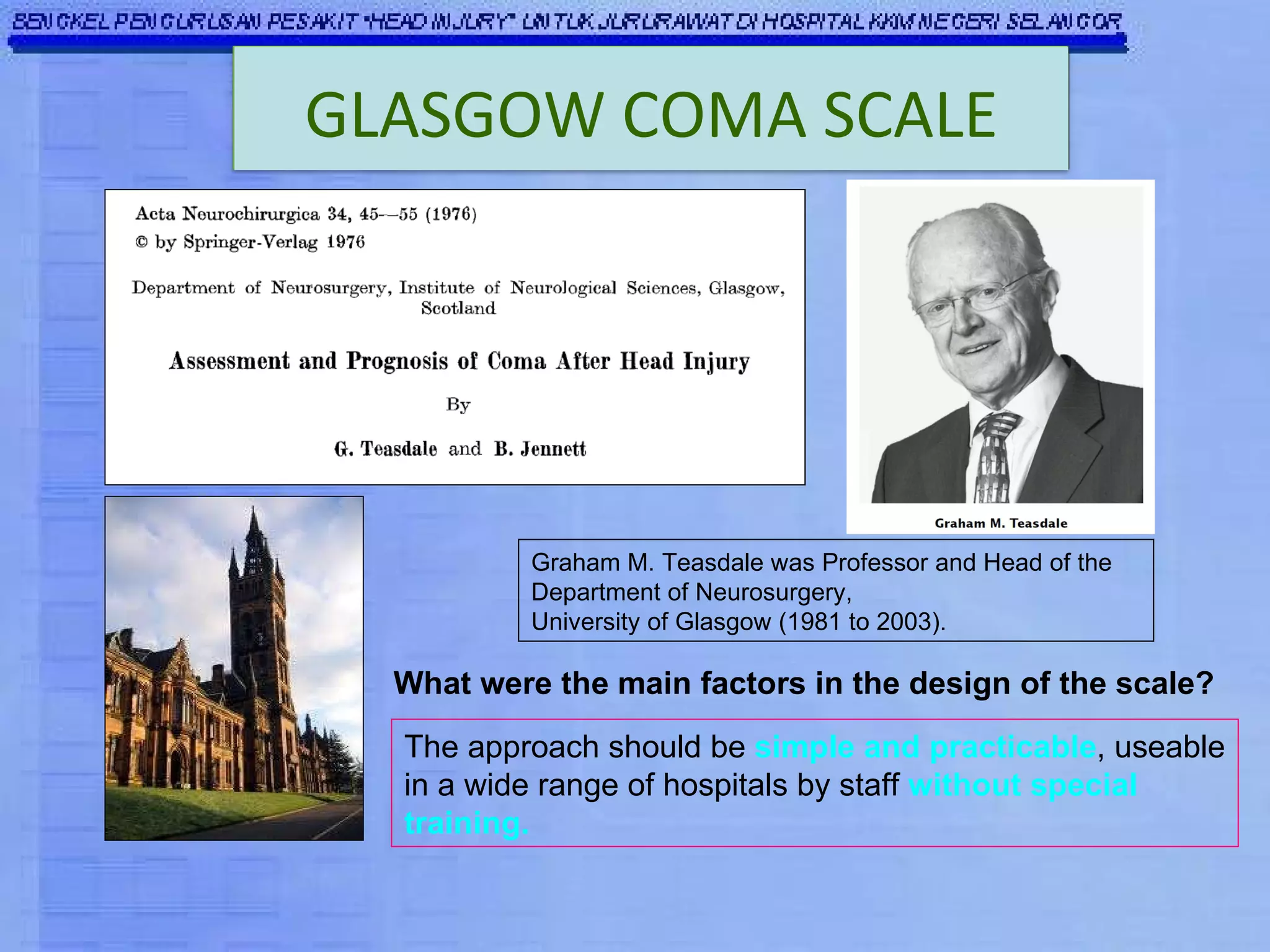
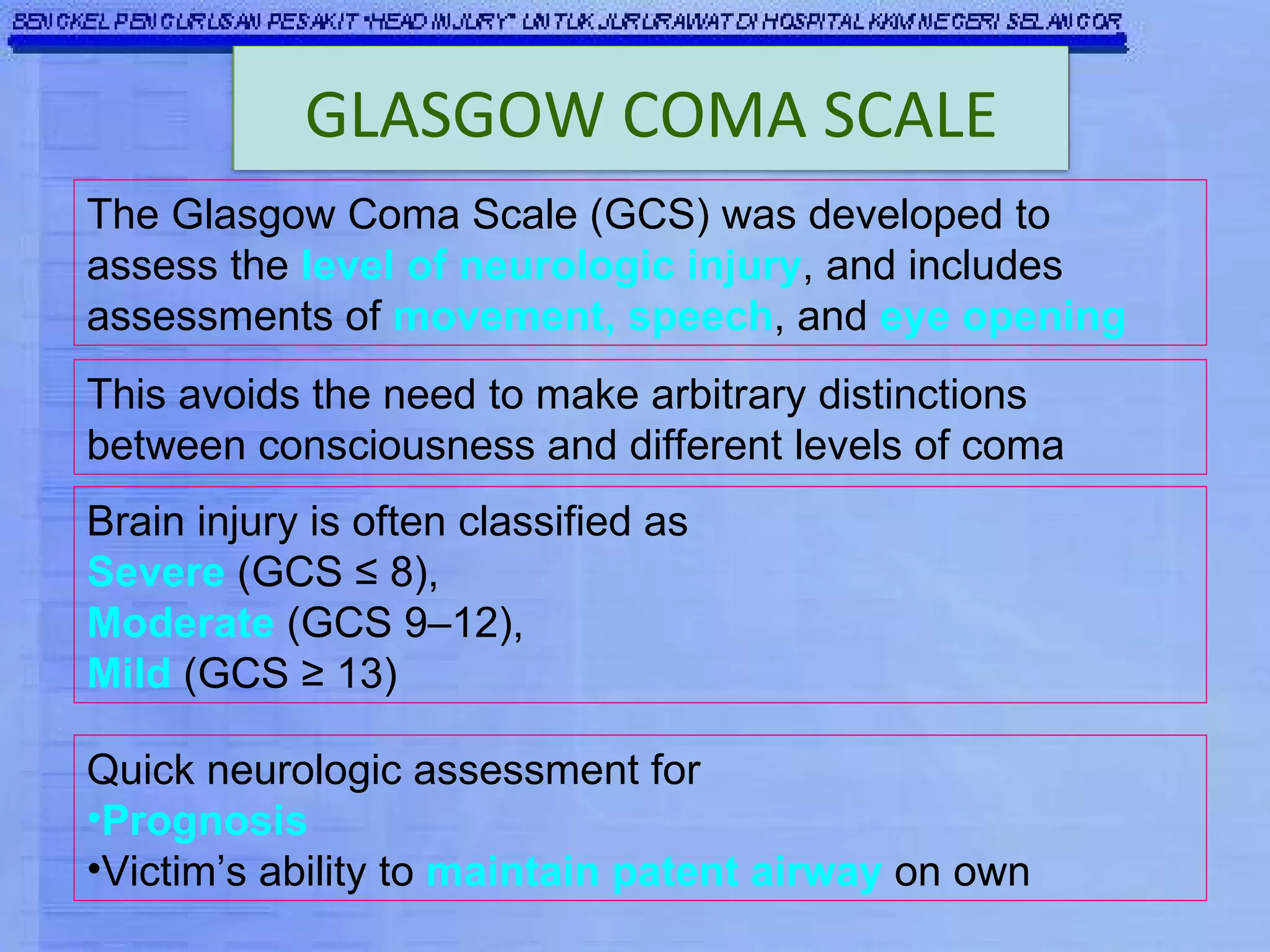
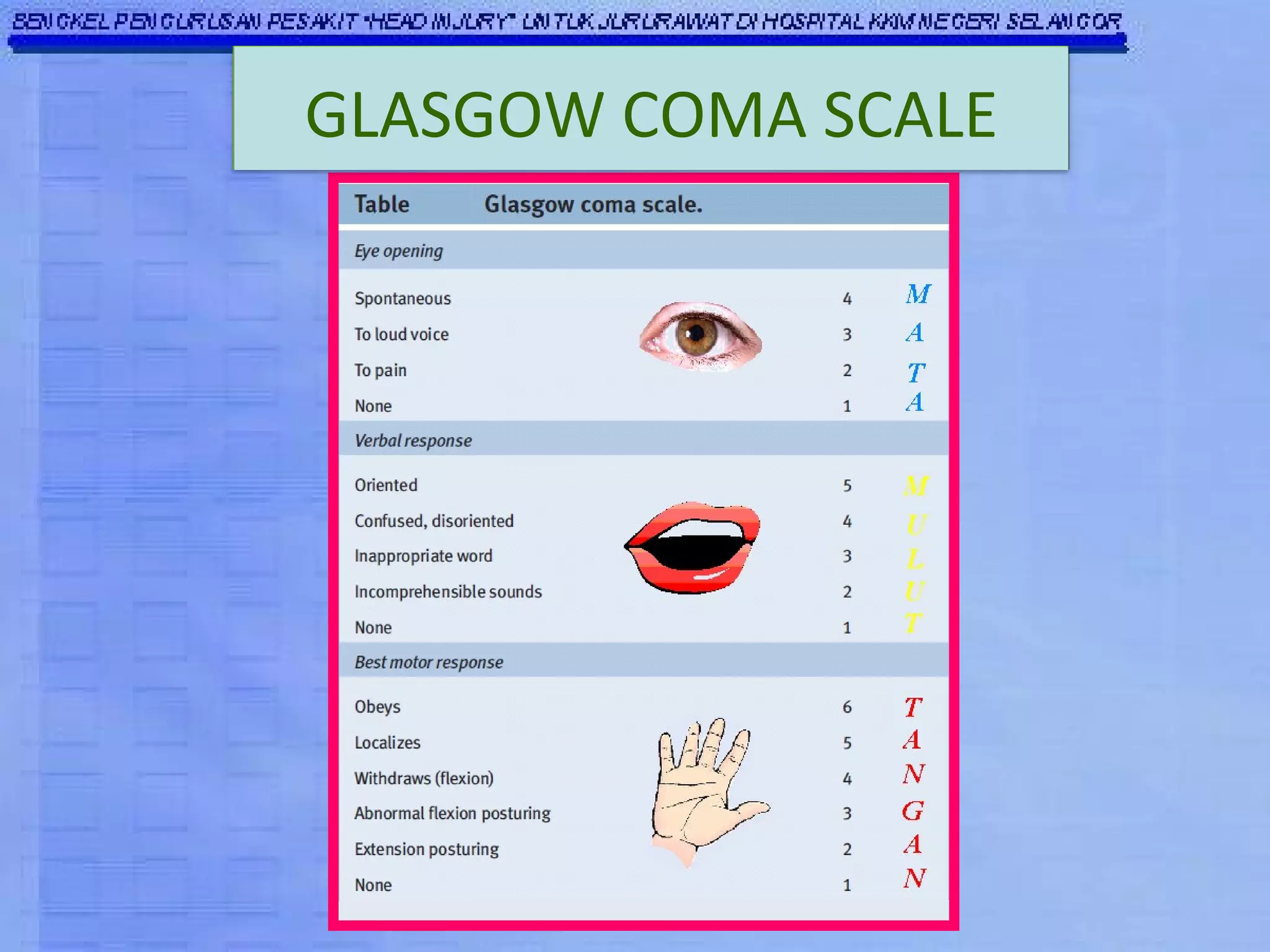
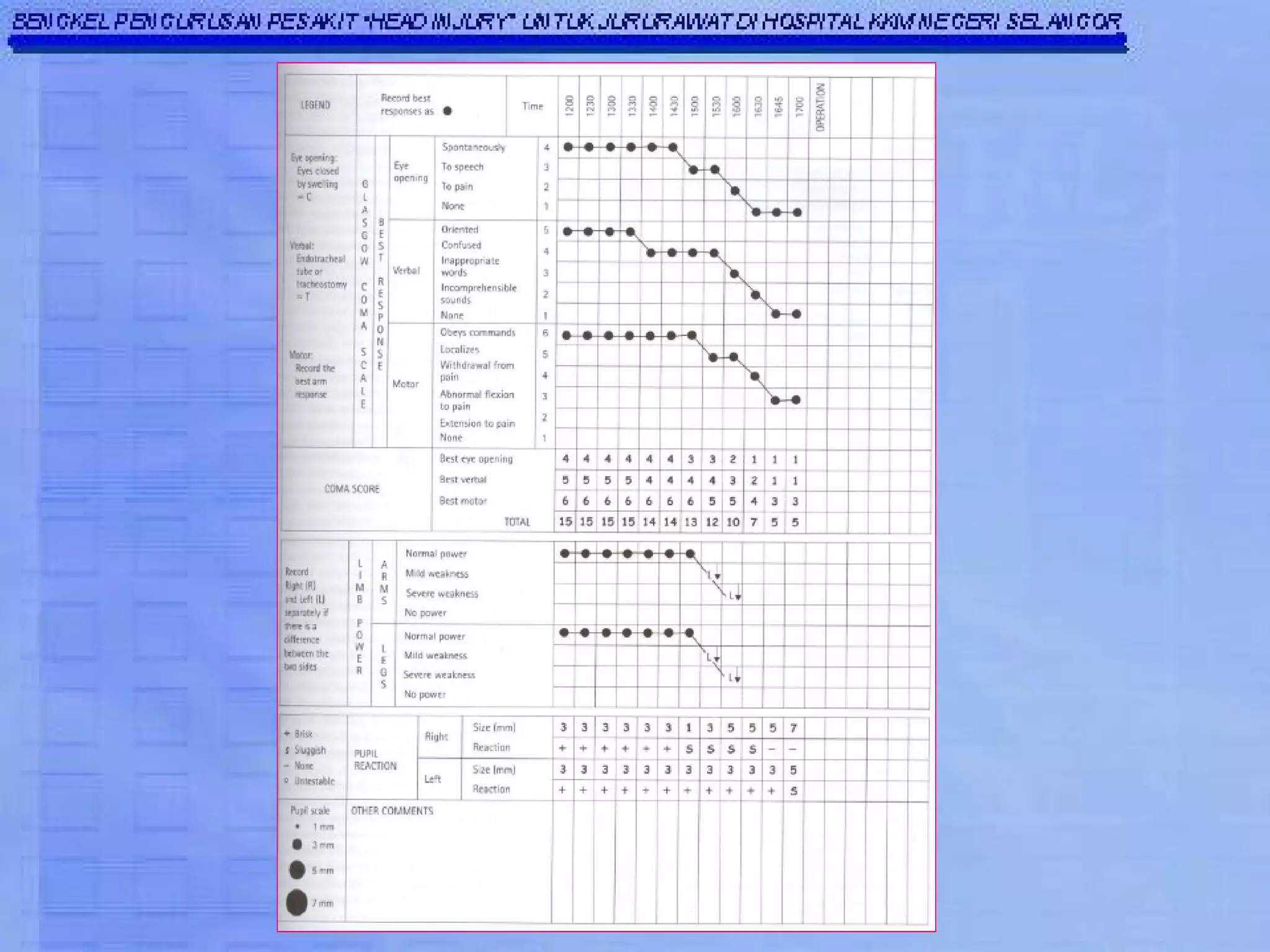
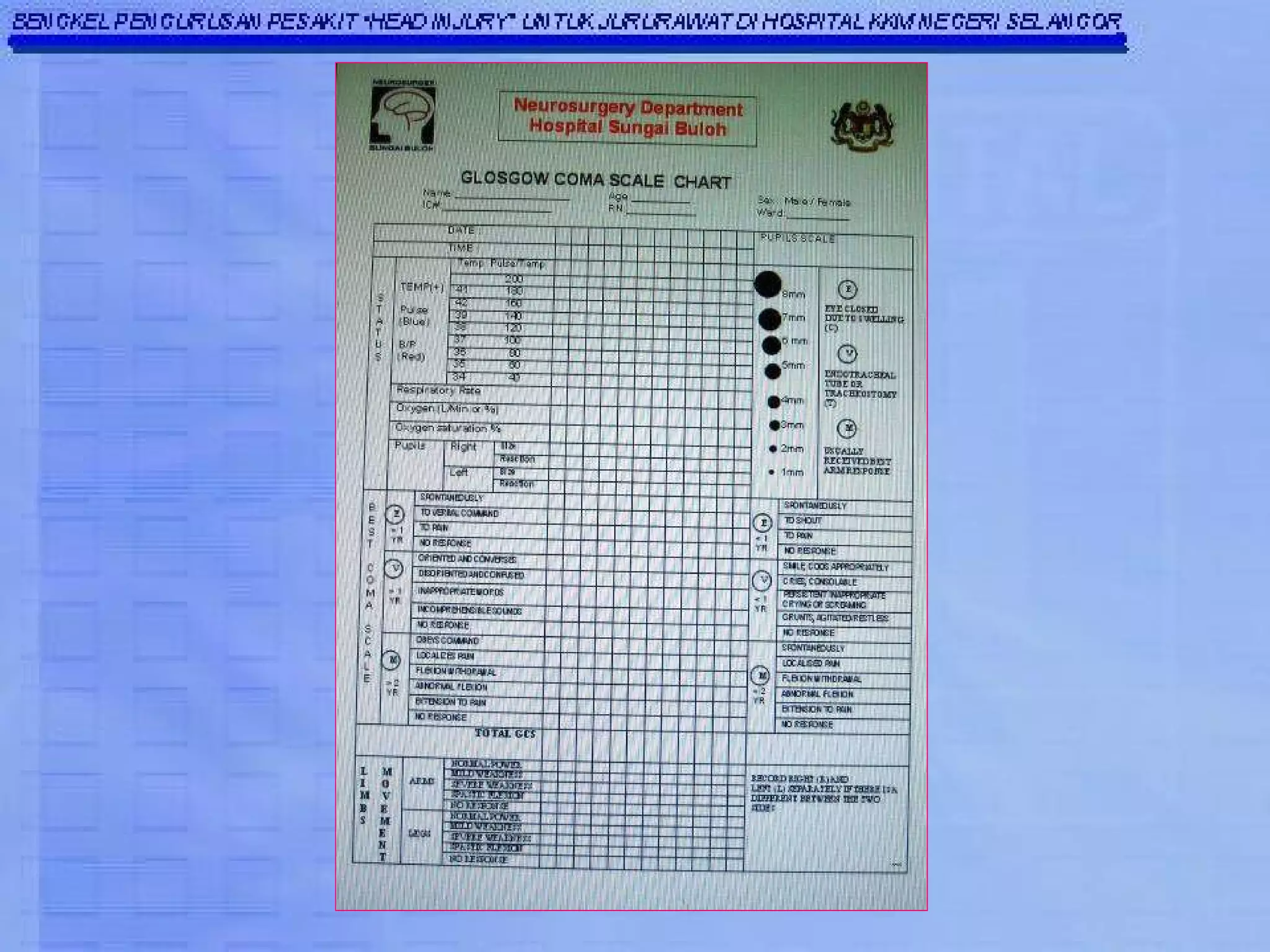
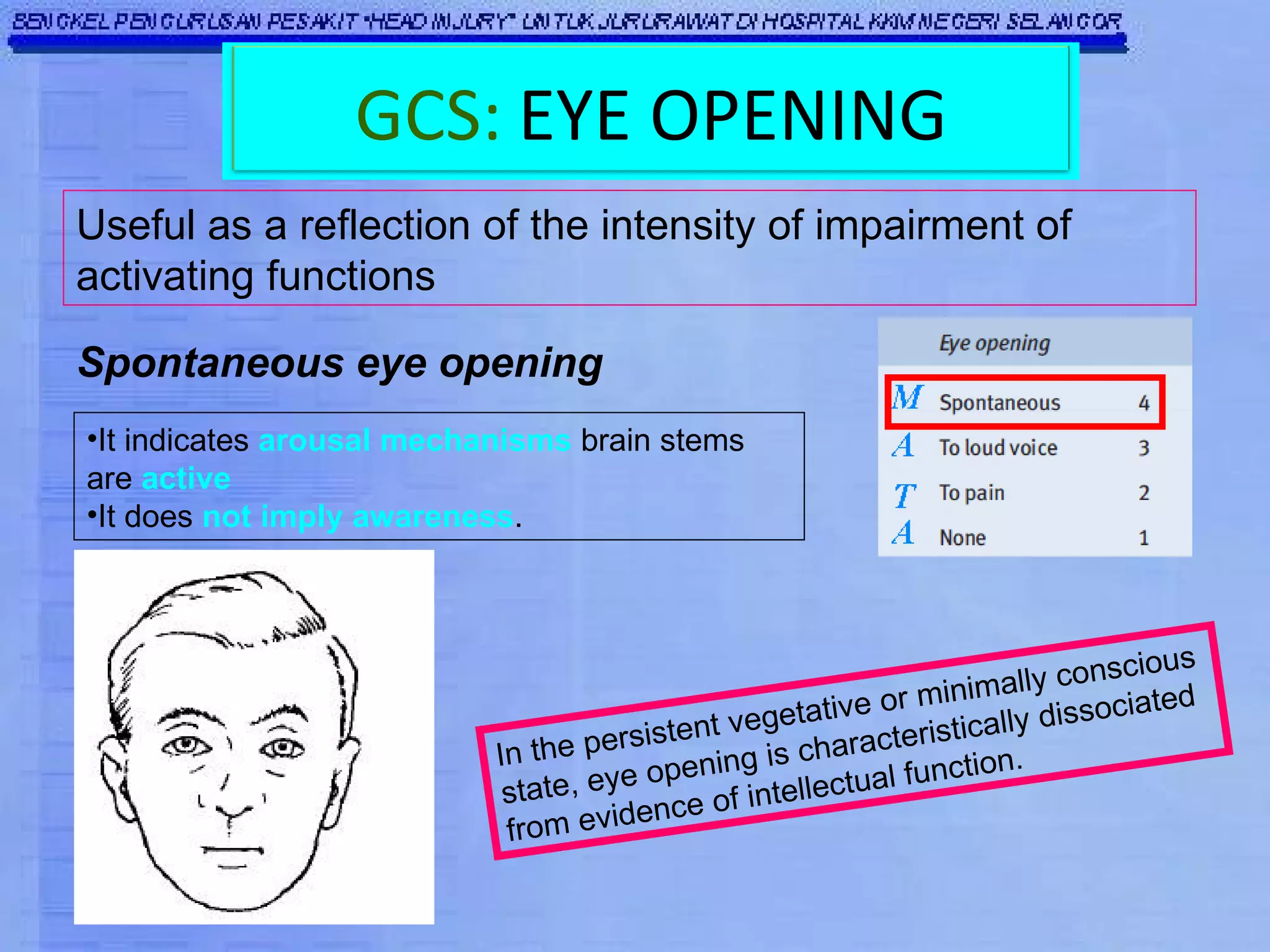
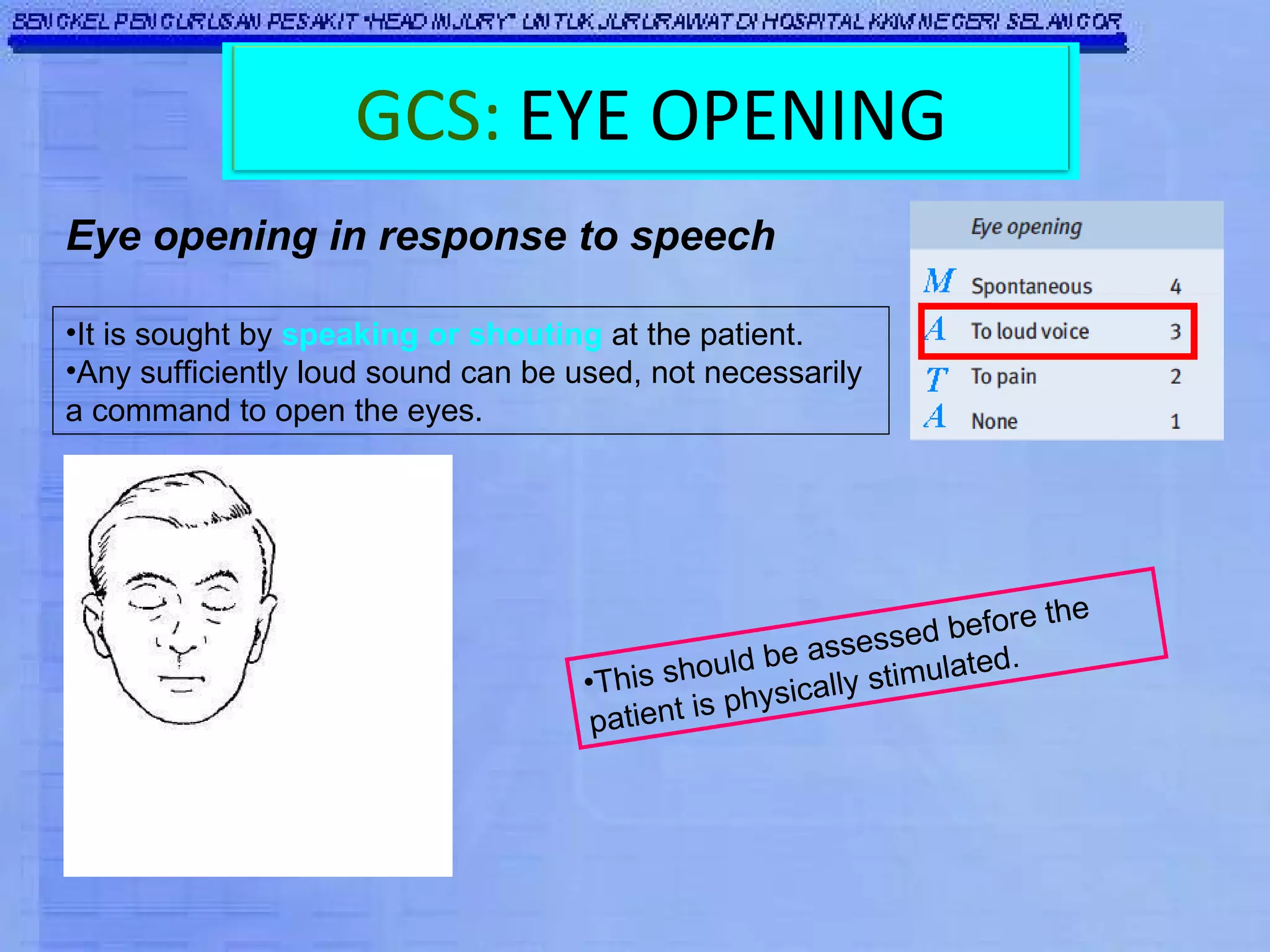
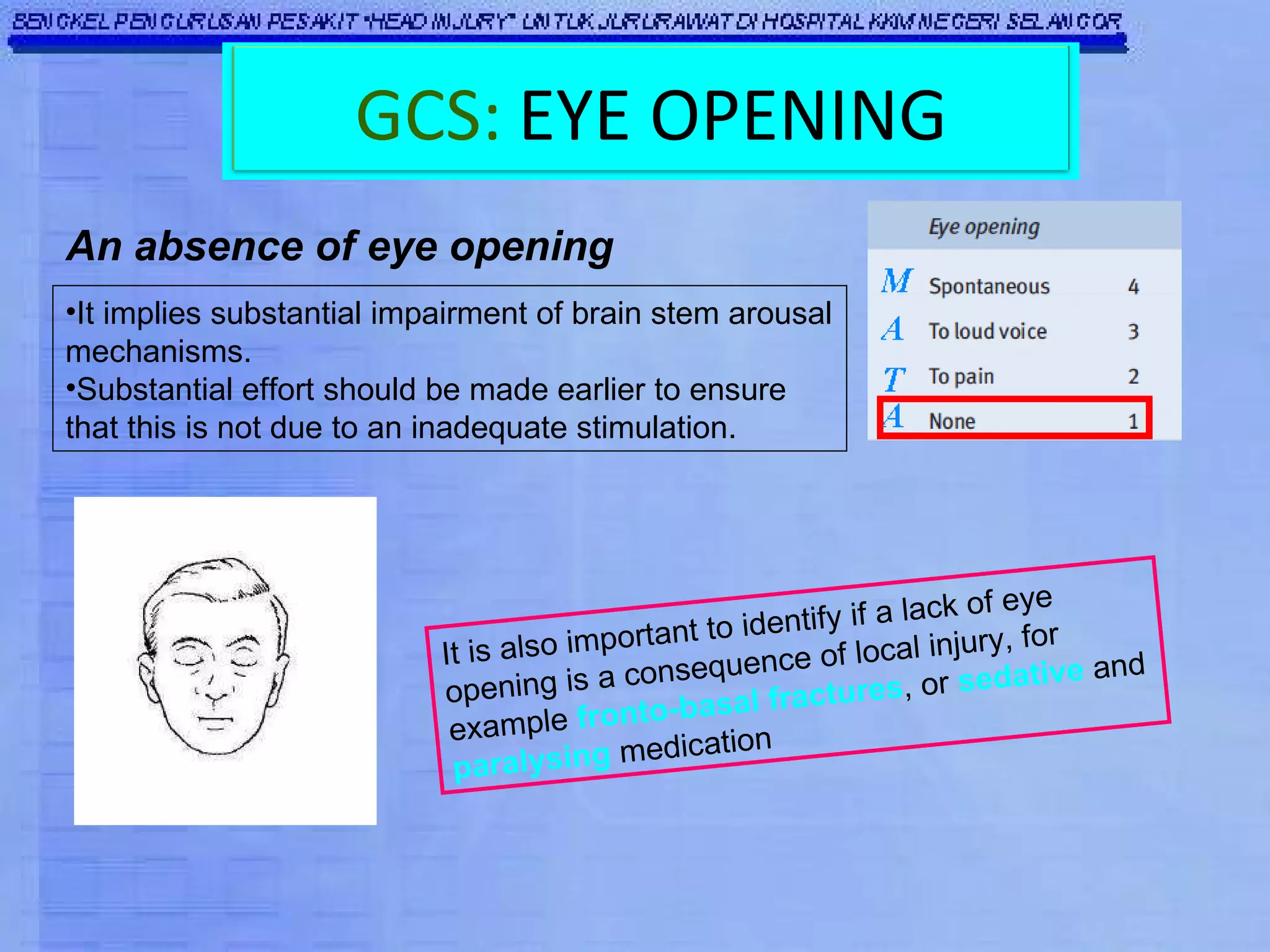
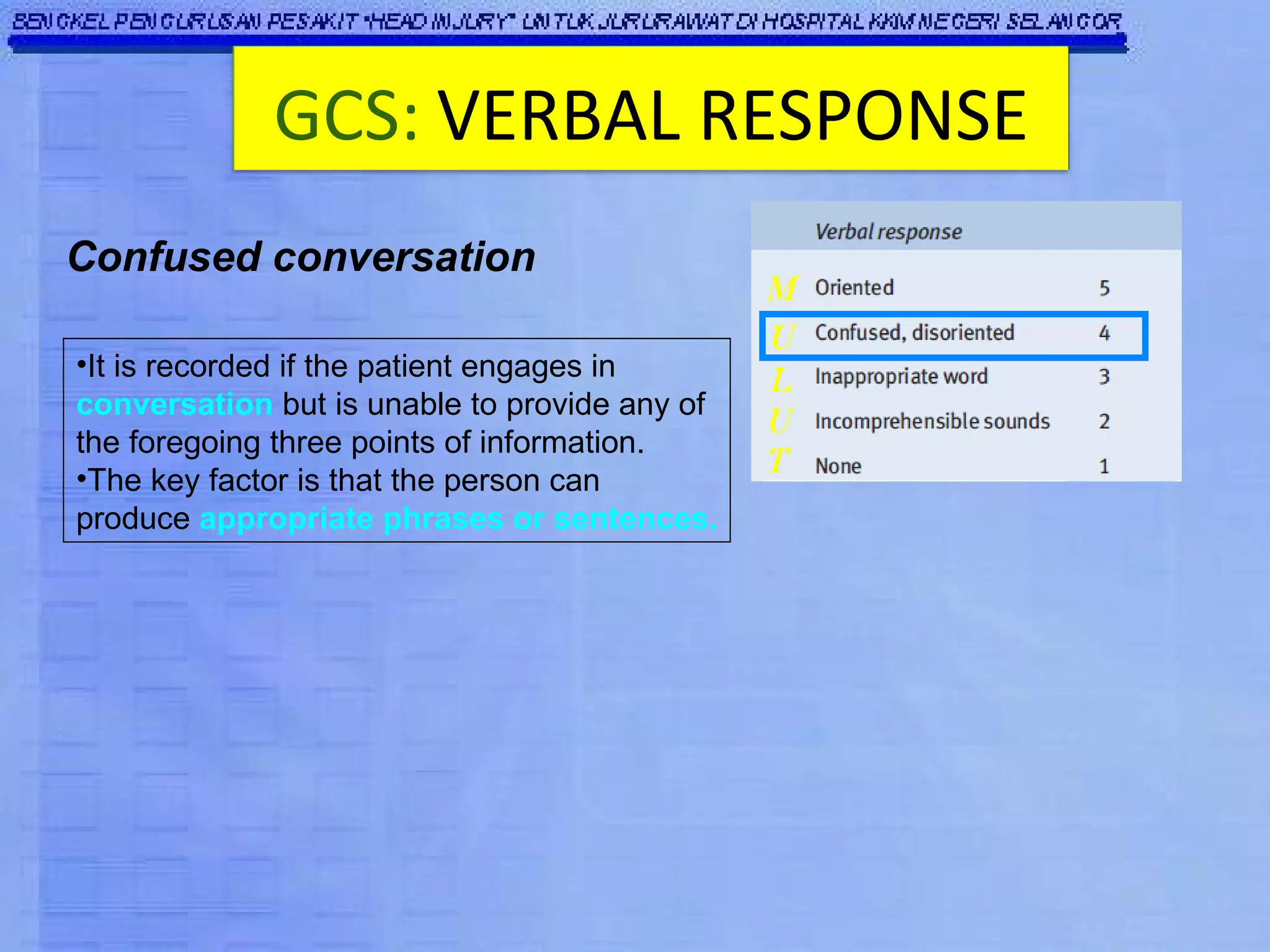
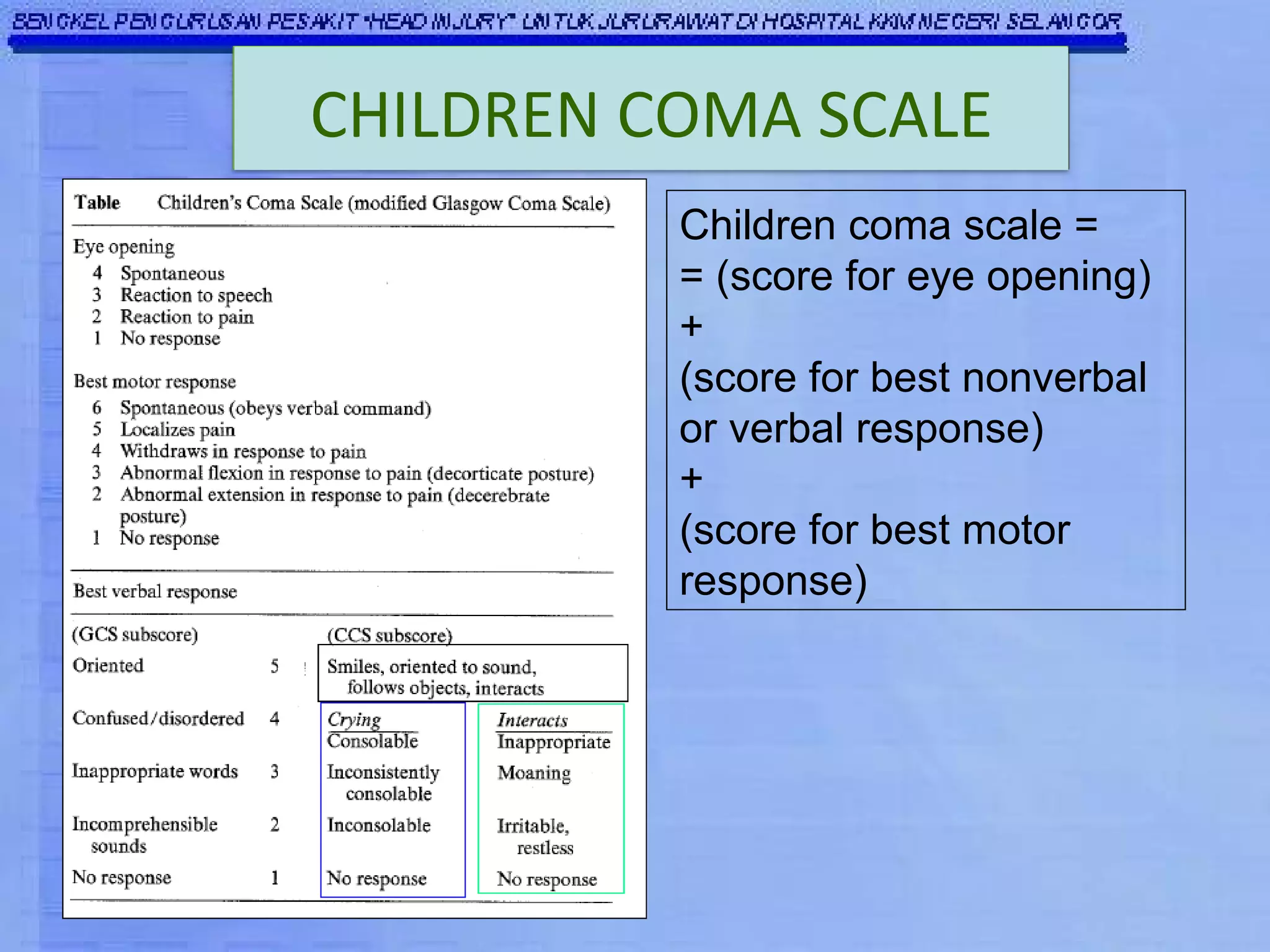
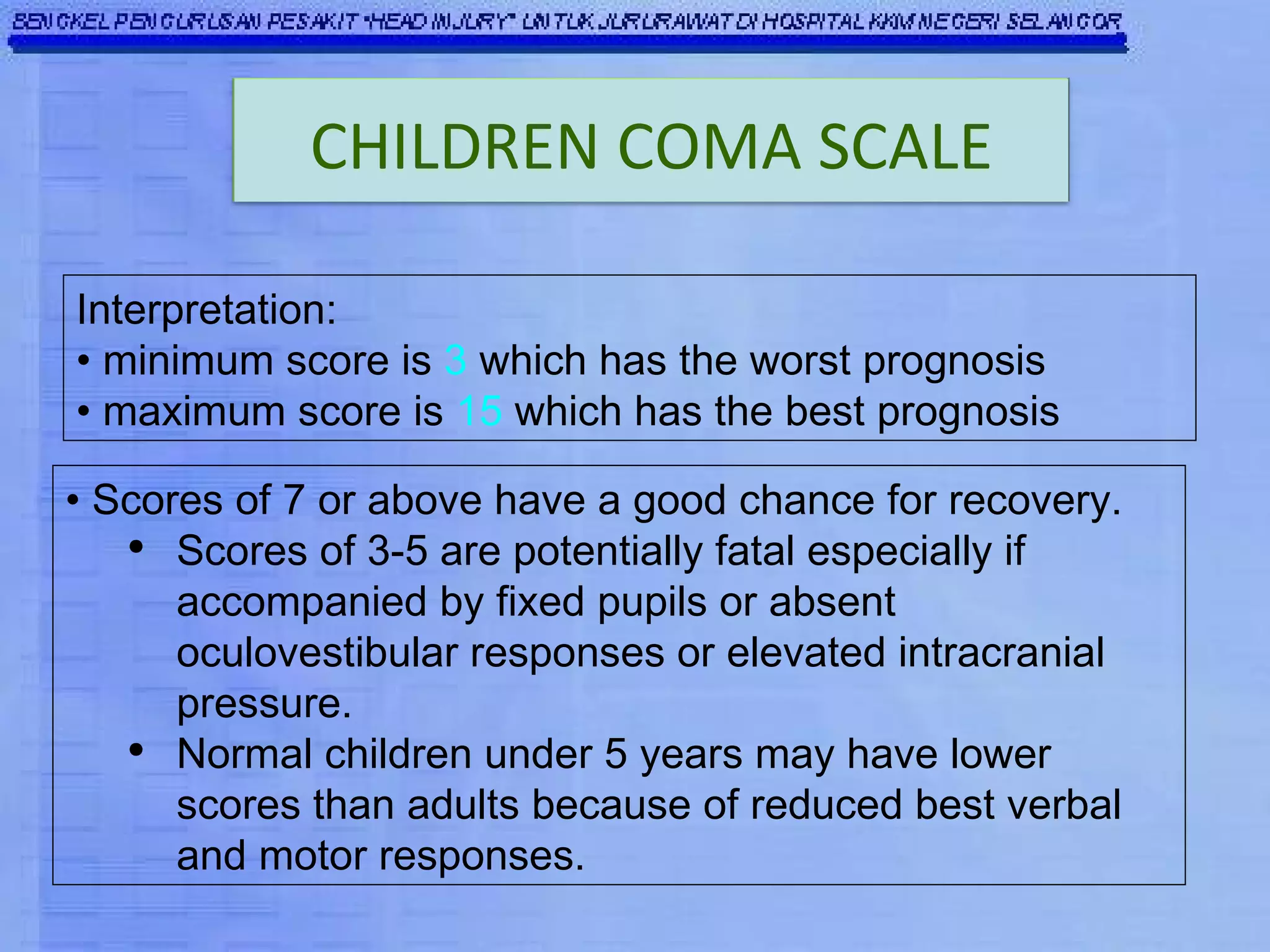
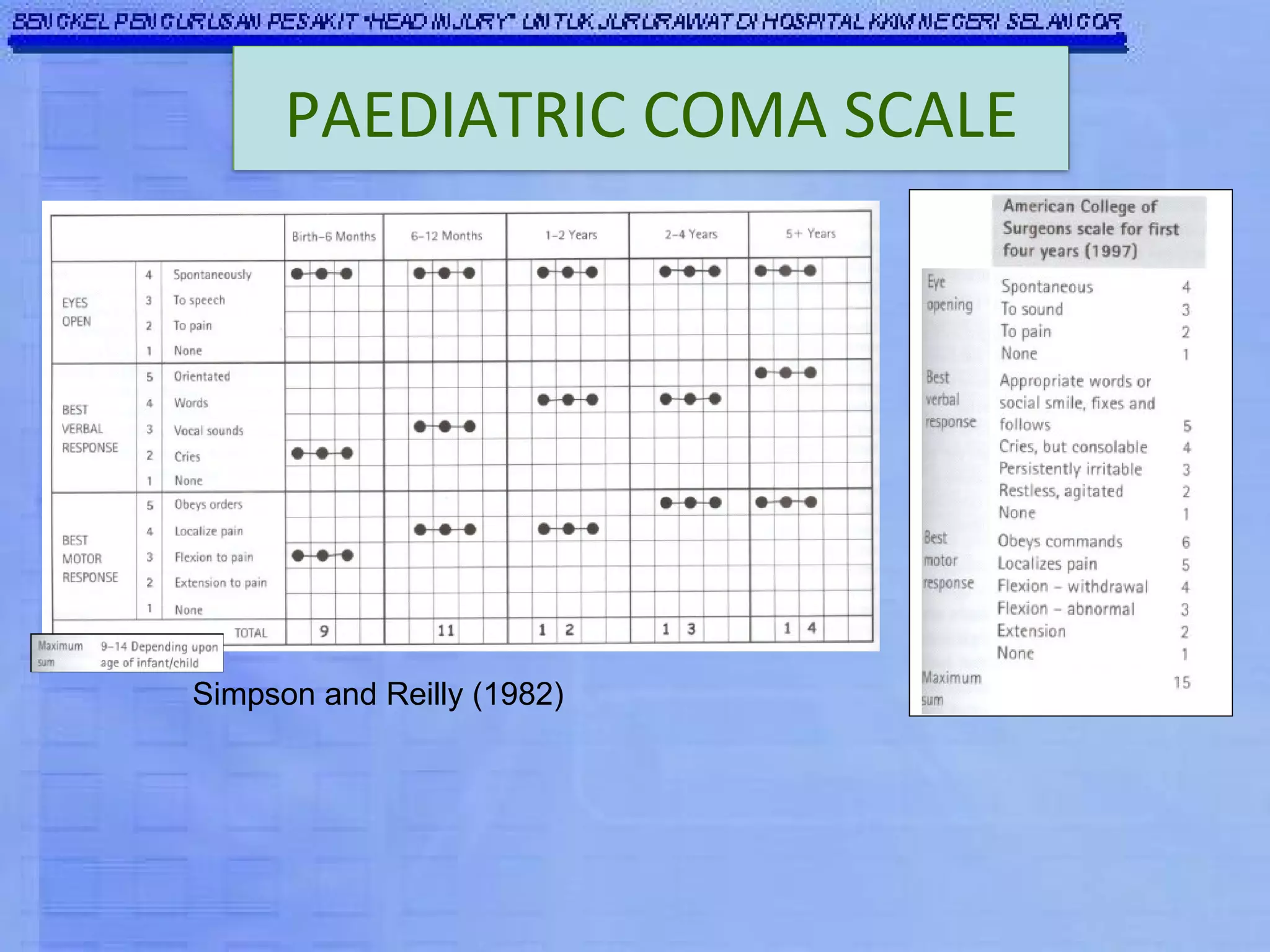
The Glasgow Coma Scale (GCS) was developed to assess the level of neurological injury from brain trauma. It assesses eye opening, verbal response, and motor response on a scale of 3 to 15, with lower scores indicating more severe brain injury. The GCS provides a practical and consistent way to monitor head injury patients and indicates their level of impairment, prognosis, and likelihood of recovery. It is an important tool used worldwide in hospitals to evaluate brain injury.