Septic shock
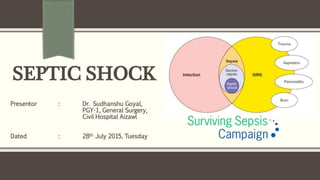
- 1. SEPTIC SHOCK Presentor : Dr. Sudhanshu Goyal, PGY-1, General Surgery, Civil Hospital Aizawl Dated : 28th July 2015, Tuesday
- 2. What is SEPTIC SHOCK? Invasion of normally sterile host tissue by microorganism Inflammatory response to the presence of microorganism Infection Two or more of following Hyothermia or hyperthermia Tachycardia Tachypnoea or Paco2 <32 mmHg Leucocytosis or leucopenia SIRS SIRS Plus Documented Infection Sepsis Sepsis + Organ dysfunction Plus Hypotension Steptic Shock
- 3. Pathophysiology of Septic Shock
- 4. Clinical Presentation Symptoms Fever: insensitive indicator Hypothermia: more predictive of severity and death Confusion/Disorientation: metabolic encephalopathy ?altered a.a. metabolism Hyperventilation: stimulation of respiratoty centres by inflammatory mediators Organ system localizing symptoms Signs Rectal temperature Extremities: Warm vs Cold shock Tachycardia and Pulse pressure Tachypnoea Altered mental status Organ system localizing signs
- 5. Workup CBC with DLC Coagulation studies : PT & aPTT and fibrin split products elevated with fibrin levels decreased in DIC Biochemical tests: Lactate levels Serum Electrolytes KFT LFT Microbiology: SSC recommends atleast 2 blood cultures before antibiotics One percutaneous Other(s) through each vascular access (if >48hrs) Urine RME and Culture Gram stain and culture of secretions and tissues (at least 1ml/gm)
- 6. Workup continued… Imaging Chest radiograph is warranted in every case Abdomen CT is preferred over radiography USG if suspected Gall bladder pathology Extremities radiograph if suspected lesion Lumbar puncture Suspected meningitis or encephalitis
- 8. Management Principles Early recognition Early and adequate antibiotic therapy Source control Early hemodynamic resuscitation and continued support Proper ventilator management with low tidal volume in patients with acute respiratory distress syndrome (ARDS)
- 9. General Management 2 large bore IV lines for aggressive fluid resuscitation and antibiotics Central venous access is useful but not mandatory Urinary catheterization to monitor UOP All cases of sepsis should be given oxygen Intubation in cases of respiratory distress due to DAD and ALI Patients who do not respond to initial fluid resuscitation needs ICU admission
- 10. Specific Management ProCESS, ARISE and ProMISe trials have concluded that Measuring lactate, targeting ScvO2 values and insertion of central venous catheter, no improved outcomes Direct and individualized care Culture and early institution of broad spectrum antibiotics Restoration of BP Reversal of evidence of end organ perfusion
- 11. Fluid Resuscitation Challenge with 1-2 L (30mL/kg) of crystalloids within 30-60 mins Continue as long as improvement continues End points: signs of volume overload sustained rise of >5mm Hg in cardiac filling pressure Rapid increase of CVP by >2 mm Hg Absolute CVP > 8-12 mm Hg Crystalloids versus Colloids SAFE trial, no significant difference Trend towards better outcome with 4% albumin NS versus LR Randomized double blinded trials LR has less chances hyperkalaemia and acidosis Mortality was higher in the saline group
- 12. Vasopressor Therapy When to start: no response with ≥4 L of crystalloid if evidence of fluid overload persistent hypotension First line therapy: DOPAMINE vs NORADRENALINE Noradrenaline Potent α agonist with minimal β agonist activity 5-20 mcg/min irrespective of weight Dopamine 30% patients fail to reach target MAP “No beneficial effect on renal blood flow and function in setting of circulatory shock of any etiology” Useful in cold shock with co-existent bradycardia Dose: begin with 5-10 mcg/kg/min upto 20 mcg/kg/min
- 13. Vasopressor Therapy continued… Second line agents: If poor clinical response to first line agents Adrenaline Increase Cardiac Index and Stroke Volume as well as HR and SVR Increase oxygen delivery and consumption Vasopressin Reserved for salvage therapy VASS Trial, decrease requirement of catecholamines but no significant effect on mortality Dose: 0.03 U/min Phenylephrine Rarely used If tachyarrythmias limit therapy with other agents
- 14. Ionotrope therapy Useful if inadequate: Cardia Index MAP SmvO2 Despite adequate volume resuscitation and vasopressor therapy Dobutamine β receptor mediated increase in CO If myocardial dysfunction or hypoperfusion in presence of adequate fluid resuscitation and adequate MAP Dose: Upto 20 mcg/kg/min
- 15. Corticosteroids CORTICUS study, patients who received hydrocortisone had rapid resolution of shock and faster improvement of organ dysfunction Higher incidence of recurrent sepsis and super-infections Recommendations (ACCCM) In patients with septic shock administer Hydrocortisone 200mg/day in 4 divided doses or 100mg bolus f/b 10mg/hr for 7 or more days In patients with early severe ARDS Methylprednisolone 1mg/kg/day continuous infusion for 14 or more days Do not use dexamethasone Weaning when vasopressor is not needed Steroids not to be used in absence of shock
- 16. Antibiotic therapy Broadspectrum empiric antibiotic therapy within 1 hr of recognition Use of 1 or more agents active against presumed source of infection plus capable of penetration in adequate concentrations Daily re-evaluation for potential de-escalation Combination empiric therapy if: Difficult to treat multidrug resistant organism (eg pseudomonas) Severe infections associated with respiratory failure and septic shock Septic shock and bacteremia from pneumocci Combination therapy to be limited to 3-5 days, switch to monotherapy based on culture and sensitivity results
- 17. Antibiotic Selection Must cover Gram positive, gram negative and anaerobic bacteria If antibiotic experienced Aminoglycoside over quinolone or cephalosporine for gram negative For covering MRSA Vancomycin or linezolid to be used For ESBL producing organisms Cephamycins (eg cefotetan) and carbapenems (eg imipenem, meropenem and ertapenem) In immunicompetent adequate coverage is offered by Carbapenems (eg imipenem and meropenem) 3rd and 4th generation cephalosporins (eg cefotaxime, cefoperazone, ceftazidime and cefepime) Extended spectrum penecillins (eg ticarcillin and piperacillin) No need for Nephrotoxic aminoglycoside
- 18. Glycemic Control Based on NICE-SUGAR trials, SSC Guidelines suggest: Target blood glucose level is < 180 mg/dL Start insulin if 2 consecutive blood glucose levels are >180 mg/dL Monitor 1-2 hrly if stable 4 hrly Capillary blood to be interpreted catiously
- 19. Blood Products Hemoglobin If Hb < 7g/dL transfusion is recommended Target Hb 7-9 g/dL No role of erythropoietin Platelet transfusion if < 10,000 < 20,000 and risk of bleeding < 50,000 if surgery or invasive procedures are planned FFP Not recommended for lab clotting abnormalities Only if planned for surgery or invasive procedures
- 20. Metabolic and Nutritional Support K, Mg and PO4 levels should be measured and corrected High protein and energy requirement state Early nutritional support with preferred oral/enteral route Gastroperesis can be treated with motility agents or small bowel feeding tube Advantages of enteral route Protection of gut mucosa Prevention of translocation of organisms from GIT Reduced complication Low cost
- 21. Mechanical Ventilation Lung protective and pressure-limited ventilation TV of 5-8 ml/kg, transpulmonary pressure not more than 30 cm of H2O Permissive hypercapnea PEEP to prevent alveolar collapse Prone position ventilation
- 22. DVT prophylaxis Low dose unfractionated heparin 2-3 times a day Low molecular weight heparin in high risk patients (eg severe sepsis and previous DVT, trauma or orthopedic surgery) If creatinine clearance < 30 mL/min use deltaparin Use mechanical DVT prevention devices in presence of CI
- 23. Other measures Renal replacement Intermittent hemodialysis and continuous venovenous hemofiltration are equivalent CVVH is better for hemodynamically unstable patient Sedation and NMB Use intermittent bolus sedation or continuous infusion sedation Daily lightening to produce awakening Avoid NMB where possible Use of bicarbonate is not recommended Stress ulcer prophylaxis PPI or H2 blocker Prone position ventilation
- 24. Sepsis at its Inception is Difficult to Recognize but Easy to Treat Left Unattended it becomes Easy to Recognize but Difficult to Treat
