Trauma Bay Care for Abuse Patients
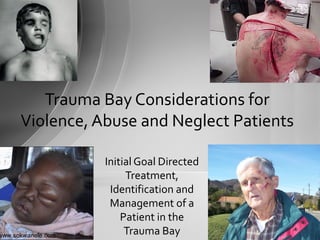
- 1. www.sokwanele.com Initial Goal Directed Treatment, Identification and Management of a Patient in the Trauma Bay Trauma Bay Considerations for Violence, Abuse and Neglect Patients
- 2. • The images and information in this presentation are a sad and realistic part of our life in the ED. • In this presentation we will hear, see and speak about abuse, neglect and violence and discuss our roles in managing these patients. Clinical Warning Clipart.com
- 3. “When people go to work, they shouldn't have to leave their hearts at home.” Author: Betty Bender Excuse yourself if you must, we will understand
- 4. • Define: – Child abuse and neglect – Elder abuse and neglect – Domestic Violence • Identify the primary and secondary role of the Nurse in managing the care of a trauma patient/victim. • Case based discussion of care models for the patient/victim. • Discuss and determine actions related to recognition and preservation of a possible crime and crime scene evidence. • Review the standards of identifying and reporting suspected cases for all ED Nurses. • Define and discuss the resources available to all nurses in supporting the possible victim of a crime of abuse or neglect. Objectives
- 5. Answer: • The ABCDEs – Patient care is always the essential focus • Save the life then move on to: 1. Ask “what’s not right with this” 2. Preserve the evidence and report • When possible preserve evidence from the beginning, if resources and medical conditions allow Pop Quiz Question: What are the initial critical steps when taking care of a traumatic injury patient who you suspect of being a victim of violence, abuse or neglect?
- 6. • Systematic patterns of behavior in a relationship that are used to gain and/or maintain control and power over another. – Emotional abuse • Includes hurting another person's feelings by saying cruel, unfair comments or by name calling – Psychological Abuse • Any threat to do bodily harm to a partner, a child, a family member, friends, pets, or one's self (suicide). – Sexual Abuse • Any non-consenting sexual act or behavior. – Physical Abuse • Any forceful or violent physical behavior. Definition of Abuse (Adult or Child) Source: Domestic Abuse Project
- 7. Child abuse and neglect is defined by Federal and State laws and can vary state by state. – The Federal Child Abuse Prevention and Treatment Act (CAPTA) provides minimum standards that States must incorporate in their statutes. – The CAPTA definition of "child abuse and neglect," at a minimum, refers to: • "Any recent act or failure to act on the part of a parent or caretaker, which results in death, serious physical or emotional harm, sexual abuse, or exploitation, or an act or failure to act which presents an imminent risk of serious harm" Child Abuse Defined Source: The Federal Child Abuse Prevention and Treatment Act (CAPTA)
- 8. • Broadly defined (and varies state by state) • There are three basic categories of elder abuse: – Domestic elder abuse • By someone who has a special relationship with the elder (a spouse, a sibling, a child, a friend, or a caregiver), that occur in the elder’s home, or in the home of a caregiver. – Institutional elder abuse • Generally occurs in residential facilities for older persons (e.g., nursing homes, foster homes, group homes, board and care facilities). • Perpetrators are persons who have a legal or contractual obligation to provide elder victims with care and protection (e.g., paid caregivers, staff, professionals). – Self-neglect or self-abuse • “Self care deficit” type issues due to lack of caring about ones own life, financial concerns, or the focus of caring for a spouse Definition of Elder Abuse and Mistreatment Source: US Centers for Aging
- 9. • The willful intimidation, assault, battery, sexual assault or other abusive behavior perpetrated by one family member, household member, or intimate partner against another. – In most state laws addressing domestic violence, the relationship necessary for a charge of domestic assault or abuse generally includes a spouse, former spouse, persons currently residing together or those that have within the previous year, or persons who share a common child. – As of 2007, a majority of states provide some level of statutory protection for victims of dating violence. Definition of Domestic Violence Source: National Center for Victims of Crime
- 10. ABCDE… is Your First Objective Saving the life of your patient is your primary role! Then ask yourself: 1.What’s wrong with this story? 2.How can I help preserve evidence? 3.Who do I need to report this to?
- 11. • Consider preservation of evidence as soon as you suspect a crime – Implement it only if it doesn’t slow or jeopardize care in any way – Make certain everyone in the room is aware of the plan to preserve – Limit the number of people who touch what is placed in the bag – always wear gloves – Consider having multiple open paper bags on the floor when the pt arrives After the ABCDE… Preserve the Evidence
- 12. • Everything goes into paper bags – This includes sheets the patient was transferred to the ED on (from the ambulance) – Nothing goes into plastic – One bag per item (or item type) is the most practical to avoid cross contamination of evidence • Bags should be sealed with tape and labeled with name (or trauma alias), date, time and initials and provided to PD as soon as possible – Seals should not be pt labels (the MRN is considered PHI) – If at all possible, do not leave the bags unattended After the ABCDE… Preserve the Evidence
- 13. • Consult the PD if it is suspected that the hands should be paper bagged (for evidence collection from the hands later) – Typically only done if the patient is dead or stable – Only with the Trauma Surgeon’s consent – Never impact care and assessment needs of the hands • It gets in the way of assessment, art lines etc… • If you need to clean the patient for a procedure, clean only the required area and then save the cleaning materials After the ABCDE… Preserve the Evidence
- 15. • Think First… • Remember: –ABCDE… –Save the life –Ask: “What’s not right with this?” –Preserve and Report Case Scenario:
- 16. • EMS Report – Code Yellow: – 8y/o male fell down a flight of stairs – c/o buttock pain, right forearm deformity, headache with possible short +LOC. – Pt is very calm, constantly asking if his Mom is there, GCS 15 – Vitals WNL, C-collar, LBB, right arm splinted +PMS Case Scenario #1
- 17. Case Scenario #1 • EMS Report – Code Yellow: – 8y/o male fell down a flight of stairs – c/o buttock pain, right forearm deformity, headache with possible short +LOC. – Pt is very calm, constantly asking if his Mom is there, GCS 15 – Vitals WNL, C-collar, LBB, right arm splinted +PMS Would a 8 year old fall down an entire flight of stairs”? Is this normal?
- 18. Case Scenario #1 • EMS Report – Code Yellow: – 8y/o male fell down a flight of stairs – c/o buttock pain, right forearm deformity, headache with possible short +LOC. – Pt is very calm, constantly asking if his Mom is there, GCS 15 – Vitals WNL, C-collar, LBB, right arm splinted +PMS Are these reported injuries consistent with falling down a flight of stairs?
- 19. • EMS Report – Code Yellow: – 8y/o male fell down a flight of stairs – c/o buttock pain, right forearm deformity, headache with possible short +LOC. – Pt is very calm, constantly asking if his Mom is there, GCS 15 – Vitals WNL, C-collar, LBB, right arm splinted +PMS Case Scenario #1 How calm would a 8 year old be, after being placed in a board and collar, and now in a trauma bay with people pulling off clothes, etc…? Social Development wise… how many 8 year olds would rather have Mom over Dad?
- 20. • Findings in the Trauma Bay: – 8 year old male – Airway clear – Name is Oliver – Multiple head contusions – Right forearm deformity – Circumferential contusion (some old some new) both wrists – Bilateral knee abrasions with full ROM – Contusions to anterior/superior chest wall, spaced at either side of sternum – Multi layer contusions to the buttock – No blood at meatus Case Scenario #1 www.philosophyblog.com.au http://www.fordarlieroutier.org http://www.fordarlieroutier.org
- 21. • Findings in the Trauma Bay: – 8 year old male – Airway clear – Name is Oliver – Multiple head contusions – Right forearm deformity – Circumferential contusion (some old some new) both wrists – Bilateral knee abrasions with full ROM – Contusions to anterior/superior chest wall, spaced at either side of sternum – Multi layer contusions to the buttock – No blood at meatus Case Scenario #1 www.philosophyblog.com.au http://www.fordarlieroutier.org http://www.fordarlieroutier.org Do all these injuries make sense based on the mechanism of injury? If not does it matter why?
- 22. • What did you do for Oliver in the Trauma Bay? – ABCDE… – What about rectal tone on this patient? • Would you, what considerations would you take, if any? – Emotional Support – Definitive diagnostics and treatment – Observe and assess interactions with staff and family • What can you do for Oliver after the Trauma Resuscitation? – Continue with the above – Report your concerns/suspicions • Why? Case Scenario #1
- 23. The Latest Data Child Abuse/NeglectBelfastTelegraph www.thesun.co.uk
- 24. • During 2008, an estimated 772,000 children were determined to be victims of abuse or neglect. Child Abuse is Everywhere Source: HHS 2008 Child Maltreatment Annual Reports •Children in the age group of birth to one year had the highest rate of victimization. •Female 51.3% •Male 48.3% •45.1% were Caucasian, 16.6% were African-American, and 20.8% were Hispanic.
- 25. • An estimated 1,740 children died due to child abuse or neglect – 71.1% of all victims suffered neglect – 16.1% of all the victims suffered physical abuse – 9.1% of all the victims suffered sexual abuse – 7.3% of all the victims suffered from psychological maltreatment (A child may have suffered from multiple forms of maltreatment and was counted once for each maltreatment type.) 2008 Types of Abuse Source: HHS 2008 Child Maltreatment Annual Reports
- 26. • Most were parents or relatives – 80.1% of perpetrators of child maltreatment were parents • 90.9% were the biological parent of the victim – 6.5 % were other relatives of the victim • Perpetrators – Female 56.2% – Male 42.6% – 75.2% younger than age 40 • Of the perpetrators who were child daycare providers, 21.2% committed sexual abuse. Who is Abusing Children Source: HHS 2008 Child Maltreatment Annual Reports
- 27. • Healthcare workers are legally required to report suspicion observed in their line of service – The code limits required reporting to persons acting in their professional or official capacities. • However anyone can report • Does not require a medical professional to report, if not in their line of service • The Code does not require clear determination of fact or “proof” • Report to the police, immediately if you fear risk of immediate harm Virginia Code 63.2-1509 Reporting Child Abuse/Neglect Source: http://leg1.state.va.us
- 28. • No legal ramifications for the reporter – Immune from civil and criminal liability (unless done in malice) • No obligation to advise family of the report • Failure to report within 72 hours of suspicion can result in fines and license action. • “A mandated reporter [e.g. Nurse] who has reason to suspect that a child is an abused or neglected child shall report the matter immediately to the local department of the county or city wherein the child resides or wherein the abuse or neglect is believed to have occurred or to the toll-free child abuse and neglect hotline of the Department of Social Services.“ Virginia Code 63.2-1509 Reporting Child Abuse/Neglect Source: http://leg1.state.va.us
- 29. Virginia Code Citation: Ann. Code § 63.2-100 • No child who in good faith is under treatment solely by spiritual means through prayer, in accordance with the tenets and practices of a recognized church or religious denomination, shall for that reason alone be considered to be an abused or neglected child. • Further, a decision by parents who have legal authority for the child, or in the absence of parents with legal authority for the child, any person with legal authority for the child, who refuses a particular medical treatment for a child with a life-threatening condition shall not be deemed a refusal to provide necessary care if: – The decision is made jointly by the parents or other person with legal authority and the child. – The child has reached age 14 and is sufficiently mature to have an informed opinion on the subject of his or her medical treatment. – The parents or other person with legal authority and the child have considered alternative treatment options. – The parents, or other person with legal authority, and the child believe in good faith that such decision is in the child's best interests. Religious Child Abuse/Neglect Exceptions
- 30. “A mandated reporter shall disclose all information that is the basis for his or her suspicion of abuse or neglect of the child and, upon request, shall make available to the child protective services coordinator and the local department that is the agency of jurisdiction any information, records, or reports that document the basis for the report.” Reporting and PHI in Virginia Source: http://leg1.state.va.us
- 31. • Police • Child Protective Services (DFS) • FACT/Child Abuse-SANE? • ED Social Worker • Child Life Services (they can assist with comfort) • Advise your charge nurse and other caregivers as warranted Who are you going to call?
- 34. • Think First… • Remember: –ABCDE… –Safe the life –Ask: “What’s not right with this?” –Preserve and Report Case Scenario
- 35. Case Scenario #2 • EMS Report – Code Blue – 64y/o Female impaled knife near xyphoid unknown depth – Found by neighbor who hadn’t seen her in weeks – Labored breathing, lungs CTA, abd soft – VS: HR 158, BP 79/36, RR 32 – Pt refused to leave the house until her son came home and said it was OK, till she became unresponsive – GCS now 5 (E1, V1, M3), EMS working to intubate Copyright © NSW Institute of Trauma & Injury Management 2010
- 36. Case Scenario #2 • EMS Report – Code Blue – 64y/o Female impaled knife near xyphoid unknown depth – Found by neighbor who hadn’t seen her in weeks – Labored breathing, lungs CTA, abd soft – VS: HR 158, BP 79/36, RR 32 – Pt refused to leave the house until her son came home and said it was OK, till she became unresponsive – GCS now 5 (E1, V1, M3), EMS working to intubate Copyright © NSW Institute of Trauma & Injury Management 2010 Lacking a detailed story, what doesn’t make sense about this patient case?
- 37. Discussion – Clues to Consider? • EMS Report – Code Blue – 64y/o Female impaled knife near xyphoid unknown depth – Found by neighbor who hadn’t seen her in weeks – Labored breathing, lungs CTA, abd soft – VS: HR 158, BP 79/36, RR 32 – Pt refused to leave the house until her son came home and said it was OK, till she became unresponsive – GCS now 5 (E1, V1, M3), EMS working to intubate Copyright © NSW Institute of Trauma & Injury Management 2010 What would you do for this patient in the Trauma Bay? What issues should you consider?
- 38. National Data Statics Elder Abuse and Neglect
- 39. Elder abuse reports on the rise Source: National Center for Elder Abuse
- 40. Elder woman are the center of abuse Source: National Center for Elder Abuse
- 41. • Healthcare workers are the largest reporting group, yet many go unreported, especially “self neglect” cases Healthcare workers are the largest reporting population Source: National Center for Elder Abuse
- 42. • Average Age - 77 – The median age of elder abuse victims was 77.9 – The median age of self-neglecting elders was 77.4 • 66.4% of abused elders are white – 66.4% were White – 18.7% were Black – 10.4% Hispanic – <1% Native Americans and Asian American/Pacific Islander Age and Race of Elder Victims (1996 data)
- 43. • It is estimated that for every one case of elder abuse, neglect, exploitation, or self neglect reported to authorities, about five more go unreported. – National Elder Abuse Incidence Study. 1998. Washington, DC: National Center on Elder Abuse at American Public Human Services Association. • Current estimates put the overall reporting of financial exploitation at only 1 in 25 cases, suggesting that there may be at least 5 million financial abuse victims each year. – Wasik, John F. 2000. “The Fleecing of America’s Elderly,” Consumers Digest, March/April. Total Elder Abuse/Neglect Cases
- 44. •This act revised the “Mandated reporters” list to include dentists, pharmacists, certified emergency medical services personnel, guardians and conservators •The Act always included physicians, nurses, mental health professionals, social workers, and law enforcement officers. Virginia Adult Protective Services Act of 2004 http://www.dss.virginia.gov
- 45. • Police • Adult Protective Services (DFS) • FACT/DV (Domestic Violence) - SANE • ED Social Worker • Geriatric Care Nurse (they can assist with comfort) • Advise your charge nurse and other caregivers as warranted Who are you going to call?
- 48. • Think First… • Remember: –ABCDE… –Safe the life –Ask: “What’s not right with this?” –Preserve and Report Case Scenario
- 49. Case Scenario #3 • EMS Report – No Trauma Code – 34y/o male reports being assaulted, will not disclose further details, nobody in custody – “Blood is everywhere” unable to determine exact location of injuries (if any), pt has moved from initial location so UTA total blood loss, not actively bleeding from anywhere – VS: HR 128, BP 155/90, RR 22, PERRLA GCS 13-14 – Pt wants to AMA, but Police have “encouraged” pt come for evaluation www.dailymail.co.uk
- 50. Case Scenario #3 • EMS Report – No Trauma Code – 34y/o male reports being assaulted, will not disclose further details, nobody in custody – “Blood is everywhere” unable to determine exact location of injuries (if any), pt has moved from initial location so UTD total blood loss, not actively bleeding from anywhere – VS: HR 128, BP 155/90, RR 22, PERRLA GCS 13-14 – Pt wants to AMA, but Police have “encouraged” pt come for evaluation www.dailymail.co.uk Lacking a detailed story, what doesn’t make sense about this patient case?
- 51. • Findings in room 12 – Airway and breathing are good. Pt is oriented to person and place but confused – Blood is everywhere but no active bleeding noted until you get to “E” and Expose • You note significant trauma to the rectum, groin and lower back – Bleeding limited at this time – VS remain stable Case Scenario #3 Medscape.com www.dailymail.co.uk
- 52. • Findings in room 12 – Airway and breathing are good. Pt is oriented to person and place but confused – Blood is everywhere but no active bleeding noted until you get to “E” and expose • You note significant trauma to the rectum, groin and lower back – Bleeding limited at this time – VS remain stable Case Scenario #3 Medscape.com www.dailymail.co.uk Not knowing all the facts, what are you immediate actions? What are your follow-up actions related to the possible criminal aspects?
- 54. • As few as 5% of domestic violence victims are identified as such in Emergency Department records. – American Journal of Public Health, 1989 • Nearly one-third of American women (31 percent) report being physically or sexually abused by a husband or boyfriend at some point in their lives. – Bureau of Justice Statistics Crime Data Brief: Intimate Partner Violence, 1993-2001, (2003) Domestic Violence data
- 55. • Intimate partner violence made up 20% of all nonfatal violent crime experienced by women in 2001. – The risk of injury increases among female rape and physical assault victims when their assailant is a current or former intimate partner • Intimate partners committed 3% of the nonfatal violence against men in 2001 Domestic Violence data Source: Bureau of Justice Statistics Crime Data Brief: Intimate Partner Violence, 1993-2001, at 1 (2003) Source: www.ncjrs.gov
- 56. • The prevalence of domestic violence among Gay and Lesbian couples is approximately 25 - 33%. • Seven states define domestic violence in a way that specifically excludes same-sex victims. • States with sodomy laws (e.g. Virginia) essentially require same-sex victims to confess to a crime in order to prove they are in a domestic relationship. – Virginia’s laws can conflict with each other, offering unclear legal determination. Actions and prosecutions vary by local jurisdiction. Domestic Violence data Source: Barnes, It's Just a Quarrel', American Bar Association Journal, February 1998
- 57. • One in three teenagers has experienced violence in a dating relationship • 15 percent of teen girls and boys have reported being victims of severe dating violence (defined as being hit, thrown down, or attacked with a weapon). • 8 percent of 8th and 9th grade students have reported being victims of sexual dating violence. Domestic Violence data Source: National Center for Victims of Crime
- 58. • Virginia law requires that if law enforcement has probable cause to believe that a domestic assault has occurred (this usually means they are able to see scratches, bruises, or other injuries with their own eyes), they must arrest the “predominant physical aggressor” unless special circumstances exist which would dictate some other course of action – VA Code 19.2-81.3 • Healthcare workers are required to report under the laws for Child and Adult abuse, as well as under the requirements of knowledge of a violent crime taking place, but there is no direct law requiring reporting of domestic abuse Domestic Violence Laws
- 59. • Fairfax Police • FACT/SANE – Sexual • ED Social Worker • Advise your charge nurse and other caregivers as warranted • Refer the possible victim to: Virginia Family Violence/Sexual Assault Hotline - (800) 838-8238 Who are you going to call?
- 61. Discussion: Clues to Consider in theTrauma • What would you consider are your priorities in a Trauma Resuscitation with any abuse or neglect patient? – Does this differ from any victim of violence or neglect? • How would you communicate with family in case of suspicion? • What ancillary services might you involve? • What discussion would you have with the rest of the
- 62. Who can you call if the event you’ve seen or participated in is too much for you, or you just want to talk? •Your Peers •ED Social Worker •EAP – 24/7/365 What if it’s too much for you
- 63. Conclusions • Remember your ABCDEs always come first. • Think about what else could be going on. • Consider the need to report suspicion – not the need to know for sure. • Utilize the vast resources IFH and the community offers to manage these cases. • Seek the support of your peers and other professionals.
- 64. THE END
Editor's Notes
- Instructor Notes: Use the instructor notes on each slide to better lead you through the presentation. TIP: There’s a lot of data in the presentation sections where there is “national data” which may be of interest to the students. The goal is to only present the highlighted “blue” sections, try not to bother with the black sections on those slides, let the students know this is additional reference material
- Make sure people know this presentation can be impactful and graphic
- If they are uncomfortable with the material they are welcome to step out for a bit
- Discuss course objectives Our Purpose here is not to teach the finer details of abuse, neglect etc.. As an experienced ER Nurse you should already know about these variables. Our focus is really to prime your thoughts on how to recognize and deal with an abuse/violence patient in the trauma bay.
- Pop Quiz: This builds the questions, then when you press Enter or Pg Down you get the answer. The focus is to help them realize that ABC’s are the priority… always
- Point out that there are 4 basic types of abuse (according to law). We will not isolate each one, in this lecture, but focus on the mechanism and how to manage the situation in the trauma bay
- Focus on the aspect that abuse is defined as “any recent act or failure to act which results in death, serious physical or emotional harm, sexual abuse of exploitation, or an act or failure to act – which presents an IMMINENT RISK OF SERIOUS HARM
- 3 types of elder abuse based on the law: Domestic – At the home Institutional – at a SNF, etc. Self neglect or abuse – for example, Self Neglect would be something like, the elderly person who stops taking their HTN meds, so they can pay for something else.
- Focus on: The willful intimidation, assault, battery, sexual assault or other abusive behavior perpetrated by one family member, household member, or intimate partner against another.
- ASK THE QUESTIONS: Is this Safe? What’s more important? Asking why the child was here or dealing with the IMMEDITATE LIFE RISK? (answer is obviously YOUR personal safety and then the immediate life risk)
- Evidence preservation is important but should never take a back seat to saving a life. IF you have time, “consider” evidence preservation. Considering doesn’t mean you do it… you can consider it and then opt that the pt’s condition is resources are such that you don’t have the ability to worry about this now. Review the bullets with the class
- More bullets to review Make sure that the students understand that PHI (Protected Health Information) is still a part of the puzzle UNTIL either the victim releases that or a subpoena has been issued by the PD. In either case it’s not our role to deal with this, that is per policy something for medical records to deal with . We do not give out medical information as a practice in the ED
- Rarely do the hands “need” to be bagged, but on occasion they will, just make sure it doesn’t impede care Also note that if you need to clean the patient, you are potentially also cleaning off evidence (e.g. DNA if doing a foley). Again while patient care is the primary goal, you must “consider” the evidence preservation. So if you’re doing a foley, only clean what you must clean to reduce infection risk (as an example) Note that: Part of the Trauma fellowship includes a great lecture of Forensics and more will be covered in that lecture
- Intro: Child Abuse/Neglect
- THINK FIRST! Focus on ABCDE (think TNCC etc) SAVE A LIFE FIRST – then look at legal issues
- Present this like a Comm Report.
- So Ask the group: What’s wrong, what doesn’t make sense to you in this report The key is it’s vague on purpose… a lot of this stuff could go either way: Ask the students: does it make sense… maybe it does, maybe it doesn’t that’s the point… get them thinking and talking about it Would an 8 year old fall down an entire flight of stairs? Developmentally where are they? Maybe they fell, maybe they jumped and fell.. Or maybe they were “helped”
- Does a buttock and forearm injury make sense with a fall down the stars? Yes/no/maybe?
- Would an 8 year old be calm if they are stripped down into nothing on a board with a bunch of people around? Would an 8 year old boy rather have Mom or Dad?
- What’s not right?
- Multiple head contusions.. Might make sense But… Circumferential contusion – of varied ages on BOTH wrists… does this make sense with the mechanism? Contusions to the anterior/superior chest wall (see the 2nd picture down from the right… that looks like fingers pointing on opposite side of sternum) – how could those have come from a fall? Contusions – multi layer on buttock, certainly mutli layer in age indicated prior injuries
- Discuss what you did with this patient in the trauma bay (stay very high level) What would you consider about rectal tone? – would you potentially destroy evidence? – is there another way to check Neuro with doing a rectal? – “clench buttock” What about emotional support? – Child Life services? What about reporting this?
- Lots of data on the follow pages… don’t read all of it, hit the highlights… focus on the blue statements, and move on. If someone has a question focus on the question. Let them know the rest is there for their reference to read at their leisure
- Lots of data on the follow pages… don’t read all of it, hit the highlights… focus on the blue statements, and move on. If someone has a question focus on the question. Let them know the rest is there for their reference to read at their leisure
- Lots of data on the follow pages… don’t read all of it, hit the highlights… focus on the blue statements, and move on. If someone has a question focus on the question. Let them know the rest is there for their reference to read at their leisure
- Lots of data on the follow pages… don’t read all of it, hit the highlights… focus on the blue statements, and move on. If someone has a question focus on the question. Let them know the rest is there for their reference to read at their leisure Some additional points Healthcare workers are ONLY required to report in their line of duty. So if you’re at home and see something, you don’t have to report (morale issues aside You don’t need to prove anything or have any evidence, only the suspicion or a concern of If it’s immediate risk get PD involved NOW
- Lots of data on the follow pages… don’t read all of it, hit the highlights… focus on the blue statements, and move on. If someone has a question focus on the question. Let them know the rest is there for their reference to read at their leisure More info: You can’t be sued if you report – the family can’t take any action against the reporting party You don’t have to (and probably shouldn’t) tell the family of your reporting effort Focus on the law that requires reporting in 72 hours for a moment
- Lots of data on the follow pages… don’t read all of it, hit the highlights… focus on the blue statements, and move on. If someone has a question focus on the question. Let them know the rest is there for their reference to read at their leisure More: I included the full text of the code here since it’s confusing. Short answer is focus on the blue paragraph – Some spiritual needs are not what we as healthcare workers thinks are right, but they are not abuse or neglect. If you’re worried – consult CPS
- Lots of data on the follow pages… don’t read all of it, hit the highlights… focus on the blue statements, and move on. If someone has a question focus on the question. Let them know the rest is there for their reference to read at their leisure PHI is Protected Health Information – short answer there is no HIPAA issue here at all
- When in question call the PD – especially if there is risk of immediate danger to the pt or siblings When in question a great IFH resource is our FACT team… call them 24/7 when you need insight
- THINK FIRST! Focus on ABCDE (think TNCC etc) SAVE A LIFE FIRST – then look at legal issues
- Read this like it’s a report from comm:
- Point out not only that they are unstable but also: Pt refused to leave the house until her son came home and said it was OK, till she became unresponsive Does this sound uncharacteristic?
- Make sure you ask what would you do for the pt? What you should hear is ABCDE Consider evidence (but don’t get in the way of pt care) Know that PD will be there Consider detailed documentation, this will be in court at some time (probably)
- Each year we’re seeing an increase in numbers, some would argue because of an actual increase vs awareness and reporting or increase in elderly population
- Focus on blue lines only – the rest is reference
- Focus on blue lines only – the rest is reference
- The act of 2004 updated the older act and added to the list to more professionals that are required by law to report
- Again the IFH FACT team is a great resource 24/7
- THINK FIRST! Focus on ABCDE (think TNCC etc) SAVE A LIFE FIRST – then look at legal issues
- Read this like a Comm report
- Discuss: Other than the blood everywhere and a little bit of an excited BP there are no outward findings.. Due to the situation and confusion, EMS did not expose the pt Consider the total picture that “everything is unclear” and we don’t really know what to expect What doesn’t make sense?
- Discuss: Trauma’s can be anywhere so keep the same rules of the trauma bay in mind when in a regular pt room See the importance of “E”
- Based on this highlighted finding, what are you considering? Answers should include: ABCDE If stable and able consider evidence
- Focus on the blue highlighted facts
- Focus on the blue highlighted facts
- GLT violence is on the rise Points to consider: Virginia is a state that has a Sodomy law Keep in mind that sodomy is essentially a legal term these days, meaning Oral or Anal Sex with same of opposite gender. So the catch 22 here is that a same sex couple has to confess to one crime (sodomy – but consensual) to claim they are a same sex partner and in the past they have had a sexual relation… but this time it wasn’t. The good news is according to the Prosecutors in this area, they tend to overlook the Sodomy laws to protect the victim. That is however in the NoVA jurisdictions others may not be so lucky.
- Focus on the blue points
- Focus on blue points If short on time biggest point is 2nd bullet that there is no law directly requiring the reporting of domestic abuse but healthcare workers. – No legal obligation to act
