Infectious agents of bioterrorism handout
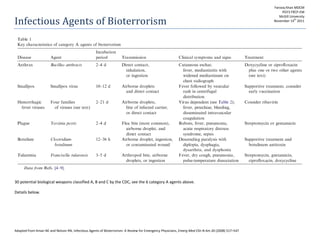
- 1. Adapted from Kman NE and Nelson RN, Infectious Agents of Bioterrorism: A Review for Emergency Physicians, Emerg Med Clin N Am 26 (2008) 517–547 Infectious Agents of Bioterrorism 30 potential biological weapons classified A, B and C by the CDC, see the 6 category A agents above. Details below. Farooq Khan MDCM PGY3 FRCP-EM McGill University November 14 th 2011
- 2. Adapted from Kman NE and Nelson RN, Infectious Agents of Bioterrorism: A Review for Emergency Physicians, Emerg Med Clin N Am 26 (2008) 517–547 Anthrax Time dependent therapy: mortality doubles if time to diagnosis goes from 2 to 4.8 days. Potential for meningitis in all types. Cutaneous: Contact with contaminated hides of goats/sheep/cows that ingest spores through soil, 2000 cases worldwide Spores in skin incubate for 5 days [1-12 days], then germinate causing edema and eventually painless black eschar ×2 weeks with lymphadenopathy/edema Eschars Ddx: tularemia, scrub typhus, rickettsial spotted fevers, rat bite fever, arachnid bites, vasculitides, and ecthyma gangrenosum Low mortality GI: least common, ingestion of contaminated undercooked meat. Oral-pharyngeal anthrax causes lip, oral, or esophageal ulcers and leads to lymphadenopathy, edema, and sepsis Anthrax infection of the lower GI tract can present with nausea, vomiting, malaise, or bloody diarrhea. Infection can ultimately lead to ascites, acute abdomen, or fulminant sepsis. Pulmonary: Wool sorters disease, ↑bioterrorism potential spores are inhaled and deposited on the alveolar surface where they are phagocytosed by macrophages. Surviving spores are transported to mediastinal lymph nodes where they germinate (2-43 days) The bacteria multiply and produce exotoxins that quickly cause mediastinal edema and necrosis followed by bacteremia, toxemia, sepsis, and death. first symptoms of inhalational anthrax are nonspecific fever, dyspnea, cough, headache, chills, vomiting, weakness, or chest pain, may have tachycardia and hypoxemia N°/v°, pallor/cyanosis, diaphoresis, AMS, HR > 110 beats/min, temp > 100.9°F, and ↑Hct all predict inhalational anthrax over similar diseases Diagnosis Aerobic blood culture of gram+ bacilli, ↑liver enzymes, CXR showing infiltrates with mediastinal widening and pleural effusions, CT chest, clinical mediastinitis Treatment Cutaneous: oral cipro/doxy ×60 days Inhalational: cipro/doxy + vanco/clinda/rifampin/clarithromycin/imipenem ×60 days (IV in limited casualty, PO in mass casualty) Steroids for pulmonary edema, resp failure and meningitis (use cipro + chloramphenicol/rifampin/pen for better CNS penetration)
- 3. Adapted from Kman NE and Nelson RN, Infectious Agents of Bioterrorism: A Review for Emergency Physicians, Emerg Med Clin N Am 26 (2008) 517–547 Public health concerns Vaccine for at risk workers (6 doses over 18 months) PEP: 60 days cipro/doxy vs 100 days +/- 3 doses of vaccine Standard universal precautions, no respiratory isolation needed Contaminated surfaces can be cleaned with sodium hypochlorite (extreme cases biocidal gases or radiation are needed to kill resistant spores) Smallpox Variola minor and major (fatality rate of 30% in epidemics) eradicated by vaccine programs in 1977. Vaccination ended in 1980. Stockpiled at CDC in Atlanta and institutes of virus preparation in Moscow. Potential for bioterrorism Droplet and contact transmission. Highly contagious (1 index case→10-20 secondary cases) Incubation: Enters body through oral nasal mucosa, travels to regional LN, replicates then seeds to the skin and all organs. asymptomatic (10-15 days) Prodromal: after 8 days, secondary replication in bone marrow and spleen: high fever, toxemia, malaise, vomiting, headache, backache, and myalgias. (3 days) Fulminant: Rash for 7-10 days, most infectious. Later wanes but Infectivity can remain even after death. Enanthem: erythematous papules and erosions. Exanthem: raised indurated erythematous macules → firm pearly umbilicated vesicles → pustular confluent → thick crusting scabs with scars. Centrifugal from face down, legs and abdomen affected last, palms/soles spared All in similar stages of development Complications Panophthalmitis, blindness, keratitis, corneal ulcers, osteomyelitis, arthritis, orchitis, and encephalitis Death most commonly occurs from bronchitis, pneumonitis, pulmonary edema, associated bacterial pneumonia, and sepsis Diagnosis: clinical suspicion, number of cases. Rare occurrence of hemorrhagic (meningococcemia-like illness) or malignant (rapid fulminant onset) variants. Index case should be confirmed by electron microscopy in level 4 biosafety lab, further diagnosis is clinical. Treatment: Supportive only. No recommended antivirals Public Health concerns : Outbreak →Vaccine (ACAM2000) for all hospital employees and other high risk groups, designated hospital, negative pressure isolation, aggressive linen/surface decon (virus can live 24h). Home quarantine, vaccination of patients within 4 days of exposure reduces fatal outcome.
- 4. Adapted from Kman NE and Nelson RN, Infectious Agents of Bioterrorism: A Review for Emergency Physicians, Emerg Med Clin N Am 26 (2008) 517–547 Hemorrhagic fever viruses Transmission: fine droplet aerosol Direct contact with blood, tissue or secretions of infected patients/animals/dead bodies. Can be inhaled aerosols in animal feces or urine, or contaminated food. Can be mosquito bite Needlestick injuries are almost always fatal.
- 5. Adapted from Kman NE and Nelson RN, Infectious Agents of Bioterrorism: A Review for Emergency Physicians, Emerg Med Clin N Am 26 (2008) 517–547 Transmission rarely occurs before onset of symptoms Airborne is less common Clinical. Virus attacks vascular system leading to ↑permeability and hemorrhaging See table for prodromes and clinical patterns When the bleeding occurs, it may manifest as petechiae, mucous membrane or conjunctival hemorrhage, hematuria, hematemesis, or melena. Disease progression can lead to DIC, hypotension, and circulatory shock. Signs of CNS dysfunction, such as delirium, seizures, or coma → poor prognosis Complications: virus dependent Ebola/marburg mortality within 6-9 days rift valley and yellow fever: jaundice rift valley and lassa fever: less hemorrhagic complications Death from viral hemorrhagic fever is preceded by hemorrhagic diathesis, shock, sepsis, or multisystem organ failure. Patients who survive this disease may be left with hearing or vision loss, impaired motor coordination, transverse myelitis, uveitis, pericarditis, orchitis, parotitis, hepatitis, or pancreatitis Ddx: Influenza, viral hepatitis, staphylococcal or gram-negative sepsis, meningococcemia, salmonellosis, shigellosis, malaria, dengue, rickettsial diseases, and Hantavirus. Non infectious: DIC, ITP/TTP, HUS, Stevens-Johnson syndrome, acute leukemia, and collagen vascular diseases Diagnosis: clincial suspicion, travel, number of patients WHO surveillance standards: Fever >38.3° <3 weeks duration ≥2 Hemorrhagic symptoms: hemorrhagic or purple rash, epistaxis, hematemesis, hemoptysis, blood in stools No alternate Dx CBC, liver enzymes, coags, fibrin slplit products, firbinogen. Sample sent to biosafety level 4 facility. Treatment: aggressive support +/- ribavirin × loading dose of 30 mg/kg IV, then 16 mg/kg IV q6h ×4 days, then 8 mg/kg IV q8h ×6 days, or in outbreaks: 2000 mg po ×1, then 1200 mg/d po divided bid ×10 days Public health concern: strict isolation, surveillance of contacts over 21 days period and subsequent isolation if symptomatic . outbreak over after 2 consecutive incubation periods (i.e. 42 days) if no additional cases
- 6. Adapted from Kman NE and Nelson RN, Infectious Agents of Bioterrorism: A Review for Emergency Physicians, Emerg Med Clin N Am 26 (2008) 517–547 Strict barrier protection, hand hygiene, double glove, impermeable gowns, N95 mask/air purifying respirators, negative pressure isolation rooms, leg and shoe coverings, face shields and eye protection, restricted access to all nonessential staff, dedicated disposable (or single use) medical equipment, and EPA-approved disinfectant. Community health education: Radio broadcasts, Churches, schools, military units, and markets informed, Contact tracing, clinical management, infection control in health facilities, and rapid on-site laboratory diagnosis. No vaccines for most, except rift valley but not available in sufficient quantities Plague Yersinia Pestis, gram– coccbacillus, rare naturally occurring cases mostly bubonic, 2% pneumonic Animal reservoir in rodents, lagomorphs and cats, flea vector Person to person transmission via contact with infected tissues, body fluids, respiratory droplets Natural epidemics are more bubonic with preceding rodent deaths. Bioweapon to consider if non endemic population has pneumonic plague and no animal deaths Clinical Bubonic: flea bite→infection of local LN (2-8 dayslater )→ fever chills weakness → formation of buboes (1-10 cm, extremely painful, erythematous, and associated with surrounding edema and warmth) at LN in groin/axilla/cervical region due to resistance of bacteria to destruction (1 days later) → Necrosis of buboe causing pneumonia, bacteremia , and sepsis, with DIC, necrosis of small vessels, purpuric skin leasions and gangrene Primary pneumonic : 2 -4 days sudden onset of a productive cough, chills, headache, body aches, and dyspnea, nausea, vomiting, abdominal pain, and diarrhea Diagnosis: Clincial suspicion Outbreak/terrorism: large number of previously healthy patients presenting with fever, cough, tachypnea, dyspnea, chest pain, pneumonia, and a fulminant course leading to sepsis or death. It is unlikely these patients would present with buboes CXR: bilateral infiltrates or consolidation Antigen detection, IgM enzyme immunoassay, immunostaining, and PCR are available on a limited basis Leukocytosis with toxic granulations, coagulation abnormalities, aminotransferase elevations, azotemia, and other evidence of multiorgan failure Gram stain of sputum or blood may reveal gram-negative bacilli or coccobacilli. A Wright, Giemsa, or Wayson stain may show bipolar staining Cultures of blood, sputum, or bubo aspirate should demonstrate growth in 24 to 48 hours. Cultures sent out are confirmed in specialty laboratories by immunostaining and immunoassay Treatment Do not delay >24h, or mortality↑
- 7. Adapted from Kman NE and Nelson RN, Infectious Agents of Bioterrorism: A Review for Emergency Physicians, Emerg Med Clin N Am 26 (2008) 517–547 Fluid resuscitation, pressors, monitoring mechianical ventilation IV/IM streptomycin × 10 days, or genta in contained casualty Mass casualty cipro or doxy po Public health concern Isolate droplet precaution In outbreak, all patients with temp >38.5°C or a new cough should start Abx HCW and Asymptomatic close contacts of pneumonic plague patients should take PEP of doxy ×7 days (if refusing meds should be obersved ×7 days) Vaccine not effective against pneumonic plaqgue Botulinum toxin (see chemical terrorism antidotes update handout) Clinical diagnosis (1) symmetric, descending flaccid paralysis with prominent bulbar palsies in (2) an afebrile patient with (3) a clear sensorium. The bulbar palsies can be summarized as the ‘‘4 D’s’’: diplopia, dysphagia, dysarthria, and dysphonia. Tests not helpful to rule in, can be used to rule out other causes Ddx: GBS, myasthenia, stroke, tick paralysis Treatment: supportive, mechanical ventilation and antitoxin (see chemical terrorism antidotes update handout) Public Health concerns: proper food storage and consumption, surveillance for contaminated food. Standard precautions handwashing Tularemia bacterial zoonosis caused by Francisella tularensis, extremely hardy aerobic, intracellular, gram-negative coccobacillus that can survive for weeks in water, soil, animal carcasses, hides, frozen meat, and hay or straw. Natural transmission through insect (tick) bite, no person to person, weaponized form is inhaled Clinical:
- 8. Adapted from Kman NE and Nelson RN, Infectious Agents of Bioterrorism: A Review for Emergency Physicians, Emerg Med Clin N Am 26 (2008) 517–547 Incubation 3-5d, abrupt onset of fever, chills, headache, coryza, sore throat, myalgia, arthralgia, and fatigue Severity, type of symptoms, and time to onset depend on route, dose, and virulence of organism 6 clinical syndromes: Can overlap Ulceroglandular: 75% to 85%. bite→papule→ulcer→eschar. Regional LN → bacteremia Glandular: 5-10%m fever and tender lymphadenopathy with no evidence of cutaneous involvement Oculoglandular: 1-2% after inoculation of the eye with contaminated fingers or with accidental inoculation with infected matter. Painful purulent unilateral conjunctivitis with cervical and preauricular LN Oropharyngeal: acquired by drinking contaminated water, eating contaminated food or undercooked meat, and, less commonly, by inhaling infectious droplets, pharyngitis, tonsillitis, or stomatitis with cervical LN. They may also manifest GI symptoms of abdo pain, na°, v°, d°, intestinal ulcerations, GI bleeding, and mesenteric LN Typhoidal: rare, severe, systemic symptoms without skin, mucosal, or lymphatic involvement, → SIRS, sepsis, DIC, ARDS, multisystem organ failure Pneumonic: atypical pneumonias, fever and non-productive cough, dyspnea, and pleuritic chest pain. Likely in terrorist attack. Complications : may spread hematogenously to cause meningitis, pericarditis, pneumonia, hepatitis, peritonitis, endocarditis, ataxia, osteomyelitis, sepsis, rhabdomyolitis, and acute renal failure Diagnosis: clinical, labs non-specific, CXRL pneumonia like +/- pleural effusions, medastinal LN, cavitary lesions. ELISA serologic test positive if 4-fold higher than convalescent titer, or single titer >1:160 Cultures can be grown from pharyngeal washings, sputum specimens, and from blood Antigen detection assays, PCR, EIA, immunoblotting, and electrophoresis are available in research and reference laboratories Treament Isolated cases: streptomycin 1 g IM bid ×10 days/ gentamicin 5 mg/kg IM/IV qd ×10 days Mass casualty: cipro 500mg po bid ×10 days/doxy 100 mg po bid ×10-14 days. Can be used in peds (benefits outweight risks), cipro for pregnancy Public health concern: no human-human spread, caution when handling animals/around insects PEP: 14 days of cipro/doxy within 24h Fever watch for contacts Vaccine only for lab workers Decontamination of exposed surfaces and objects can occur with 10% bleach solution followed in 10 minutes by 70% alcohol solution
