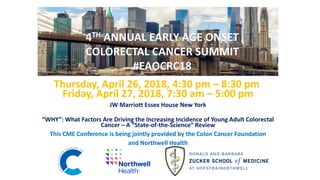
- 1. Thursday, April 26, 2018, 4:30 pm – 8:30 pm Friday, April 27, 2018, 7:30 am – 5:00 pm JW Marriott Essex House New York “WHY”: What Factors Are Driving the Increasing Incidence of Young Adult Colorectal Cancer – A “State-of-the-Science” Review This CME Conference is being jointly provided by the Colon Cancer Foundation and Northwell Health 4TH ANNUAL EARLY AGE ONSET COLORECTAL CANCER SUMMIT #EAOCRC18
- 2. SPECIAL SYMPOSIUM Transforming Family Health History Ascertainment and Colorectal Cancer Preventive Services in Primary Care An Update from the NCCRT Family History Early Age Onset Task Group Thursday April 26, 2018 4:30 pm – 8:30 PM
- 3. EDUCATIONAL OBJECTIVES • Review the mission, goals and accomplishments of the National Colorectal Cancer Roundtable (NCCRT) Family History and Early Onset Task Group. • Learn about the importance of Family Health History for colorectal cancer, including advanced adenomas, and its importance in preventing colorectal cancer. This will include current challenges and opportunities surrounding ascertainment and documentation of actionable family health history information in primary care. • Experience a “First Look” at the NCCRT Risk Assessment & Screening Toolkit for facilitating the identification and management of patients at risk of familial, hereditary and early onset colorectal cancer. This will include a summary of our current state of knowledge on the optimal standards for collecting a family history as well as care and support for the young adult colorectal cancer patient. The Toolkit will include examples of best practices as well as tools and resources available to facilitate efforts to meet these standards. • Review the leadership roles, challenges, and opportunities for primary care in implementing system-based strategies aimed at promoting appropriate risk assessment and screening of individuals at familial risk of CRC, as well as early diagnostic evaluation of individuals with signs or symptoms of CRC, regardless of age. ORGANIZER AND HOST Thomas K. Weber MD FACS Director of Surgical Oncology; Northwest Region at Northwell Health President and Founder, Colon Cancer Foundation CO-CHAIRS NCCRT FAMILY HISTORY EARLY ONSET CRC TASK GROUP Paul C. Schroy III MD MPH Professor of Medicine Boston University School of Medicine Director of Clinical Research GI Section, Boston Medical Center Dr. Dennis J. Ahnen MD AGAF FACG Professor of Medicine University of Colorado School of Medicine, Genetics Clinic, Gastroenterology of the Rockies
- 4. PRESENTATIONS OPENING REMARKS Thomas K. Weber, MD, FACS, Director of Surgical Oncology; Northwest Region at Northwell Health; President and Founder, Colon Cancer Foundation OVERVIEW AND INTRODUCTION TO THE NATIONAL COLORECTAL CANCER ROUNDTABLE (NCCRT) AND THE FAMILY HISTORY EARLY AGE ONSET COLORECTAL CANCER TASK GROUP Dennis Ahnen, MD, AGAF, FACG, University of Colorado School of Medicine Paul Schroy III, MD, MPH, Boston University School of Medicine FRAMING THE FAMILIAL/HEREDITARY COMPONENT AND OTHER OPPORTUNITIES TO IDENTIFY THOSE MOST AT RISK: • LYNCH, FAP, MYH • FIRST DEGREE RELATIVE WITH COLORECTAL CANCER • FIRST DEGREE RELATIVE WITH COLONIC ADVANCED ADENOMA Swati G. Patel, MD, MS, University of Colorado Anschutz Medical Center Heather Hampel, MS, LGC, The Ohio State University Comprehensive Cancer Center Christine Louise S. Molmenti, MPH, PhD, Feinstein Institute for Medical Research/Northwell; Donald and Barbara Zucker School of Medicine at Hofstra/Northwell
- 5. PRESENTATIONS FIRST LOOK – THE NCCRT RISK ASSESSMENT AND SCREENING TOOLKIT TO DETECT FAMILIAL, HEREDITARY, AND EARLY ONSET COLORECTAL CANCER: Emily Edelman, MS, CGC, The Jackson Laboratory Shelly Yu, MPH, American Cancer Society Cancer Action Network, Inc. Summary of current practices and known barriers related to the identification, screening and management of patients at increased CRC risk; Opportunities with regard to Electronic Health Record Systems; Family history ascertainment and risk assessment tools currently on the market; Overview of the Toolkit goals, core objectives, conclusions and limitations; Suggestions for implementation and dissemination; Plans for future follow up and programming.
- 6. PRESENTATIONS Primary Care Leadership in Colorectal Cancer Risk Assessment: Family Medicine, Internal Medicine, Obstetrics and Gynecology - Faculty Includes: Dennis Ahnen, MD, AGAF, FACG, University of Colorado School of Medicine Durado Brooks, MD, MPH, American Cancer Society Maureen Killackey, MD, New York Presbyterian/Herbert Irving Comprehensive Cancer Center Jennifer Reich, MD, Orange Regional Medical Center and Valley Hospital Randa Sifri, MD, Thomas Jefferson University
- 7. National Colorectal Cancer Roundtable and Family History Early Age Onset CRC Task Group Who Are We?
- 8. NCCRT is a national coalition of public, private, and voluntary organizations whose mission is to advance colorectal cancer control efforts by improving communication, coordination, and collaboration among health agencies, medical-professional organizations, and the public. Co-Founded by ACS and CDC in 1997 Collaborative partnership of over 100 member organizations Includes many nationally known experts, thought leaders, and decision makers on colorectal cancer Work is conducted throughout the year through various Task Groups and Special Topic Meetings National Colorectal Cancer Roundtable (NCCRT)
- 9. Task Groups Professional Education and Practice Community Health Centers Public Awareness and Social Media Evaluation and Measurement Policy Action Quality Assurance Family History and Early Onset CRC
- 10. Tools, Resources and Publications 10
- 11. 80% by 2018 80% by 2018 is a movement in which hundreds of organizations have committed to eliminating colorectal cancer as a major public health problem and are working toward the shared goal of reaching 80% screened for colorectal cancer by 2018. More than1500 organizations have signed the pledge! nccrt.org/tools/80-percent-by-2018/80-percent-by-2018-pledge/
- 12. Family History and Early Age Onset (EAO) CRC Task Group
- 13. Founded in 2012 Expanded to include Early Onset CRC in 2016 The charge is to identify key issues and areas of need around familial, inherited and early onset colorectal cancer for the purpose of identifying opportunities for the Roundtable to be a catalyst for change. Family History Task Group
- 14. • Help clinicians develop a system-based approach to the identification and management of patients at familial risk, as well as the recommendation for early diagnostic evaluation of those presenting with signs or symptoms of CRC at any age. • Improve EHRs to help facilitate needed screening and/or counseling recommendations for patients with a family history. • Increase clinician-patient and intra-family communication about familial/heritable risk. • Improve “on time” screening for the 50 to 55 population, according to recommended guidelines. • Address the increase in CRC in young adults through strategic planning and interactions with key stakeholders and thought leaders. Task Group Themes
- 15. Family History and Early Age Onset CRC Task Group Accomplishments
- 16. Hosted FH Symposium on Sept 23, 2014 • 34 attendees, including many renown experts in the field • Goals: Review state-of-the-science: risk estimate, screening guidelines, screening rates, barriers, interventions Identify research priorities Determine critical next steps to increase screening rates in high-risk individuals • Key take-home messages Need to enhance the capability of EHR systems for collecting FH data in standardized formats and linking them with clinical decision making; Need for provider education and risk assessment tools to facilitate identification and appropriate management of patients at increased/high risk; Outreach to survivors provides a key yet underutilized link to high risk families. Needs include: o Tools to help survivors communicate risk to their families. o Guidelines for educating patients about talking to their doctors regarding CRC.
- 18. State-of- Science Paper: Key Priorities • Improve how we collect and utilize cancer FH information. • Establish consensus across organizations for CRC screening guidelines by FH status. • Enhance provider/patient knowledge of guidelines and communication about CRC risk. • Encourage cancer survivors to promote screening within their families, and partner with existing CRC screening programs to expand reach to high-risk groups.
- 19. Improve Collection/Utilization of FH Information Electronic Health Record (EHR)
- 20. GI Brief 5 key recommendations: • Focused FH for all patients annually • Keep abreast of guidelines • Establish a referral process • ID high-risk patients in Endoscopy Unit • Develop/use tools to communicate with family Available at nccrt.org/80by2018 Provider Education
- 21. GI Brief/Dissemination • Released during the Dec. 8, 2016 webinar on familial risk and CRC: http://nccrt.org/resource/familial-risk-webinar/ • Sent email notification to NCCRT members and 80% pledged partners • Promoted on NCCRT’s Facebook and Twitter social media channel • Issued call to action to GI society representatives and communications leads to promote Provider Education
- 22. Toolkit • Jackson Lab commissioned to develop practice transformation clinician’s toolkit on family history and early onset CRC. • Goals: To bridge the existing knowledge gap and to provide a step-by-step, detailed tool for practices that are dedicated to improving their processes related to the collection of family history and acting on that information according to recommended guidelines. Provide guidance on the appropriate diagnostic evaluation of patients with “alarm” signs and symptoms of CRC, regardless of age. Provider Education
- 23. Toolkit Specific Objectives: • Conduct a multi-faceted needs assessment to discover best practices in CRC screening of at-risk populations and to identify key drivers influencing successful CRC screening programs • Develop a toolkit for PCPs to facilitate practical implementation of appropriate risk assessment, screening, and communication practices for early detection of CRC Provider Education
- 25. 2017 Early Age Onset Colorectal Cancer Summit: “What we know, what we don’t know, and what we need to know” •The National Colorectal Cancer Roundtable, the American Cancer Society, and the Colon Cancer Challenge Foundation convened a strategic meeting on December 6, 2017, with a small group of key thought leaders and national stakeholders to focus on the concerning trend of early age onset colorectal cancer. •Purpose: To assess how the NCCRT and its partners, including clinical practitioners, researchers, and advocacy organizations, can most effectively align to address the issue in both the short and long term. Early Onset CRC
- 26. Agenda and Discussions •Panel 1: Emerging Trends and Research: A review of what we know, what we don’t know, and what we need to know. •Panel 2: Exploring key questions that need further scientific research and explanation This discussion asked panelists to pose key questions from their perspective that need to be answered and studies that need to be conducted in critical research areas. Focus areas included epidemiology, molecular biology, and genetics. •Review and Discussion: Risk Assessment and Screening Toolkit to Detect Familial, Hereditary and Early Onset Colorectal Cancer Early Onset CRC
- 27. Small Group Discussions “Acting Now: What important steps need to happen if we are to address knowledge gaps” •3 Discussion Groups What are the key research questions that need to be addressed in this area and how can we stimulate needed research? What do frontline providers need most need if they are to play a more effective role in diagnosing CRC at the earliest stage? What is the role of national organizations, such as NCI, CDC, ACS and the NCCRT, in stimulating work around the early age onset issue with front- line providers? Early Onset CRC
- 28. Meeting Themes • Defining roles for major stakeholders National agencies: coming together and providing guidance for research on the issue. Front-line providers: Engaging them and better understand how to provide assistance. NCCRT: Provide a platform to gather partners around the issue. Healthcare Systems: Improve organization and engagement in research and implementation. • Improving Practice: Development, accessibility and validation of tools improving practice. Early Onset CRC
- 29. Meeting Themes (cont) • Modeling: Inform the CRC screening microsimulation models by better defining the adenoma prevalence & dwell time in the < 40 - 50 year old age group. • Emphasis on communication: Continue to promote awareness around family health communication, with particular interest towards advanced adenomas; Changing the narrative to incorporate “On Time Screening” messaging • Insuring universal MSI testing • Urgent need for additional research Early Onset CRC
- 30. Post-Meeting Progress • Two meeting reports are in development A detailed meeting recap and recording of conversations. An academic manuscript noting key themes, areas of focus, and pertinent research questions explored. • Keeping the conversation moving forward: Colon Cancer Challenge Foundation’s Summit Early Onset CRC
- 31. Improve Collection/Utilization of FH Information EHR EHR Meeting (9/29/15) Delphi Survey ACS CAN
- 32. Hosted EHR Meeting (9/29/15) Objectives: Develop consensus statement, core components and outline NCCRT Strategy on improving FH collection in EMRs Issues from Family History perspective: – EMR data is collected in a variable manner • What is goal of FH component of EMR? • What are the minimal data elements? • How should they be collected? – No link between family history data in EMR and clinical decisions • What types of linkage? • Potentially work with vendors Improve Collection/Utilization of FH Information
- 33. Delphi Survey Goal: •Establish a standardized, core set of data items for collecting cancer family history directly into EHRs, or integrating these into EHRs from family history tools. Progress: • Transition from “Broad Consensus” to “Expert Consensus” • Completed first iteration of the survey. • Received comments on low and high level agreement questions, currently working on those with mid level agreement Improve Collection/Utilization of FH Information
- 34. Delphi Survey Improve Collection/Utilization of FH Information • Consensus items thus far (>80%) – Goal- ID patients who should be referred for further risk assessment and those at higher than average risk and need more intense screening – Data elements- FDRs and SDRs, age of cancer dx, all cancer types that would change screening, entered as discrete elements in searchable fields, importable from FH tool and patient portal, updated whenever new information becomes available
- 35. Delphi Survey Improve Collection/Utilization of FH Information – Links to Decision Making- capacity to alert increased risk of hereditary cancer syndrome or elevated cancer risk or need for different screening, provide links to current screening guidelines based on FH and generate best practice alerts for cancer screening for high risk pts – Development Process- Elements of FH section should be guided by national standards, standardized across EHRs, incorporated centrally by EHR vendors and updated by vendors as recommendations change – Incentives- Completing/Maintaining FH section and referral of appropriate patients for genetic counseling/testing should be expected as part of high quality care
- 36. Improve Collection/Utilization of FH Information • ACS CAN EHR Workgroup- Shelly Yu Recommendations #1: Enable the systematic, structured, and easy collection of critical data elements to inform cancer risk assessment, prevention and screening #2: Support cancer screenings by enabling providers to identify, order, track, and document screenings #3: Enable cancer risk assessment by appropriately flagging patients for genetic counseling, testing, and/or screening, and integrating with risk assessment tools
- 37. Family History Task Group Next Steps
- 38. • Finalize, disseminate and validate the Clinicians Family History EAO Toolkit • Complete the Delphi Survey, analyze the data, share results with the NCCRT and ACS CAN and submit for publication • Identify strategies for optimizing communication about advanced adenomas • Work with NCCRT to change narrative regarding “on-time screening” •Ask NCCRT to convene and facilitate a meeting of leaders of Primary Care Organizations to discuss EAO CRC. Next Steps
- 40. The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute Framing the Familial/Hereditary Component of Colorectal Cancer & Other Opportunities to Identify those Most At Risk Heather Hampel, MS, LGC Associate Director, Division of Human Genetics Professor, Department of Internal Medicine Twitter: @HHampel1
- 41. Nearly Half of Early-Onset CRC is Hereditary/Familial: aka Potentially Preventable
- 42. 42 The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute Who is at high risk for cancer? Family History is the key…
- 43. Family History An important first step in risk assessment for genetic diseases and other hereditary health conditions Americans know that family history is important to health. A recent survey found that 96 percent of Americans believe that knowing their family history is important. Yet, the same survey found that only one-third of Americans have ever tried to gather and write down their family's health history.
- 45. Strong family history of cancer Need referral for genetic counseling & consideration of genetic testing Need intensive cancer surveillance Depends on the syndrome but often includes colonoscopy every 1-2 years starting in the teens-20s The first degree relatives of a person with a hereditary cancer predisposition syndrome have a 50% chance that they have inherited it Cancer risks vary but range from 20-100% High Risk Families
- 46. Cancer in 2 or more close relatives (on same side of family) Multiple generations affected Early age at diagnosis Rare cancers (sebaceous skin cancer) Multiple primary tumors (colon and uterus; more than one colon cancer) Multiple colon polyps (>10) Patients with certain pathology findings Abnormal IHC or MSI+ testing High Risk Clues:
- 47. Over 1.2 million individuals in the United States have Lynch syndrome Inherited condition that causes high risks for colorectal cancer, endometrial cancer, and other cancers Preventable cancers with early and more frequent screening 95% of affected individuals do not know they have Lynch syndrome Lynch Syndrome
- 49. Familial Adenomatous Polyposis (FAP) o > 100 adenomatous polyps throughout colon o Increased risks for colorectal, duodenal, thyroid cancers, medulloblastoma, and hepatoblastoma o Gene: APC (30% of mutations are de novo) Attenuated FAP o 20-100 adenomas o Gene: APC (mutations in specific locations lead to milder phenotype) Adenomatous Polyposis Syndromes MUTYH-Associated Polyposis (MAP) o 20-100s of adenomatous polyps o Overlap with FAP and Lynch syndrome o Gene: MUTYH (recessive with 1/50 carrier frequency) Polymerase proofreading-associated polyposis (PPAP) o Increased risk of adenomatous colon polyps, colon cancer, uterine cancer, and possibly other cancers o Newer syndrome, still being defined o Genes: POLD1, POLE
- 50. Peutz-Jeghers syndrome o Peutz-Jeghers polyps primarily in the small intestine but can be throughout GI tract o Increased risk for GI cancers and multiple other cancers (breast, SCTAT of the ovaries and testicles, pancreatic) o Gene: STK11 Hamartomatous Polyposis Syndromes Juvenile polyposis syndrome o Juvenile polyps throughout GI tract, increased risk for GI cancers o > 5 JP is diagnostic criteria o Genes: BMPR1A, SMAD4 Serrated polyposis syndrome o > 20 serrated/hyperplastic polyps throughout the colon o Increased risk for colon cancer o Gene: Not known GI = gastrointestinal; JP = juvenile polyposis; SCTAT = sex cord tumor with annular tubules.
- 51. Hereditary mixed polyposis syndrome o Syndrome mostly seen in individuals of Ashkenazi Jewish ancestry o Adenomatous, hyperplastic, other type of polyps through GI tract o Gene: SCG5/GREM1 Cowden syndrome o Multiple different types of polyps – ganglioneuromas especially suspicious o Increased risk for breast, thyroid, endometrial, and colon cancers o Gene: PTEN Mixed Polyposis Syndromes
- 52. 1-2 cases of a cancer in the family Do not need referral for genetic counseling Do need increased cancer surveillance Generally the first degree relatives of a person with a cancer are about twice as likely to develop that same cancer than someone without that family history (10% lifetime risk) Moderate Risk Families
- 53. Familial Colorectal Cancer Risks Taylor, DP, Gastroenterology 2010;138:877-886.
- 54. >1 FDR dx at any age Colonoscopy every 5-10 years beginning at age 40 (or 10 years before earliest dx of CRC) >1 SDR diagnosed <50 Colonoscopy every 5-10 years beginning at age 50 FDR with advanced adenoma(s) Colonoscopy every 5-10 years beginning at age 40 or age of onset of adenoma in relative Otherwise follow Average Risk recommendations Colonoscopy every 10 years beginning at age 50 Familial Colorectal Cancer Screening Recommendations
- 55. 55
- 56. Overview of Opportunities for Improving Capture of Family History through the EHR Shelly Yu, MPH Senior Legislative and Policy Analyst – Emerging Science ACS CAN Shelly.yu@cancer.org
- 58. Family History and Advanced Adenoma Initiatives Christine L.S. Molmenti, PhD, MPH Assistant Professor Feinstein Institute for Medical Research Donald and Barbara Zucker School of Medicine at Hofstra/Northwell Department of Occupational Medicine, Epidemiology, and Prevention Center for Health Innovations and Outcomes Research April 26, 2018
- 59. Overview 1. Background and significance 1. Study designs and initiatives • Advanced adenoma prevalence among early age onset colorectal cancer • Integrated post-colonoscopy communication system (iColon) • NCCRT Advanced Adenoma Working Group 2. NCCRT Advanced Adenoma Working Group
- 60. Prime target for prevention Fearon and Vogelstein, Cell, 61, 759-767, 1990 Terzic et al, Gastroenterology 138(6), 2101-2114 2010 Normal Epithelium Metastatic Cancer Dysplastic lesion Early Adenoma Late Adenoma Cancer Cytokines, DNA repair genes, K-ras, P53, COX-2 overexpression
- 61. Advanced adenoma (AA) Defined as: ≥1 cm and/or villous/tubulovillous features or high-grade dysplasia Associated with: Increased risk of adenoma recurrence Increased risk of colorectal cancer Strum WB, NEJM 374(11); 2016
- 62. Strum WB, NEJM 374(11); 2016 Advanced adenomas ≤ 5mm adenomas • 45-71% of adenomas • 7-16% advanced features • 0.05% malignant (4mm) 6-9 mm adenomas • 21-23% of adenomas • 10-34% advanced features • 0.2% malignant (8mm) (20 mm) ≥ 10 mm adenomas • 8-22% of adenomas • All advanced based on size • 37-54% advanced features • 3.2-11% malignant
- 63. Increased CRC risk among FDRs of patients with advanced adenomas • 2.27 to 4.36 fold increase in odds of CRC and large AA among those with FDRs diagnosed with adenomas • 6-fold increased odds of being diagnosed with an AA among FDRs of individuals with >1 AA • FDRs of AA patients have significantly higher risk of developing colorectal cancer Meta-analysis of 9 studies estimated RR of colorectal cancer in FDRs of patients with adenomas as 1.99 FDR = First Degree Relative (Parent, Sibling, Child)
- 64. Guidelines 1. United States Multi-Society Task Force (USMSTF) 2. American Cancer Society (ACS) Advanced adenoma in 2 FDRs (any age) or AA in 1 FDR < 60 y Colonoscopy every 5 years beginning 10 years before the age at diagnosis or age 40 y, whichever is earlier. Advanced adenoma in 1 FDR at age ≥60 y Begin screening at 40. Options for screening are the same as those for average-risk persons. 3. National Comprehensive Cancer Network (NCCN) Advanced adenoma(s) in an FDR regardless of age Colonoscopy beginning at age 40 y or at age of onset of adenoma in relative, whichever is first
- 65. 88% with adenoma diagnosis do not know they are at higher risk Among those with Any Adenoma (n=56) More likely 7 (12.5%) Less likely 18 (32.1%) About as likely 16 (28.6%) Don't know 15 (26.8%) Compared to the average person your age, your chance of developing colorectal cancer is…… Among those with ≥1cm, ≥3, or villous histology (n=30) More likely 4 (13.8%) Less likely 9 (31.0%) About as likely 8 (27.6%) Don't know 8 (27.6%) Molmenti C, 2018, in preparation Columbia University CRC Risk Perception and Risk Awareness Study 88% 86%
- 66. Initiative #1. Prevalence of advanced adenomas among early age onset colorectal cancer cases • In collaboration with the Ohio Colorectal Cancer Prevention Initiative (OCCPI): Universal Screening for Lynch Syndrome (USLS)
- 67. Unknown what percentage of EAO CRC is due to family history of advanced adenoma Ohio Colorectal Cancer Prevention Initiative (OCCPI): Universal Screening for Lynch Syndrome (USLS) EAO CRC 67 56% Sporadic 16% Hereditary 14% Family history CRC ≥14%?? Family History of AA
- 68. Unknown what percentage of EAO CRC is due to family history of advanced adenoma Ohio Colorectal Cancer Prevention Initiative (OCCPI): Universal Screening for Lynch Syndrome (USLS) EAO CRC 68 50% Sporadic 16% Hereditary 14% Family history CRC 20% Family History of AA
- 69. Unknown what percentage of EAO CRC is due to family history of advanced adenoma Ohio Colorectal Cancer Prevention Initiative (OCCPI): Universal Screening for Lynch Syndrome (USLS) 56% Sporadic 14% Family history of CRC XX% Family History of AA 40% Sporadic 16% Hereditary 14% Family history CRC 30% Family History of AA
- 70. Priority area in CRC research Understand advanced adenoma prevalence among EAO CRC is a priority area and a critical step in decreasing incidence and mortality of EAO CRC Innovation: • Determine the contribution of component of familial risk that has not been measured • The first study (to our knowledge) to investigate the prevalence of AA among a cohort of pathologically confirmed EAO CRC patients 70
- 71. EAO CRC cases, n=507 • EAO cases recruited between 1/1/2013 and 12/31/2016) Diagnosed with a primary invasive colorectal adenocarcinoma (all stages) <50 years of age Not identified as having a cancer susceptibility gene or having a family history of colorectal cancer • Anticipate 4 first degree relatives per EAO case N=~2000 FDRs to contact
- 72. Proband contacted and consented Letter/email Proband provides contact information for FDR(s) Study team contact FDRs* Consent and medical release form signed Study staff identifies documentation of FDRs colonoscopy and pathology reports Study flow *FDRs who have not undergone colonoscopy will be encouraged to do so as soon as possible. For those who decline, FIT will be offered
- 73. Outcomes 1) Prevalence of AA among FDRs of EAO CRC patients who do not have a hereditary syndrome or a first degree relative with colorectal cancer. 2) Proportion (%) of EAO CRC patients who would have been recommended to start colonoscopy PRIOR to the age at which they developed their colorectal cancer based on the FDR with an advanced adenoma. 3) Proportion (%) of patients that were diagnosed with a EAO CRC that could have been realistically prevented or detected early.
- 74. Initiative #2. Integrated colonoscopy communication system (iCOLON) - NCI K08 grant submission Month Day, 74
- 75. Improve post-colonoscopy communication Population Adenoma patients, primary care and GI physicians Goals 1. Close “open communication loops” 2. Engage patients and families after adenoma diagnosis 3. Address surveillance colonoscopy underutilization Design Mixed-methods approach 75
- 76. Preliminary data indicates: 1. Communication between the gastroenterologist and the referring physician often lack contextual information such as final pathology results 2. Recommended follow up is not consistently documented. 3. Post-polypectomy patients have low awareness of their risk for colorectal cancer and surveillance recommendations. 4. No efficient system in place for communicating colonoscopy results.
- 77. Research questions: 1) Will improving understanding of colonoscopy results among patients with advanced adenomas impact conversation with FDRs about early screening? 2) Is it possible to create a “universal colonoscopy report” that can be shared among the gastroenterologist, patient, and primary care? 3) Can we provide links to family members to impact early screening adherence?
- 78. Survey content and outcomes* . Primary care and GI physicians will be identified and recruited upon patient nd adenoma diagnosis. y criteria. and female rs of age, lonoscopy at ithin the last ma removed, ne. Patients ory of CRC, hereditary e with luded. erologists will be Specific rvey will nowledge of their colonoscopy results, their perceived risk of colorectal cancer, Table 5. Aim 3 primary outcomes Survey Content Outcome(s) Patient What were the results of your colonoscopy? Compared to the average person, do you think you are more likely/less likely//about as likely to get CRC? Do you know if/when follow up colonoscopy should be? Risk perception Knowledge (of results and surveillance interval) Primary Care Do you know the surveillance interval that was recommended by the GI? Knowledge of GI recommended surveillance interval GI How often do you communicate risk status to your patients? How confident are you in the educational material you provided regarding their results and risk? Frequency of communicating risk. Self efficacy of communicating risk and providing appropriate patient education *Add family history questions and survey links to family members
- 79. Allscripts •Primary insurance •Medical history •Laboratory results •Lipid profile •Metabolic panel ProVationMD Endoscopy Report •Zip code •Date of birth •Age •Gender •Indications •Quality of bowel preparation •Findings •Adenoma size •Number of adenomas removed •Biopsies (yes/no) •Impression •Recommendation •Procedure code •Diagnosis code Sunrise •Height •Weight •BMI •Medications •Alcohol •Tobacco, •Language •Colonoscopy withdrawal time •Date and time of procedure •Performing physician/fellow •Cecal intubation •Use of anesthesia vs. conscious sedation Cerner Northwell Health Data Extraction Colonoscopy Registry (N=21,000) • Histology • Location of polyps • Colorectal adenomas ICD- 9/10 codes o 211.3 Colon adenoma o 211.4 Rectal adenoma • CPT codes o 43580, 45385, 45385 (screening for colorectal neoplasm)
- 80. National Colorectal Cancer Roundtable Advanced Adenoma Working Group - Established December 2018 80Month Day,
- 81. Mission • To understand the role of advanced adenoma on EAO CRC • To develop novel tools and resources to improve advanced adenoma knowledge and awareness among patients and physicians • To impact compliance with surveillance colonoscopy uptake among adenoma patients and screening uptake among FDRs of advanced adenoma patients 81
- 82. Summary and Next Steps 1. Know your family history of CRC and adenomas, particularly advanced adenomas 2. Research initiatives are needed to fully explore: • Impact of advanced adenomas on EAO CRC • How to reach family members of individuals diagnosed with advanced adenomas Month Day, 82
- 83. Acknowledgements Columbia University Alfred Neugut Heather Greenlee Jeanine Genkinger Grace Hillyer Benjamin Lebwohl Richard RosenbergCleveland Clinic Carol Burke Hennie Hasson University of Arizona Elizabeth Jacobs David S. Alberts Richard H. Carmona Robin Harris Denise Roe Cynthia Thomson The Ohio State University Heather Hampel Mark Arnold Bruce Casto Steven Clinton Northwestern University Elizabeth Hibler University of Colorado Dennis Ahnen Jennifer Kolb Harvard University Stephanie Smith-Warner Fred Tabung Northwell Health Jacqueline Moline Gloria Ho Tom Weber Tom McGinn Michael Diefenbach Renee Pekmezaris Joseph Conigliaro John Chelico Martin Lesser Rehana Rasul Samantha Schneider Francine Smith Maurice Cerulli Larry Miller Montana State University Gary D. Stoner
- 85. Outcomes 3. Proportion (%) of EAO patients that were diagnosed with a EAO CRC that could have been realistically prevented or detected early. The numerator for this proportion will include the number of EAO cases for which the tumor stage and timing of the screening interval (based upon the FDRs adenoma diagnosis and a priori categories* determined by the investigators) intersect in such a way that that it would have been reasonably possible to detect their EAO cancer early or prevent it altogether. *Category examples (will provide gender specific analyses in the study): Tumor stage 0-1 and screening recommended ≥5 yrs prior = yes reasonable chance of prevention. Tumor stage 1-2 and screening recommended ≤ 5 yrs prior = early detection more reasonable than prevention. Tumor stage 3-4 and screening recommended within one year prior = no, not reasonably prevented but potentially detected at an earlier stage. Tumor stage 3-4 and screening recommended ≥5 years prior = prevention and early detection is reasonable.
- 86. EHR Adoption, Functionality Has Increased 1.) 2008 numbers refer to adoption of basic EHRs, as defined by ONC (e.g., any EHR with capabilities in areas such as: patient demographics, physician notes, nursing assessments, patient problem lists, electronic lists of medications taken by patients. “An Electronic Health Record (EHR) is an electronic version of a patient’s medical history, that is maintained by the provider over time, and may include all the key administrative clinical data relevant to that person’s care under a particular provider…The EHR automates access to information and has the potential to streamline the clinician’s workflow. The EHR also has the ability to support other care-related activities directly or indirectly through various interfaces, including evidence-based decision support, quality management, and outcomes reporting.” - Centers for Medicare & Medicaid Services 17% 78% 9% 96% 2008 2015 Physicians Hospitals Post HITECH – Adoption of certified EHRs Pre HITECH – Adoption of basic EHRs EHR Adoption1 Among Physicians and Hospitals
- 87. Incentives Not Aligned EHR Incentive Programs (EH and/or EP) Stage 1 Stage 2 Family health history included as a menu objective for EPs and EHs; only requires one structured data entry for one first-degree relative Modified Stage 2 Stage 3 c Incorporation of Family History Requirements in the EHR Incentive Programs and CEHRT Certified Electronic Health Record Technology (CEHRT) 2014 Edition Requires EHRs to, at a minimum, be capable of recording information about a patient’s first degree relative using either SNOMED CT or the HL7 Pedigree standard; additionally EHRs must permit a user to change and access the information 2015 Edition Requires EHRs to enable a user to record, change, and access a patient’s family health history electronically using updated SNOMED CT (September 2015 Release)
- 88. Challenges to Family History Remain 85% Of women undergoing mammographies for were missing critical family history data in the EHR Incomplete family histories Michelle Lardner, Deputy CIO, NIH No major EHR vendor has native genomics tools or functionality…besides family history documentation, there is no place to create or document pedigree. Lack of advanced functionalities Welch BM, et al., Journal of Genetic Counseling, 2018 Despite the fact that…FHx tools support HL7 standards, integration with EHRs is still a challenge Lack of integration Commonly Cited Challenges Related to Family History in the EHR
- 89. Future Opportunities Health reform (e.g., QPP) - Specific measures within the MIPS encourage increased patient engagement and integration with third party tools (e.g., Advancing Care Information measure ACI_CCTPE_3 requires that patient- generated health data or data from a non-clinical setting is incorporated into the certified EHR technology) - Overall increased focus on population health management and accountable care incentivize prevention and early detection Technological advancements - Increase in the number of validated family history collection tools available on the market today, including patient-facing tools - Improved integration capabilities with SMART on FHIR and pluggable apps Regulatory and Technological Opportunities to Improve Family History
- 90. THANK YOU!
- 91. First Look: The NCCRT Risk Assessment and Screening Toolkit to Detect Familial, Hereditary, and Early Onset Colorectal Cancer Emily Edelman, MS, CGC April 26, 2018
- 92. Disclosures No conflicts to disclose. The Jackson Laboratory is a nonprofit biomedical research institution. JAX Education does not aim to increase use of commercial products or services.
- 93. Agenda Current use of CRC family history (FH) Electronic health record (EHR) opportunities Presentation of new toolkit Family history tools Next steps for dissemination and implementation Limitations and future opportunities
- 94. Current state of FH collection Among individuals with a family history of CRC: o <50% received appropriate screening o <40% have talked with a clinician about their family history Among individuals presenting with rectal bleeding o <40% have insufficient family history info documented to complete evaluate Fletcher 2007 JGIM; Cameron 2014 Patient Educ Couns; Weingart 2017 Jt Comm J Qual Patient Saf
- 95. Complex barriers to clinical integration 52.6% 47.4% 44.7% 28.9% PCP perceived barriers to integration Knowledge/ skills ELSI Systems Evidence Mikat-Steven 2014
- 96. A family history solution for primary care should address known barriers Provide education to build skills, point of care tools Translate evidence-based guidelines on FH collection and risk assessment Practical guidance on establishing FH processes and best practices o Identify opportunities to leverage the EHR and electronic tools and algorithms o Collaborating with genetic and cancer specialists
- 97. Overall Goal Develop a system that helps practices: Identify patients at increased/high risk based on personal and family history Apply screening guidelines based on risk Refer high risk patients to genetics Recognize and rapidly diagnose patients with a presenting CRC
- 98. Toolkit in Action Maya Reason for visit Establishing care Medical hx 34 yo Social hx Married, one son Family hx Father with CRC @ 62
- 99. Establish a system for structured assessment Develop a team-based approach to family history collection and interpretation. Use the EHR and/or external tools to assist in family history collection and risk assessment. Standardize how and where family history data is recorded in the medical record to increase the usability of this information.
- 100. Stepwise instruction
- 102. Example workflows
- 103. Curated tools
- 104. Worksheets
- 105. Use a tool to aid in family history collection and risk assessment High Increased Average Maya 34 y d. 50s dx. 50s dx. 43 60s dx. 50s 101 64 Hypothyroid 65 dx 62 80s80sd. 50 pneumonia d. 70s 70 50s 2 37 S.E. Asian
- 106. No one size fits all solution Cancer risk assessment systems Cancer Gene Connect (Invitae) Cancer IQ CRA Health Family History Tool (Myriad) Progeny (Ambry) Patient-centered collection tools Electronic My Family Health Portrait It Runs in My Family Paper Does It Run in the Family? Family Health Workbook SHARE workbook Primary care assessment systems Family Healthware MeTree MyLegacy Risk calculator NCI CRC Risk Assessment Tool Hereditary cancer mutation predictors MMRPredict MMRPro PREMM1,2,6 PREMM5 Patient-centered questionnaires CRC Risk Assessment Checklist Columbia 3-question survey SHARE workbook Simple FH Screening Tool for CRC UM 5-question survey User-friendly Lynch syndrome tool https://tinyurl.com/ycqeko6h
- 107. Example: Evaluating FH tools Practice’s FH goals o Identify patients at increased or high risk o Apply screening guidelines to patients based on risk level o Refer high risk patients to genetic services for further evaluation, counseling, and testing Desired FH tool features Structured collection of 1st and 2nd degree relatives Patient-entered collection Electronic questionnaire Risk assessment support Free
- 108. Example Using the FH Tool Features Worksheet, the practice can identify the tools that meet their desired needs: 1. CancerGene Connect/Invitae 2. CRA Health 3. My Family Health Portrait 4. Myriad Family History Tool 5. Progeny/Ambry The practice reviews and tests the tools to select one for use. https://tinyurl.com/ycqeko6h
- 109. Establish a system: additional components Select a set of CRC screening guidelines. Identify genetic and cancer specialists. Identify patient support materials and evidence-based interventions that can increase CRC screening adherence. Evaluate process and outcomes.
- 110. Assess risk Collect sufficient family history to enable risk assessment. Assess patterns and red flags. Assign to risk category: Average, increased (moderate or familial), high (hereditary).
- 111. Maya’s Family History Father: 65 y/o, CRC dx 62 Paternal aunt: Died in 50s due to endometrial cancer dx 50s Paternal uncle: 60s, gastric cancer dx 50s Paternal cousin: 44 y/o, CRC dx 43 Endometrial Cancer Gastric Cancer Colon Cancer Maya 34 y d. 50s dx. 50s dx. 43 60s dx. 50s 101 64 Hypothyroid 65 dx 62 80s80sd. 50 pneumonia d. 70s 70 50s 2 37 S.E. Asian
- 112. Identify genetic red flags and patterns Endometrial Cancer Gastric Cancer Colon Cancer Maya 34 y d. 50s dx. 50s dx. 43 60s dx. 50s 101 64 Hypothyroid 65 dx 62 80s80sd. 50 pneumonia d. 70s 70 50s 2 37 S.E. Asian Family history of multiple affected relatives Earlier age at onset of disease than expected
- 113. Colon, endometrial, and gastric cancers are associated in Lynch syndrome
- 114. Maya is at high risk Multiple affected relatives Early age of onset Possible dominant pattern of associated cancers
- 115. Communicate risk & manage patient based on risk Develop personalized plan for cancer screening, surveillance, and prevention, and genetic referral. Recommend colonoscopy for increased risk individuals. Communicate risk levels and management recommendations. Tailor risk communication to patient and needs. Recommend patients share risk information with relatives. Evaluate patients with alarm signs and symptoms for CRC
- 116. Stepwise instruction Implementation support and training
- 117. Tools
- 118. External education
- 119. Maya is a candidate for cancer genetic evaluation & testing Referral to cancer genetics Genetic counseling Genetic testing for Lynch syndrome, and potentially other genes Personalized management, prevention and surveillance
- 120. Maya has homework Talk to family members with cancer Learn more about cancer history Be aware testing may be recommended for affected relatives first
- 121. Should I have a hysterectomy now? Is it dangerous to have more children? What does this mean for my son? Is there anything I can do to stop cancer? If gene-positive, Maya has questions
- 122. Early onset CRC is on the rise Recognize that the incidence of CRC is increasing in individuals under age 50. Be aware that a substantial proportion of early onset CRC may be prevented or detected at an earlier stage by identifying people with a family history of cancer and adenomas. Regardless of age, consider CRC in the evaluation of patients with alarm signs and symptoms, including: o blood in the stool o recent-onset and persistent or progressive diarrhea/constipation o persistent or progressive abdominal pain o abdominal mass o unexplained iron deficiency anemia o unexplained weight loss
- 123. A comprehensive family history and early onset CRC toolkit
- 124. Toolkit design supports applying skills and implementing processes and tools Step-wise instruction to help practices: o Establish a structured process o Improve clinical skills Tools and worksheets with worked examples Case studies and tips Appendix of guidelines, educational resources and websites
- 125. Looking ahead Launch at nccrt.org o In coordination with release of updated ACS CRC screening guidelines Dissemination Implementation o Looking for interested practices and partners! Evaluation
- 126. Toolkit limitations FH and EAO focus, not comprehensive to include all aspects of cancer genetics CRC focus rather than comprehensive risk assessment across conditions Limited evidence-based best practices Family history tools and EHR limitations Assumes organizational buy-in Practice variation, assumes need for some customization and modifications based on experience
- 127. Opportunities for the future 1. Validate CRC FH screening tools in toolkit for primary care. 2. Develop an electronic version of FH screening tools and/or provide them to EHR vendors. 3. Develop a CRC risk assessment calculator for providers that integrates personal history, lifestyle risk factors, and family history for use in the general population. 4. Implement the toolkit and evaluate the process of implementation. 5. Collaborate with professional societies and other stakeholders to develop a comprehensive risk assessment tool or process that includes CRC along with other conditions. 6. Develop an awareness campaign about EAO CRC for front line providers. 7. Further evaluate needs and opportunities related to patient education and engagement re: FH. 8. Provide minimum requirements and best practices regarding FH to EHR vendors. 9. Research solutions for portability of family history across EHRs and health systems.
- 128. Acknowledgements Authors Emily Edelman, MS, CGC Therese Ingram, MA Kate Reed, MPH, ScM, CGC Linda Steinmark, MS, LCG Paige Tanner, BS NCCRT FH-EAO Task Force Leadership Dennis Ahnen, MD Paul Schroy, MD, MPH Thomas Weber, MD, FACS Advisors Cindy Borassi Anjee Davis, MPPA Robin Dubin, MBA Greg Feero, MD, PhD Stephanie Guiffre, MPA Heather Hampel, MS, LGC Djenaba Joseph, MD, MPH Xavier Llor, MD, PhD Susan Miesfeldt, MD Martha Raymond, MA, CPN Michelle Tropper, MPH Jennifer Weiss, MD Reviewers & Contributors Siobhan Dolan, MD, MPH Caitlin Gutheil, MS Paul Han, MD, PhD Kenneth Lin, MD, MPH, FAAFP Leigh LoPresti, MD Natalie Mikat-Stevens, MPH Trudie Milner, PhD Randa Sifri, MD Alissa Terry, ScM, CGC Primary care interview participants NCCRT & ACS Leadership Caleb Levell Mary Doroshenk, MA Rebecca Siegel, MPH Durado Brooks, MD, MPH Robert Smith, PhD Funding This toolkit was supported by the Grant or Cooperative Agreement Number, DP004969-04, funded by the Centers for Disease Control and Prevention.
- 131. Toolkit goals & objectives Goals • Enable primary care providers to implement a structured family history collection and screening process for familial, hereditary, and early onset cancer • Facilitate timely diagnostic evaluation of patients with signs or symptoms of early onset CRC Learning objectives 1. Create a system to integrate family history collection and screening into practice flow 2. Identify patients at increased or high risk based on personal and/or family history 3. Apply screening guidelines to patients at increased and high risk 4. Refer high risk patients to genetic services for further evaluation, counseling, and testing 5. Include CRC in the differential diagnosis of adults under age 50 with alarm signs and symptoms
- 132. Development process Needs assessment o Literature review o Environmental scan of tools and resources o Identification of best practices in primary care o Interviews with PCPs Design: Identify learning objectives, content, and instructional strategy Develop content, adapt existing content as indicated Iterative review and revisions o content review with experts o target audience review o NCCRT advisor review
- 133. FH tools for primary care Desired features of a FH tool for primary care Structured collection of 1st and 2nd degree relatives Clinical decision support Patient entered collection Validated for primary care Electronic and paper collection options Maintained technology and clinical content Electronic risk assessment EHR integration Risk stratification to separate categories: average, increased, high Patient/health system owns data Personal as well as FH risk Free Assesses multiple conditions Spanish/ other language versions available
- 134. THANK YOU For permission to share these slides please contact Cindy Borassi, Executive Director, Colon Cancer Foundation info@coloncancerchallenge.org 4TH ANNUAL EARLY AGE ONSET COLORECTAL CANCER SUMMIT #EAOCRC18
